Causes of obliterating atherosclerosis of the arteries
The disease causes severe circulatory failure in the legs, dooms patients to excruciating suffering and makes them unable to work. The process is localized mainly in large vessels (aorta, iliac arteries) or medium-sized arteries (femoral, popliteal arteries).
The most striking sign of ischemia of the lower extremities is intermittent claudication, characterized by the appearance of pain, a feeling of numbness and compression in the leg muscles when walking. This sensation forces the patient to stop, after which the pain and compression gradually disappear, but when the load is resumed, the pain returns. The affected leg is usually paler than the opposite leg and cold to the touch. Even minor injuries (scratches, bruises, abrasions) heal poorly and can cause ulcers. The feeling of numbness and pain at rest is often also caused by ischemia of the nerve trunks (ischemic neuritis). Prolonged course of the disease leads to the development of gangrene and inevitable amputation.
The degree of damage to the vascular bed is based on the walking distance. The pain forces the patient to stop, waiting for it to disappear. Without treatment, the disease continues to progress, which leads to a decrease in walking distance, limitation of the patient’s physical activity, and the inability to lead a normal lifestyle. Unfortunately, most often patients associate these pain sensations simply with muscle fatigue due to age, or with venous problems, defining the pain as a cramp, thus delaying seeking medical help and deepening the degree of damage to the arterial bed. In severe cases, the patient cannot walk 10 meters without stopping, but then it gets even worse: pain appears at rest, initially passing in an upright position, but after a short period of time the pain becomes constant, taking painkillers becomes ineffective. Gradually, the lumen of the artery narrows, leading to complete closure. Doctors are forced to admit that patients seek medical attention. help is late when the damage to the limbs is irreversible.
Risk factors:
- smoking;
- regular increase in blood pressure;
- high concentration of total cholesterol and its components in the blood;
- overweight (obesity);
- sedentary lifestyle (hypodynamia);
- diabetes;
- cardiovascular diseases in close relatives.
Damage to the vascular system of the lower extremities is a life-threatening condition, and ranks third in the structure of mortality from cardiovascular diseases. This figure is due to the development of such a severe complication as gangrene of the limb, which often leads to the need for amputation, and with high amputation, the mortality rate is 25%. Along with this, it should be noted that 50% of patients die within a year without amputation after the diagnosis of “critical ischemia”.
Symptoms
- A sharp weakening or disappearance of the pulse in the groin, popliteal fossa or foot
- Pain in the muscles of the lower leg (more often) and thigh, which regularly occurs when walking and goes away after a short rest (stop) - intermittent claudication
- Constant or periodic pain in the foot, requiring a forced position with the limb lowered down
- Coldness, paleness of the foot; in severe cases – the appearance of pronounced cyanosis (cyanosis), marbled spotted color and/or trophic disorders in the form of necrosis (tissue death)
The most striking symptom is the appearance of pain when walking, which forces the person to stop or slow down their walking speed. Most often, in the initial stages, the patient feels increased fatigue of the lower leg muscles, mainly along the back surface, then a pronounced sensation of painful compression appears. In some cases, similar sensations may occur in the thigh muscles and buttocks. As the disease progresses, walking speed decreases and the distance walked shortens. In addition, young men often experience a decrease in potency. All these symptoms are a reason to contact a vascular surgeon.
Conclusion
Atherosclerosis of the coronary vessels is a disease that results from an unhealthy lifestyle, so it is necessary to adjust your diet, establish a daily routine, and also introduce daily physical activity.
As noted earlier, it is extremely difficult to completely avoid this disease and standard treatment with statins inhibits the performance of the most important vitamins D and K2 for humans, which leads to a complete loss of vascular elasticity, so it is important to receive additional doses of these substances from the outside. For example, Osteo K2 completely covers the amount of vitamin D and K2 necessary for the elasticity of the vascular wall, even when taking statins.
Diagnostics
To confirm the diagnosis and clarify the severity of the disease, additional diagnostic methods are needed:
- Ultrasound Dopplerography of the arteries of the lower limbs with measurement of the pressure ratio on the arm and leg, which normally should be close to unity
- duplex scanning of arteries of the artery is a method that allows not only to assess the blood flow in the vessel, but also to see the vessel itself and changes in its walls
- conducting stress tests (treadmill test, i.e. walking on a treadmill under certain conditions)
- according to indications, it may be necessary to conduct a contrast study of the arteries of the heart - multislice computed tomography or angiography of the aorta and arteries of the lower extremity
Prevention of atherosclerosis of the aorta and coronary arteries
How to influence the process of calcification, leading to hardening of the plaque, how to prevent the development of this process?
