The principle of defibrillation: how the rhythm is restored
Defibrillation is the most important step in cardiopulmonary resuscitation.
The principle of operation is based on stopping fast, ineffective contractions of the heart chambers by creating an electrical discharge. Rhythm restoration is carried out using a high-energy (200-360 J) electrical impulse, which passes through the human body in 0.01 s and breaks the “vicious circle”. Technical steps of defibrillation: 1. An electric current is passed between two electrodes, which are applied at the base and apex. The direction of the impulse corresponds to the normal passage of excitation through the conduction system of the organ. 2. The simultaneous energy flow stops the spontaneous contraction of individual fibers and “synchronizes” cardiomyocytes. 3. After a short pause, the normal heart rhythm is restored, which is set by the sinus node (“driver”). If the first procedure is ineffective, defibrillation can be repeated with greater intensity after 2 minutes (after assessing the condition and performing chest compressions). The number of impulses is not limited.
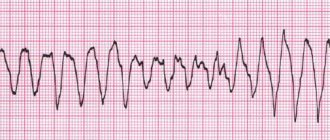
Ventricular fibrillation is a pathological condition that occurs when muscle tissue begins to contract chaotically and very quickly, up to 250-480 beats per minute. In such a rhythm, the ventricle is not able to adequately fill with blood and transfer it to the body. Without timely cessation of this process, the prognosis for survival is unfavorable.
Electrical pulse therapy, or rather its variety - electrical defibrillation, is one of the main resuscitation measures for sudden death. As is known, the most common cause of cardiac arrest is ventricular fibrillation. Based on this, the outcome of resuscitation often depends on the ability to defibrillate as quickly as possible.
If an adult patient is in cardiac arrest and a defibrillator is immediately available, it is advisable to use it as soon as possible. If cardiac arrest occurs without witnesses or a defibrillator is not available, it is advisable to begin cardiopulmonary resuscitation (CPR) while searching for a defibrillator to assess the rhythm and administer a shock if necessary.
In practice, defibrillation during CPR is as follows. While continuing to perform cardiac massage, defibrillator pads or self-adhesive defibrillator electrodes are applied to the patient's chest and the heart rhythm is quickly assessed. Assessing heart rate from defibrillator pads or self-adhesive electrodes is faster than recording an ECG. Chest compressions are interrupted briefly to assess the rhythm. Indications for defibrillation are ventricular fibrillation and pulseless ventricular tachycardia. Asystole and electromechanical dissociation are not indications for defibrillation.
The applicability of double sequential defibrillation in a stable shock rhythm has not been substantiated. Double sequential defibrillation is the almost simultaneous application of two shocks using two defibrillators. Although some reports mention favorable outcomes, a 2021 systematic review found no evidence to support double sequential defibrillation and did not recommend its use in routine medical practice. Existing studies are subject to a variety of biases, and observational studies have not shown improvements in outcome.
When using a manual defibrillator: charge the defibrillator (set the charge), then pause the compressions and apply one shock, after which compressions are immediately resumed. Defibrillation should not interfere with the performance of high-quality compressions; pauses between stopping and resuming compressions should be no more than 5 seconds. The level of energy required for each specific defibrillator is determined by its operating instructions. Typically, for a biphasic defibrillator, the first shock level is at least 150 J, for a monophasic defibrillator - 360 J. Before delivering the shock, you must make sure that no one is touching the patient. The medical professional performing defibrillation directs the resuscitation team.
Please note that medical examination gloves do not protect personnel from electric shock when a shock is applied.
When using an automatic external defibrillator (hereinafter referred to as AED), follow its instructions, trying to minimize pauses in compressions.
After defibrillation, CPR is continued for 2 minutes, then the heart rhythm is quickly assessed again. If ventricular fibrillation or pulseless ventricular tachycardia persists, repeat the shock (150–200 J for a biphasic defibrillator or 360 J for a monophasic defibrillator), then immediately resume CPR (without pausing to reassess the rhythm and determine the pulse), beginning with chest compressions ( ratio with artificial breaths 30:2). Continue CPR for 2 minutes, then quickly assess the rhythm. If ventricular fibrillation or pulseless ventricular tachycardia persists, a 3rd shock is applied (150–200 J for a biphasic defibrillator or 360 J for a monophasic one). CPR is then immediately resumed (without pausing to re-assess the rhythm and determine the pulse), starting with chest compressions (ratio to rescue breaths 30:2).
If there is no recovery of cardiac activity after the 3rd shock, 1 mg of epinephrine (can improve myocardial blood flow and increase the chances of success of the subsequent shock) and 300 mg of amiodarone are administered through venous (or intraosseous) access. Medicines are administered as a bolus diluted in 10 ml of 0.9% sodium chloride solution or against the background of infusion of solutions.
The administration of epinephrine at a dose of 1 mg is repeated after every 2 cycles of CPR (every 3-5 minutes) until the patient shows signs of life or biological death is declared.
The next administration of amiodarone at a dose of 150 mg is possible after the 5th attempt at defibrillation. If amiodarone is not available, lidocaine is administered at a dose of 1 mg/kg (do not administer lidocaine if amiodarone has already been administered). In the case of persistent ventricular fibrillation or pulseless ventricular tachycardia, possible reversible causes of cardiac arrest are excluded.
Types of devices and their structure
A defibrillator is a medical device that generates powerful high-voltage electrical impulses.
