Posthemorrhagic anemia
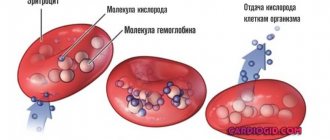
The main factors in the development of posthemorrhagic anemia are the phenomena of vascular insufficiency, hypovolemia with a decrease in the total volume of plasma and circulating formed elements, in particular, red blood cells that transport oxygen. This process is accompanied by a decrease in blood pressure, blood supply to internal organs and tissues, hypoxemia, hypoxia and ischemia, and the development of shock.
The degree of severity of the body's protective and adaptive reactions is determined by the volume, speed and source of bleeding. In the early reflex-vascular phase of compensation for blood loss (the first day), due to the stimulation of the sympathetic-adrenal system, vasoconstriction and increased resistance of peripheral vessels are observed, stabilization of hemodynamics due to the centralization of blood circulation with primary blood supply to the brain and heart, a decrease in the return of blood to the heart and cardiac output. The concentration of red blood cells, Hb and hematocrit are still close to normal (“hidden” anemia).
The second hydremic phase of compensation (2-3 days) is accompanied by autohemodilution - the entry of tissue fluid into the bloodstream and replenishment of plasma volume. Increased secretion of catecholamines and aldosterone by the adrenal glands and vasopressin by the hypothalamus contributes to the stability of the level of electrolytes in the blood plasma. There is a progressive decrease in red blood cells and Hb (total and per unit volume), hematocrit; the value of the color indicator is normal (posthemorrhagic normochromic anemia).
In the third, bone marrow phase of compensation (4-5 days), due to iron deficiency, anemia becomes hypochromic, the formation of erythropoietin by the kidneys increases with activation of the reticuloendothelial system, bone marrow erythropoiesis, and foci of extramedullary hematopoiesis. In the red bone marrow, hyperplasia of the erythroid lineage and an increase in the total number of normocytes are observed, in the peripheral blood there is a significant increase in the number of young forms of erythrocytes (reticulocytes) and leukocytes. Hb, red blood cell and hematocrit levels are decreased. Normalization of the level of red blood cells and Hb in the absence of further blood loss occurs after 2-3 weeks. With massive or prolonged blood loss, posthemorrhagic anemia becomes hyporegenerative in nature, and shock develops when the body's adaptive systems are depleted.
Anemia - symptoms and treatment
Treatment should first of all be aimed at identifying and eliminating the root cause, so therapy for anemia lasts a long time, often accompanied by several medical specialists.
Indication for treatment
The indication for drug treatment is a decrease in hemoglobin levels to less than 120 g/l in women and below 130 g/l in men.
Basically, treatment involves restoring hemoglobin reserves, increasing the number of red blood cells, and normalizing hematocrit. The main effective method of treating iron deficiency anemia is the use of iron supplements orally or parenterally (intravenously or intramuscularly)
To restore the hemoglobin level in a patient with iron deficiency anemia, the dose of ferrous iron per day (only it is effectively absorbed) must be 100-300 mg, taking into account depleted iron reserves (about 1.5 g).
| Drug name | Components included in the drug | Fe dosage, mg | Dosage form of release | Daily dose, g |
| Conferon | succinic acid | 50 | Pills | 3-4 |
| Heferol | Fumaric acid | 100 | Capsules | 1-2 |
| Hemophere prolongatum | Ferrous sulfate | 105 | Dragee | 1-2 |
| Ferrogradumet | Plastic matrix - gradation | 105 | Pills | 1-2 |
| Aktiferrin | D, L-serine | 113,8 34,8 | Capsules Syrup | 1-2 1 teaspoon per 12 kg body weight |
| Ferroplex | Ascorbic acid | 10 | Dragee | 8-10 |
| Sorbifer Durules | Ferrous sulfate + Ascorbic acid | 100 | Pills | 1-2 |
| Tardiferon | Ferrous sulfate + mucoprotease | 80 | Pills | 1-2 |
| Fenyuls | Ascorbic acid, nicotinamide, B vitamins | 50 | Capsules | |
| Irovit | The same + ascorbic acid, cyanocobalamin, L-lysine | 100 | Capsules | 1-2 |
| Irradian | Ascorbic acid, folic acid, cyanocobalamin, L-cysteine, D-fructose, yeast | 100 | Dragee | 1-2 |
It is more effective to prescribe drugs with a higher content of ferrous iron; they should be taken orally (by mouth) 1-2 times a day. This is the most convenient approach for patients, and therefore their adherence to therapy increases. Many dosage forms of iron include ascorbic and succinic acids, fructose, cysteine, etc., they help the best absorption of iron in the gastrointestinal tract. Iron supplements are best tolerated if taken with food.