The main factor influencing the development of atherosclerosis of the coronary arteries and thoracic aorta is a person’s lifestyle. Prevention of the disease will be:
- lack of excess weight;
- balanced quality nutrition;
- giving up alcohol and cigarettes;
- sufficient physical activity during the day;
- elimination of stressful situations and overwork;
- normalization of metabolism (sufficient levels of calcium, vitamins and other microelements).
People with a hereditary predisposition to atherosclerosis must adhere to the rules of a healthy lifestyle to prevent the development of this pathology.
The article described in detail the process of development of the disease, from which it is clear that plaques can form due to excess calcium in the arteries. This happens when the body lacks certain nutrients that would direct calcium into the bones and teeth.
Numerous studies indicate that vitamins such as D3 and K2 help calcium to be absorbed. A person must obtain them from animal foods; vitamin D is also synthesized in the skin under the influence of sunlight. Calcitriol, a derivative of D3, reduces inflammation in the plaque area, and vitamin K2 activates the protein osteocalcin, which redistributes calcium from plaques to where it is most needed - to bone tissue. In addition, K2 is needed for the synthesis of another protein (MGP protein), which is a vascular orderly and removes excess calcium.
Unfortunately, today a person cannot get the required amount of these substances from food, so scientists have learned to create special supplements that, when taken, will compensate for the deficiency of vitamin D3 and K2 in the body. One of these drugs is Osteo K2; you can learn more about it here.
Treatment
In the early stages of the disease, drug treatment aimed at preventing the development of atherosclerotic plaques and improving the rheological properties of blood is acceptable. For this purpose, statins and antiplatelet agents (aspirin) are used.
If the lumen of the vessel is so closed that the blood supply to the limb is disrupted, surgical treatment is necessary:
- balloon dilatation and stenting of the vessel (expansion of the narrowed part and installation of a stent to prevent re-narrowing of the lumen),
- endarterectomy (removal of plaque with the inner layer of the vessel),
- shunting (creating bypass paths for blood flow around an irreversibly damaged area of the vessel).
Causes of atherosclerosis of the vessels of the lower extremities
Atherosclerosis of the vessels of the lower extremities
There is a complex of factors that contribute to
atherosclerotic vascular damage , including the arteries of the lower extremities. There are non-modifiable (that is, unchangeable) and modifiable (modifiable) risk factors. Non-modifiable risk factors include:
- age (the older you are, the stronger the manifestation of atherosclerosis);
- gender (men suffer from atherosclerosis much more often than women);
- genetic predisposition (if there are strokes and cardiovascular diseases in the family history, atherosclerosis is more likely).
Main modifiable risk factors
:
- disorders of lipid metabolism (increased levels of total cholesterol in the blood. A distinction is made between low-density lipoprotein cholesterol and high-density lipoprotein cholesterol. The threat of atherosclerosis increases with an increased content of low-density lipoprotein cholesterol and, conversely, with a reduced content of high-density lipoprotein cholesterol.);
- smoking;
- diabetes;
- obesity, overweight;
- high blood pressure (accelerates the development of atherosclerosis);
- sedentary lifestyle (leads to metabolic disorders);
- poor nutrition;
- renal failure.
For the development of atherosclerosis of the arteries of the lower extremities, smoking and diabetes mellitus are of greatest importance.
Russian National Atherosclerosis Society
Obliterating atherosclerosis of the lower extremities
The concept of obliterating atherosclerosis of the extremities
Obliterating atherosclerosis (that is, that atherosclerosis that leads to “overgrowth” of the lumen of the vessel) is classified as occlusive lesions of the arteries.
Occlusion (from the Latin word occlusus - “locked” [2]), in turn, is the blockage of any vessel due to various reasons, including as a result of atherosclerotic lesions. Obviously, blockage of an artery, for example, the femoral one, leads to a cessation of blood flow through it and disruption of the blood supply to the leg. Thus, obliterating atherosclerosis is a special case of occlusive disease of the arteries, in which the progressive growth of an atherosclerotic plaque inside the vessel leads to blockage of the arteries. Obliterating atherosclerosis can develop in any of the arteries of the extremities, but more often it occurs in the arteries of the legs. Therefore, in this section we will talk about atherosclerotic lesions of the arteries of the legs or lower extremities. Diabetes mellitus is quite often combined with obliterating atherosclerosis of the arteries. Unlike obliterating atherosclerosis, which occurs with damage to arteries of large and medium diameter, with diabetes mellitus occlusion of small arteries, mainly of the foot, develops. The result is a condition called diabetic foot.
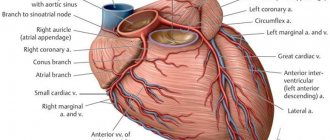
Obliterating atherosclerosis of the legs is most common in older people, but this disease can also be observed at an earlier age (up to 50 years). Men, especially smokers, become ill approximately 10 times more often than women [3, 9]. Often there is so-called multifocal atherosclerosis, in which atherosclerotic arterial lesions develop simultaneously in the arteries of several organs or parts of the body. Obliterating atherosclerosis of the legs can be combined, for example, with atherosclerosis of the coronary arteries of the heart, when damaged, coronary heart disease (CHD) develops. In such cases, the manifestations of combinations of these diseases may be different. As a rule, damage to the arteries of the legs during physical activity will make itself felt earlier than manifestations of coronary artery disease (angina pectoris, etc.) occur.
Concept of blood supply to the lower extremities
Impaired blood supply to the legs can develop with atherosclerotic lesions of various arteries, starting from the final (terminal) section of the abdominal aorta and ending with small vessels of the leg and foot. The terminal portion of the abdominal aorta gives rise to two common iliac arteries. This location of the abdominal aorta is called the bifurcation. The common iliac arteries are in turn divided into internal and external iliac arteries. The internal iliac artery supplies blood mainly to the organs of the pelvic region (bladder, rectum, external and internal genital organs) and partially to the gluteal muscles. The external iliac artery in its initial section supplies blood mainly to the soft tissues (muscles, skin, etc.) of the anterior abdominal wall. The direct continuation of the external iliac artery, starting from the groin region, is the femoral artery, which supplies blood to the leg.
The femoral artery directs its course to the popliteal fossa, simultaneously giving off the so-called deep and superficial branches (arteries). In the knee area, the femoral artery is called the popliteal artery, which subsequently divides into the anterior and posterior tibial arteries, which supply blood to the lower leg and foot. The most important branch of the posterior tibial artery is the peroneal artery, which supplies blood to the calf muscles. The arteries of the leg are connected to each other through their branches (anastomoses), mostly in the area of the lower leg and foot. It is for this reason that if only one of the arteries of the same leg is affected by atherosclerosis, pronounced disturbances in the blood supply to the leg and foot cannot develop. This is due to the fact that the blood supply to the leg in this situation will be provided by collateral (roundabout) arteries. Significant disturbances in the blood supply to the leg and foot will occur either when all arteries of the leg are affected, or when the arteries above are blocked (popliteal, femoral, external iliac, etc.).
Development of obliterating atherosclerosis of the legs
As mentioned above, obliterating atherosclerosis is a special case of occlusive damage to the arteries. There are acute occlusion, which occurs suddenly, and chronic occlusion, which develops gradually. A transition from chronic to acute occlusion is possible, for example, when an atherosclerotic plaque ruptures with subsequent formation of blood clots on its uneven surface (arterial thrombosis). But still, in the vast majority of cases, obliterating atherosclerosis of the arteries of the legs develops gradually. Until, as a result of the growth of an atherosclerotic plaque, the lumen of a particular artery narrows by more than half, manifestations of the disease do not occur.
A decrease in the diameter of the artery lumen causes chronic ischemia (oxygen starvation or hypoxia) of the leg tissues, especially its muscles. Initially, leg ischemia occurs only when performing physical activity and manifests itself as so-called intermittent claudication. This sign (symptom) of the disease consists of the appearance of various kinds of pain, cramps, and sometimes just fatigue in the legs. The main thing is that all these sensations develop when performing physical activity, initially when walking quickly “uphill” or when climbing stairs. The appearance of pain or discomfort in the legs forces the patient to stop. During rest, blood flow in the leg muscles is restored and the amount of chemicals that accumulate in them due to oxygen starvation is reduced. It is these chemicals, particularly lactic acid, that are believed to cause pain in the leg muscles.