Treatment of iron deficiency anemia with parenteral forms of iron supplements
There are clear indications for such therapy:
- with impaired absorption from the intestine (absorption deficiency syndrome, resection of the small intestine, enteritis, etc.);
- exacerbation of chronic diseases of the gastrointestinal tract, such as peptic ulcer of the stomach or duodenum, Crohn's disease, ulcerative colitis;
- poor tolerance to iron-containing drugs when taken orally;
- if you need to quickly replenish iron reserves in the body.
For parenteral administration, iron preparations are used, such as Ferinject (intravenous), Ektofer (intramuscular), Ferbitol (intramuscular), Ferrum Lek (intramuscular, intravenous), Ferkoven (intravenous) [2].
Regarding the treatment of postpartum anemia, there are no clear conclusions about methods. Studies have shown that oral iron does not have a significant benefit over intravenous iron or placebo. However, oral iron does not cause life-threatening allergic reactions like intravenous iron. The clinical value of blood transfusion remains uncertain, in part because of the risks involved. This method can be used to treat postpartum anemia in cases of acute or severe bleeding during childbirth. However, it is not recommended after minor to moderate bleeding in stable patients with mild or asymptomatic anemia. In any case, it is necessary to assess the severity of anemia and consider the use of an iron-rich diet as a method of prevention and adjunct to treatment [7].
Iron deficiency anemia is the most common type of anemia. However, treatment for other types of anemia differs from treatment for IDA. With other types of anemia, to normalize blood counts, it is necessary, for example, to replenish vitamin B12, folic acid, control concomitant chronic diseases and other factors that were the root cause of anemia. To do this, you need a timely visit to a doctor who will diagnose and determine management tactics.
How to improve treatment. Diet
For all types of anemia, the diet should include foods high in iron: pork and beef liver, veal, beef, buckwheat, green apples, pomegranates, mushrooms, cabbage, beans and other legumes, dark chocolate, etc.
You need to eat 4-6 times a day. For normal digestion, food should be at room temperature; too cold or too hot food irritates the gastric mucosa, which prevents the absorption of beneficial elements. The amount of water you drink per day is 30 ml per 1 kg of weight, including tea, juice, soup, etc. Drinking alcohol and smoking are strictly prohibited. Alcohol not only negatively affects the health of the gastrointestinal tract, but also washes out beneficial components in the urine, which is harmful even for healthy people. Smoking increases stomach acidity, which can cause gastritis or ulcers. In this case, the absorption of beneficial microelements will be impaired.
For iron deficiency anemia, it is necessary to include fermented foods (kefir, kvass, sauerkraut, etc.). The acid contained in such products easily comes into contact with iron and prevents the formation of poorly absorbed iron phytates, resulting in improved penetration of iron into enterocytes (cells lining the inner surface of the intestine). The formation of iron phytates is also reduced if plant products are crushed or cooked [10].
Daily iron supplementation in menstruating women is an effective clinical public health strategy for alleviating anemia and iron deficiency, as well as increasing hemoglobin and iron stores. Daily iron supplementation also improves physical performance in women. In addition, there is evidence that iron supplementation reduces fatigue [8].
Daily oral iron and folic acid supplementation of 30–60 mg elemental iron and 400 μg (0.4 mg) folic acid is recommended for pregnant women to prevent anemia, puerperal sepsis, preterm birth, and low birth weight [9].
Contraindications for anemia
For anemia, strict diets are contraindicated; the diet should include foods high in iron, vitamin B12 and folic acid. The development of anemia is also possible while taking certain medications (antitumor drugs, a number of antibacterial, antiprotozoal, antiviral, anti-inflammatory, antirheumatic, antiepileptic and antipsychotic drugs). Therefore, taking this group of drugs for anemia should be under the supervision of a specialist.