The most interesting thing is that for the ischemia of the leg muscles to disappear, it is enough to stop for only a few minutes. There is no need to sit down or lie down. As soon as the discomfort in the leg muscles passes, the same brisk walking can be continued until the attack of leg muscle ischemia resumes. Over time, intermittent claudication occurs during normal walking. The progression of the disease leads to the fact that the distance that can be covered without the appearance of intermittent claudication is steadily decreasing, day by day. Pain with intermittent claudication can occur in various muscles of the legs, which depends on the level of location of atherosclerotic lesions of the abdominal aorta and arteries of the legs. If atherosclerosis develops in the terminal part of the abdominal aorta with a transition to the common iliac arteries, then pain occurs in the muscles of the buttocks, thighs and legs. When atherosclerosis affects the femoral and popliteal arteries, pain occurs in the calf muscles of the leg where atherosclerosis is present. It is believed that with isolated obliterating atherosclerosis of the arteries of the leg, intermittent claudication does not occur. With further growth of the atherosclerotic plaque, the lumen of the artery can decrease significantly. This leads to the fact that pain in the legs can be observed at rest, and the pain becomes prolonged. Increased pain is observed as a result of giving the leg an elevated position.
Significant pain in the legs occurs when, in addition to the main artery, blood flow through the collateral arteries is also disrupted. In addition to pain, in such cases, persistent numbness of the toes may occur along with a sensation of “crawling goosebumps” (paresthesia). In advanced cases, with obliterating atherosclerosis of the legs, tissue necrosis (gangrene) of the foot develops, as well as poorly healing skin ulcers, primarily on the legs and feet. With atherosclerotic lesions of the terminal (end) section of the abdominal aorta, involving the common iliac arteries, men may experience impotence. To be more precise, we are talking about impaired erection of the penis. The combination of intermittent claudication, erectile dysfunction, decreased muscle mass in the legs, as well as constant pallor of the legs and feet with atherosclerosis of this location is called Leriche syndrome (i.e., a set of symptoms).
If a patient with atherosclerosis of the legs has diabetes mellitus, disturbances in the local nervous regulation of tissues, mainly the legs and feet, may be observed. This leads to the loss of so-called pain sensitivity, i.e. when the skin is irritated by any sharp object, for example, a needle, no pain occurs. Skin ulcers in such patients are also painless and difficult to cure. When an atherosclerotic plaque ulcerates on its uneven surface, as mentioned above, blood clots can form, which can contribute to the development of acute arterial occlusion as a result of arterial thrombosis (see above). Manifestations of this life-threatening condition occur below the location of the thrombosis, for example, with thrombosis of the external iliac artery, the blood supply to the thigh, leg and foot is disrupted.
Complaints of patients with obliterating atherosclerosis of the legs
The main complaint of patients with obliterating atherosclerosis of the leg arteries is muscle pain. It can be sharp or dull, sometimes bursting pain, often accompanied by muscle cramps. At first, the pain occurs with intense activity, such as running, fast walking, or climbing stairs. The appearance of pain forces the patient to stop. On average, after 1-5 minutes the pain goes away, and it may be replaced by a feeling of fatigue in the legs. With further exercise, the pain appears again. After a certain period of time, depending on the speed of progression of the atherosclerotic process, there is a reduction in the duration of the distance that the patient can walk without pain. Pain in the legs occurs every time you start walking. At this stage of the disease, there may be no other complaints at rest, with the exception of erectile dysfunction due to atherosclerotic lesions of the terminal abdominal aorta.
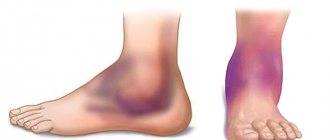
With the increase of chronic occlusion of the arteries of the legs, patients note the appearance of pain at rest. These pains are usually intense and aching. To reduce pain, patients often dangle their legs off the bed while sleeping, which promotes additional blood flow to the leg muscles. Subsequently, due to impaired blood supply to the legs, cracks in the skin of the sole of the feet appear. Even the most minor injury to the legs can contribute to the appearance of long-lasting wounds and ulcers on the legs, which are painless in diabetes mellitus. These skin manifestations cause a lot of concern to patients. Leg skin ulcers in this case are trophic, i.e. associated with malnutrition of the lower extremities. Due to poor blood supply, the legs “lose” their muscle mass, as if they dry out. Numbness in the legs and a “crawling” sensation are often noted.
Diagnosis of obliterating atherosclerosis of the legs
A doctor can often suspect the presence of this disease in a patient as a result of a routine interview. When establishing a diagnosis of obliterating atherosclerosis of the lower extremities, it is mandatory to study the pulsation of the arteries of the legs. Usually the pulsation of the femoral artery (in the groin area), the popliteal artery (in the popliteal fossa) and the arteries of the lower leg (at the ankle) are determined. The pulse weakens or disappears below the level of arterial occlusion. In some cases, especially with narrowing (stenosis) of the terminal abdominal aorta, a noise can be detected above it using a phonendoscope. If the patient only has intermittent claudication, the appearance of the legs may not change. In advanced cases of the disease, the leg may look shrunken and its skin reddened. Hair growth on the legs may also stop and the growth of nails on the toes may be impaired. Non-healing wounds and skin ulcers are often found. The main methods for diagnosing obliterating atherosclerosis of the legs are ultrasound examination of the arteries in combination with an assessment of the speed of blood flow through them (Dopplerography). The combination of these techniques is called duplex scanning.
The use of modern equipment makes it possible to accurately determine the severity of narrowing of the abdominal aorta and leg arteries, including when they are completely occluded. These methods are usually complemented by a comparative assessment of the “upper” (systolic) blood pressure (BP) in the brachial artery and in various arteries of the legs using a conventional blood pressure measuring device. Normally, systolic blood pressure is higher in the legs than in the arms. With obliterating atherosclerosis of the legs, systolic blood pressure at the level of the ankles decreases in proportion to the severity of atherosclerosis of the arteries of the legs. If you supplement the measurement of blood pressure in the legs with methods of reproducing everyday exercise in an office environment, for example, using a “treadmill” (treadmill), then when muscle pain occurs, blood pressure in the legs will decrease.
There are many other bloodless (non-invasive) methods for assessing blood flow disturbances in the arteries of the legs (rheovasography, etc.), but all of them are complementary to Dopplerography. Angiography of the aorta and other arteries is the reference method for diagnosing occlusive lesions. The method consists of introducing a special catheter tube into the vascular bed under local anesthesia by puncturing a large artery of the arm or leg. This catheter is then brought to the site of occlusion and a contrast agent is injected through it. At the same time, X-ray photography is carried out. Angiographic examination is usually performed to decide on surgical treatment of the disease. Currently, there are various angiographic techniques in combination with computer technologies, but traditional angiography still remains the “gold” diagnostic standard.
Treatment of obliterating atherosclerosis of the legs
All patients with intermittent claudication are advised to walk regularly for at least one hour a day. This is necessary for the development of blood supply to the leg muscles through collaterals, as well as for increasing the duration of the pain-free period of walking. The essence of the technique is that the patient must walk until pain appears, then pause until it stops completely, and then continue walking again. Among the medications that are used in the treatment of this disease, vasodilators can be noted. The most effective vasodilators used in the treatment of obliterating atherosclerosis are the so-called prostaglandin E1 drugs, for example, alprostadil.
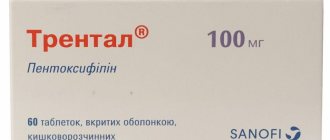
The use of alprostadil leads to dilation of the arteries and improved blood supply to the leg muscles. Alprostadil also reduces thrombus formation. Since this drug dilates the arteries not only of the legs, but also, in particular, of the heart, there is an increase in heart rate, which may be undesirable with concomitant coronary artery disease. There are also other vasodilators (so-called calcium ion antagonists, thromboxane inhibitors or buflomedil), but their effectiveness is currently being clarified. In the treatment of obliterating atherosclerosis, medications are used that reduce blood viscosity and improve the flexibility of red blood cells (erythrocytes), in particular pentoxifylline. This drug is prescribed in large doses, up to 1200 mg per day. Treatment of concomitant diabetes mellitus is necessary, since such a condition as diabetic foot has a poor prognosis due to the lack of effective treatment.
With the development of trophic ulcers and wounds of the skin of the legs, the use of special ointments and creams, including those containing antibiotics, may be required. Surgical treatment of patients with obliterating atherosclerosis of the lower extremities is carried out mainly in cases of severe disturbances in the blood supply to the legs, when complaints appear at rest. Surgical treatment includes the so-called balloon angioplasty, endarterectomy, bypass grafts, removal (resection) of the damaged section of the artery with its subsequent replacement, and the so-called sympathectomy [9].