Is it possible to treat anemia with folk remedies?
To date, there are no effective folk remedies for treating anemia, because correction of iron deficiency cannot be achieved only by changing diet or using any herbs, decoctions and juices. The reason for this is that the absorption of iron from food is limited (no more than 3-5% from plant foods), and in medications it is contained in higher concentrations.
Epidemiology
According to the Ministry of Health of Italy, Belgium, Germany and Spain, the annual incidence of iron deficiency anemia is 7.2-13.9 per 1000 inhabitants per year. Increased incidence is observed in women, young and elderly people, patients with gastrointestinal disorders, pregnant women and women with menometrorrhagia, and people taking aspirin or antacids. In countries where meat is not a major part of the diet, iron deficiency anemia is observed 6-8 times more often than in European countries. This occurs even despite equivalent total iron in the diet, since heme iron from meat products is better absorbed than non-heme iron. In a study of children and adolescents from Sudan and Nepal, iron deficiency anemia was found in 2/3 of those included in the study. Moreover, in some regions, intestinal parasites significantly worsen the course of iron deficiency anemia due to constant blood loss in the gastrointestinal tract.
Forecast
In most cases of iron deficiency anemia, the therapy provided has excellent results. However, the situation is significantly complicated by the frequent presence of a severe primary disease that causes anemia (most often oncological pathology). In addition, the prognosis of patients with iron deficiency anemia is significantly worsened by diseases of the cardiovascular system.
Iron deficiency anemia is rarely fatal, but severe and moderate cases can cause sufficient hypoxia to aggravate chronic lung and heart disease.
In children, iron deficiency can cause reduced growth rate, reduced IQ and reduced learning ability.
Laboratory diagnosis of iron deficiency anemia
Although the patient's symptoms and complaints can help in the early diagnosis of iron deficiency anemia, the disease is confirmed using various laboratory tests.
Tests for diagnosing iron deficiency anemia:
- general blood analysis;
- peripheral blood smear;
- serum iron, total iron-binding capacity, ferritin.
| Laboratory markers | Changes |
| General blood analysis | Decreased MCV, MCHC; increase in RDW |
| Peripheral blood smear | Microcytosis, hypochromia, thrombocytosis |
| Serum iron | Reduced |
| Total iron binding capacity | Increased |
| Ferritin | Reduced |
Note: MCV—mean erythrocyte volume; MCHC—average erythrocyte hemoglobin concentration; RDW—red blood cell distribution index by size.
General blood analysis
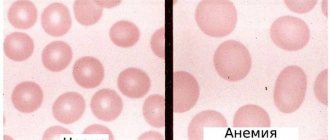
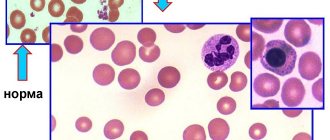
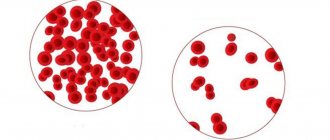
A general blood test allows you to suspect iron deficiency anemia and assess the severity of the disease. In chronic iron deficiency anemia, microcytosis and hypochromia of erythrocytes are observed, characterized by a decrease in the mean erythrocyte volume (MCV) and the mean erythrocyte hemoglobin concentration (MCHC). It should be noted that up to 40% of patients with iron deficiency anemia have normocytic red blood cells, so a normal mean red cell volume does not exclude iron deficiency anemia. The erythrocyte distribution index (RDW) shows the level of variation in erythrocyte size and helps confirm the presence of both normocytes and microcytes in the early stages of the development of iron deficiency anemia, as well as confirm the combined etiology of anemia in the presence of microcytes and macrocytes (iron, B12 and folate deficiency anemia ). An increase in RDW is referred to as anisocytosis.
It should be noted that with iron deficiency anemia, erythrocyte indices change only a few months after the onset of the disease.
An increase in platelet count (more than 450,000/mcd) is often observed, which normalizes with therapy. The white blood cell count is usually within normal limits, but leukocytosis may rarely be observed.