The choice of surgical treatment method is determined by the location and extent of vascular changes, as well as the general condition of the patient and the presence of other (concomitant) diseases. As mentioned above, many patients with obliterating atherosclerosis of the legs also have severe atherosclerosis of the coronary arteries of the heart (CHD). During vascular bypass surgery or resection of a section of leg arteries in such patients, acute myocardial infarction or other heart complications may develop. Therefore, such patients often undergo heart surgery first. For narrowings of limited extent or complete occlusions of the arteries, balloon angioplasty is effective. The essence of this method is that, under local anesthesia, a large artery of the leg (arm) is punctured (pierced) and a special catheter tube is brought to the place of narrowing (occlusion) of the vessel. At the end of such a catheter there is a special balloon in a collapsed state, which is filled with liquid and inflated under high pressure.
As a result of this manipulation, the atherosclerotic plaque is destroyed and the patency of the artery is restored. Using this method, you can eliminate various narrowings in the arteries of the body, including the coronary arteries of the heart. Sometimes the method is supplemented by installing a special metal spacer spring (stent) in the place of the former narrowing. Balloon angioplasty can be performed without prior surgical treatment of coronary artery disease. In case of multiple narrowing of the artery, especially in combination with its calcification (calcification) or in the case of extended narrowing, vascular bypass surgery is performed, which consists in bypassing the narrowing using a vascular bridge-shunt. It is also possible to remove a section of the artery and then replace it with a vascular synthetic prosthesis.
When narrowing of the aorta and large arteries is limited in extent, they resort to endarterectomy - removal of their inner layer along with the atherosclerotic plaque. Sympathectomy is a surgical interruption of the vasoconstrictor effect of the nervous system. This method is performed when it is impossible to use other types of surgical treatment. Unfortunately, if small arteries of the leg and foot are damaged, especially with diabetes mellitus, restoration of arterial patency is impossible. In particular, it is technically impossible to apply a vascular bypass, since the arteries of the leg and foot can be closed (occluded) along their entire length. If such patients develop gangrene of the foot, then it is necessary to resort to amputation. As a rule, the level of amputation is sufficient to enable the possibility of prosthetic replacement of part of the leg in the future.
Prevention of obliterating atherosclerosis of the legs
General preventive measures boil down to eliminating risk factors for the development of atherosclerosis (impaired metabolism of cholesterol and its derivatives, obesity, detection and treatment of diabetes mellitus, smoking cessation, etc.). It has been noted that complete cessation of smoking, along with drug treatment, contributes to a significant improvement in the condition of patients and slows down the progression of the disease. Preventive foot care is extremely important for patients with foot ischemia. It is necessary to use moisturizing creams, avoid the use of irritating chemicals (callus fluids, etc.), beware of injuries, in particular when cutting toenails, for which it is recommended to seek the services of a pedicurist. Do not use electric heating pads or hot water containers to warm your feet. Carrying heavy objects should be avoided as this impairs the blood supply to the legs. To reduce the risk of various foot injuries, it is not recommended to walk barefoot; you should wear comfortable or orthopedic shoes.
Thromboangiitis obliterans (Buerger's disease)
Thromboangiitis obliterans (Buerger's disease) is a disease of an unknown nature, in which inflammatory changes in arteries of medium and small diameter, as well as in veins, lead to obliteration (overgrowth) of their lumen with disruption of blood movement through them. The disease occurs predominantly in young (20-40 years old) smoking men, and only in 5-20% of cases it is observed in women [6, 9]. It is believed that the basis of the disease is an altered reaction of the body to tobacco, which either causes or provokes inflammatory changes in blood vessels. The development of this disease cannot exclude a hereditary predisposition, as well as an altered response from the immune system. With thromboangiitis obliterans, the terminal sections of the arteries and veins of the legs and forearms, as well as the arteries and veins of the feet and hands, are affected. All layers of the walls of arteries and veins are involved in the inflammatory process, starting with the smallest ones, then inflammation of the arteries of medium diameter joins.