Peripheral blood smear
Examination of a peripheral blood smear is an important step in the diagnosis of patients with anemia. Iron deficiency is characterized by microcytic (reduction in the size of the red blood cell) and hypochromic (decreased hemoglobin concentration in the red blood cell, leading to a “paler” color of the red blood cells) anemia. It should be noted that microcytosis is determined earlier than the change in MCV.
In iron deficiency anemia, codocytes (target cells) are not observed, unlike thalassemia, and anisocytosis and poikilocytosis are most often not expressed. In addition, with iron deficiency anemia, intraerythrocyte inclusions are not observed.
In regions with reduced meat consumption, the coexistence of folate deficiency and iron deficiency is common. In this condition, macrocytes with hypochromic microcytes may be observed in the smear. In this case, the MCV value will be within normal limits.
Ferritin, iron, iron binding capacity
To assess the concentration of iron in the body, studies are carried out on serum iron concentration, total iron-binding capacity and ferritin concentration.
Iron deficiency anemia is characterized by a decrease in the concentration of iron and ferritin and an increase in total iron-binding capacity. However, a complete positive “triad” of laboratory markers occurs at later stages of anemia development. Ferritin is the first to respond to a decrease in iron concentration.
The ferritin molecule is capable of binding 4000-5000 iron atoms at a time, which makes it the main protein storage of iron in the body. Ferritin is found mainly in the cytoplasm of cells of the reticuloendothelial system, as well as in free form in blood serum.
Ferritin concentration directly reflects the total iron content in the body. Thus, serum ferritin concentration is a diagnostic tool for the analysis of iron status. Ferritin concentrations vary greatly among patients of different ages and genders.
In iron deficiency anemia, serum ferritin concentration is one tenth of the normal value. A number of studies have shown that ferritin is one of the most sensitive markers of iron deficiency anemia in the early stages of the disease, however, the results of the study should be interpreted with caution, since in some cases it does not reflect the real picture of the total iron content in the body. Most often this is due to the fact that ferritin is an acute-phase protein and can increase significantly in acute and chronic inflammation, as well as in chronic liver diseases and chronic kidney disease. In this regard, normal ferritin values can be observed when iron deficiency anemia coexists with other chronic pathologies.
Ferritin is also a marker of response and monitoring of iron therapy.
Tests to confirm the etiology of iron deficiency anemia:
Differential diagnosis with anemia of chronic disease
Ferritin is an acute phase protein, and its concentration increases significantly during inflammatory processes, making it impossible to use as a marker for the differential diagnosis of anemia of chronic disease and iron deficiency anemia in some clinical cases. In the late 1990s, a sensitive and early marker of iron deficiency, the soluble transferrin receptor, was described, which increases in proportion to tissue iron deficiency. The main advantage of this marker is that its concentration does not change during the inflammatory response, which makes it an ideal marker for the differential diagnosis of anemia of chronic disease and iron deficiency anemia. Additionally, to increase the accuracy of the study, it is recommended to use the soluble transferrin receptor/Logferritin (sTFR-F). A positive rTGF-F test result is highly likely to diagnose iron deficiency. The sensitivity of the method is 89.19%, specificity is 92.86%.
Hemoglobin electrophoresis
Hemoglobin electrophoresis helps confirm beta thalassemia and other hemoglobinopathies as the cause of microcytic anemia.
Study of hemoglobin in stool
A study of hemoglobin in stool can confirm that chronic gastrointestinal bleeding is the cause of the development of iron deficiency anemia. Modern methods make it possible to detect human hemoglobin in stool with high accuracy and specificity. These methods make it possible to conduct research even in patients who have not previously excluded meat products from their diet. To increase the accuracy of the study, simultaneous testing of fecal calprotectin in stool may be recommended.
The main reason for the appearance of hemoglobin in the stool is malignant tumors of the large intestine, therefore confirmation of iron deficiency anemia and detection of hemoglobin in the stool is an indication for colonoscopy.
Determination of osmotic resistance of erythrocytes
The osmotic stability test of red blood cells is a classic test for diagnosing hereditary spherocytosis. In microspherocytosis, microcytosis and decreased MCV may be observed, but normochromia and normal MCHC values help distinguish this condition from iron deficiency anemia. In rare cases, testing the osmotic resistance of red blood cells helps to accurately determine the etiology of the disease.