With thromboangiitis obliterans, there is a proliferation of cells in the inner layer of arteries and veins, causing a narrowing of their lumen. Subsequently, blood clots form in the lumen of the vessels, i.e. vascular thrombosis develops. As a result of these changes, the movement of blood through the vessels is disrupted, up to complete cessation. In advanced cases of the disease, hardening of the tissue around the arteries may develop, affecting nearby nerves. Rare cases of thromboangiitis obliterans of the arteries of internal organs have been described [6]. The disease begins with inflammation of the subcutaneous veins (phlebitis), most often of the legs and feet, which is manifested by the formation of sensitive nodules along the veins with redness of the skin over them. These nodules may subsequently disappear in one part of the vein and appear in another. The appearance of obvious signs of arterial damage is preceded by various temperature sensations from the vessels, mainly the hands and feet: patients note either a feeling of cold or heat in the hands and feet. And a number of patients have an abnormal reaction to cold: the fingers and toes, when exposed to cold, first turn white, then turn blue, and finally turn red (Raynaud's phenomenon).
Since the disease develops gradually, disturbances in the blood supply to the same hands and feet do not become noticeable immediately. With a significant narrowing of the lumen of the arteries, pain appears that occurs when walking and goes away with rest. The epicenter of pain is the arch of the feet and the lower part of the legs. Pain may also be felt in the hands when moving your fingers. As the disease progresses, muscle pain appears even at rest. When the lumen of the arteries is completely overgrown, the greatest disturbances in blood supply are observed in the fingers and toes. Trophic ulcers often form at their tips, and in advanced cases of the disease, irreversible necrosis (gangrene) of tissue, mainly the fingers and toes, can develop. The initial diagnosis of the disease is based on the study of patient complaints, as well as on the study of pulsation of the arteries of the arms and legs.
With thromboangiitis obliterans, pulsation in the large arteries of the extremities persists, but pulsation in the arteries of the hands and feet, as well as in the adjacent areas of the forearms and legs, disappears. Accurate information about the patency of blood vessels can be obtained by duplex scanning (a combination of ultrasound diagnostics with an assessment of the speed parameters of blood flow - Dopplerography). Determining blood pressure (BP) at various limb levels may also be useful. At the site of the vascular lesion, a sharp decrease in blood pressure is observed. To confirm the diagnosis, angiography can be used - injection of a contrast agent directly into the arteries, followed by x-rays. Treatment of the disease involves complete cessation of smoking; you should not even chew tobacco. Smoking contributes to the accelerated development of the disease. When you quit smoking, the disease does not reverse, but it may not progress further. To improve blood supply to the legs, daily walking is recommended, up to 30 minutes twice a day, which promotes the development of roundabout (collateral) blood circulation in the leg muscles. Careful care of the skin of the hands and feet is necessary, since any wounds and abrasions may not heal for a long time and may even fester.
For the same reasons, it is recommended to wear comfortable shoes. With the help of medication, temporary improvement can be achieved. Vasodilators, particularly alprostadil, may be helpful. There is currently no effective surgical treatment for thromboangiitis obliterans. As an auxiliary measure, surgical interruption of the vasoconstrictor effects of the so-called sympathetic nervous system (sympathectomy) can be performed.
Temporal arteritis
Temporal (cranial, giant cell) arteritis is a disease of unknown origin, in which, as a result of inflammatory changes in the wall of the arteries, the movement of blood through them is disrupted. The disease occurs in people over 50 years of age, somewhat more often in women. The inflammatory process primarily involves arteries of medium diameter, most often the head and neck. Often there is damage to the aorta and its branches. As a result of inflammation, a pronounced thickening of the inner layer of the arteries occurs, followed by a narrowing of their lumen. Patients are usually bothered by a throbbing headache, often in the temples and back of the head. Quite often there is pain or discomfort in the masticatory muscles when chewing, and sometimes during a long conversation. At the onset of the disease, general fatigue, weakness and increased body temperature may also be a concern. When the arteries of the eyes are involved in the inflammatory process, various visual impairments develop, including complete blindness.
If the disease is accompanied by so-called polymyalgia rheumatica, soreness in various muscles may be noted along with severe weakness. The arteries in this disease, in particular the temporal ones, are somewhat dilated, painful and knotty to the touch (rather than smooth). It should be noted that the arteries can be changed from the inside in the complete absence of corresponding external manifestations. A clinical (general) blood test usually reveals a decrease in hemoglobin levels and the number of red blood cells, an increase in the number of leukocytes and platelets. The erythrocyte sedimentation rate (ESR) in this disease is significantly increased. Ultrasound diagnostics in combination with assessment of blood flow velocity parameters (Doppler sonography) can be useful in identifying temporal arteritis. The main method for diagnosing this disease is a biopsy (obtaining pieces) of the temporal artery and then examining them under a microscope. To ensure diagnostic reliability, pieces of both temporal arteries are usually taken for biopsy. Treatment of the disease is medication. It is aimed primarily at preventing the development of complete blindness. Patients are prescribed so-called glucocorticosteroids, in particular prednisolone, for a long period (months, years). If there is no effect from glucocorticosteroids, the antitumor drug methotrexate is sometimes prescribed [6].
Raynaud's disease and syndrome
Raynaud's phenomenon refers to attacks of involuntary contraction (spasm) of small arteries (arterioles), accompanied by sudden pallor or blue discoloration (cyanosis) of the skin supplied by these arterioles to parts of the body. Raynaud's phenomenon can be either an independent manifestation (Raynaud's disease) or a consequence of other diseases and conditions (Raynaud's syndrome). The most common phenomenon is Raynaud's phenomenon of the fingers, less often - the toes, and sometimes the nose, tongue, etc. The origin of this phenomenon is not entirely clear; it is possible that it is associated with abnormalities of the arterioles themselves. It is also assumed that the so-called sympathetic nervous system is involved in the development of Raynaud's phenomenon, when irritated, a spasm of arterioles develops. Raynaud's disease predominantly affects young women. The disease usually occurs suddenly. Attacks are triggered by exposure to cold or emotional experiences.
The essence of the attacks is the development of a sudden spasm of arterioles and an associated decrease in blood flow, for example, to the fingers. A lack of blood supply is manifested by a sharp pallor of the skin, up to absolute whiteness. In this case, the same fingers temporarily stop feeling anything, but as a rule there is no pain in them. The attack lasts from several minutes to several hours and ends as suddenly as it began. At the end of the attack, the skin acquires a blue tint, and then, as a result of a rush of blood, the blue color changes to red. In some patients, pallor of the skin may be absent, but blueness and redness occur. It has been noted that exposure to heat reduces the duration of the attack. The attacks do not have any clear periodicity. As a result of repeated attacks, the inner layer of arterioles becomes thinner, and accumulations of blood cells, in particular platelets, often form in them (thrombosis).
After several years of illness, the skin over the arterioles becomes smooth, thinned and tense, and the subcutaneous structures seem to disappear (atrophy). In cases where the attack lasts several hours, tiny skin ulcers may develop, for example, on the fingertips. Raynaud's syndrome, as mentioned above, is a manifestation of other diseases and conditions. This syndrome is often observed in atherosclerosis obliterans and thromboangiitis of the extremities, so-called systemic connective tissue diseases: systemic lupus erythematosus, rheumatoid arthritis, etc. In some cases, Raynaud's syndrome develops as a result of side effects of drugs, in particular the so-called? - (beta) adrenergic blockers. It can be difficult to distinguish between attacks that are due to either the disease or Raynaud's syndrome. Raynaud's syndrome can occur in people of both sexes; unilateral lesions are more common, i.e. attacks occur, for example, only with the participation of one of the hands. If no other possible causes of Raynaud's phenomenon are identified within an average of two years, then they speak of Raynaud's disease. One of the methods for diagnosing Raynaud's phenomenon is plethysmography of fingers before and after their contact with cold water. This method is bloodless (non-invasive); it consists of a graphical recording of vascular tone.
General measures to treat Raynaud's disease include avoiding hypothermia and wearing gloves in cold weather. Smoking patients are advised to give up this bad habit, as nicotine promotes arterial spasm. In some cases, psychotherapy and sedative medications can be effective. Drug treatment of Raynaud's disease consists of taking vasodilating and antispastic medications, in particular the so-called? - (alpha) adrenergic blockers (doxazosin, prazosin). In rare cases, especially when skin ulcers that are resistant to treatment are formed, surgical interruption of the influences of the sympathetic nervous system (sympathectomy) is resorted to. Treatment of Raynaud's syndrome comes down to treating the diseases and conditions that caused it, as well as eliminating drug overdose. Measures and medications used to treat Raynaud's disease may also be effective.