Modern devices differ little from their predecessors, consisting of a capacitor, charging and discharge circuit with a pulse generation circuit - biphasic current. New models have a built-in electrocardiograph to assess the success of manipulations. Today there are the following types of devices (examples are shown in the photo):
Manual external defibrillator
Such a device requires professional skills. It is used in conjunction with a cardiograph, which, depending on the type of device, can be built-in or separate. The healthcare professional determines the heart rate and the shock needed.
Manual internal defibrillator
It is used in an operating room directly on an open heart. Has special “spoons” for applying a shock.
Automated external defibrillator (AED)
Designed specifically for inexperienced users or for non-medical personnel (police officers, firefighters, airport workers, train stations, stadiums and other public areas). The device independently detects the heart rhythm and chooses when defibrillation is required and when not.
Using an AED before specialized help arrives significantly increases the victim’s chances of survival. However, it does not replace the use of manual cardiopulmonary resuscitation (without artificial respiration).
Implantable cardioverter defibrillator
This device is similar to a pacemaker (artificial pacemaker); some modern models can act as a pacemaker. The implant continuously monitors the patient's heartbeat and automatically delivers a small electrical shock (a process called cardioversion) if it detects a life-threatening arrhythmia. This does not cause discomfort and significantly prolongs life.
Portable cardioverter-defibrillator
The patient wears the cardioverter on a special belt. The device is necessary for those who are at the stage of preoperative preparation for implantation of a pacemaker. The discharges delivered by the device synchronize cardiac activity.
Publications in the media
Electrical defibrillation is the application of a strong short-term electrical discharge to the heart area, which leads to synchronization of the process of excitation of the myocardium.
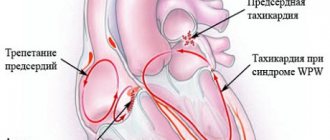
Indications • Ventricular fibrillation or flutter • Prolonged paroxysms of ventricular and supraventricular tachycardia, atrial fibrillation, resistant to drug therapy and accompanied by symptoms of rapidly increasing decompensation of cardiac activity • Paroxysms of atrial flutter with atrial contraction frequency of about 300 per minute or paroxysms of atrial fibrillation-flutter in patients with Wolff–Parkinson–White syndrome.
Contraindications • Intoxication with cardiac glycosides • Sinus tachycardia • Permanent form of atrial fibrillation lasting more than 2 years • Arrhythmias arising against the background of an active inflammatory process in the heart or sharp dilatation of the ventricles with pronounced dystrophic changes in the myocardium.
Technique. Ventricular defibrillation can be performed either open heart or transthoracic. The defibrillator capacitor charging voltage is measured in kilovolts (kV) or joules (J). With the transthoracic defibrillation technique, the capacitor charge is always higher than with an open chest. In adults of average build, at the first attempt at defibrillation it is usually equal to: with the transthoracic technique - 5.5 kV or 200 J, with an open heart - 2.5 kV or 50 J.
• The patient's position is lying on his back.
• Place one of the defibrillator electrodes under the angle of the left shoulder blade (use a large flat electrode, carefully wrapped in several layers of gauze and generously moistened with physiological solution) so that its entire surface is in close contact with the skin.
• To avoid damage by electrical discharge, turn off the recording equipment if the electrocardiograph or cardioscope does not have a special safety device.
• A second electrode with a diameter of 10–12 cm is placed either in the left subclavian region, or under the right clavicle, or along the right parasternal line centered on the third intercostal space.
• If a defibrillator is used, in which both electrodes are equipped with handles, the center of one of them is placed along the right parasternal line at the level of the III–IV rib, and the second - at the level of the V–VI rib along the left anterior axillary line.
• All those present are asked to move away from the bed and under no circumstances touch the patient. The front electrode is pressed against his chest with a force of about 10 kg and a shock is applied. At the moment of its passage, a general one-time contraction of the patient’s muscles occurs.
• After applying the shock, immediately connect the electrocardiograph and take an ECG. The doctor listens to the patient, measures blood pressure, checks the pulse, and analyzes the ECG. If sinus rhythm is restored, electrical pulse therapy is considered completed. If the first attempt is unsuccessful, the capacitor voltage is increased by 1 kV and a second discharge is applied. Sometimes it becomes necessary to apply several shocks (three or four or more). In this case, each time the capacitor voltage is increased by 1 kV, but not more than 7 kV.
• As a rule, defibrillation is preceded by cardiopulmonary resuscitation, which is interrupted only at the moment the electric shock is applied. Under no circumstances should cardiac massage be interrupted while preparing the defibrillator. Defibrillation does not exclude medicinal measures aimed at restoring the energy potential of the myocardium (administration of epinephrine, lidocaine, sodium bicarbonate, procainamide, magnesium solution).
Complications • Cardiac arrest • The appearance of extrasystole • Skin burns at the site of application of the electrodes • Increased body temperature.
Indications
- ventricular (ventricular) fibrillation;
- ventricular (ventricular) tachycardia without pulse.
Defibrillation is not indicated if the heart has stopped completely (with asystole and pulseless electrical activity), or when the patient is conscious or has a pulse.
Execution technique
The algorithm for resuscitation by defibrillation, approved by the American Heart Association in 2015, is as follows:
- Make sure there are indications for defibrillation (assessed using ECG data).
- Initiate cardiopulmonary resuscitation (CPR) with oxygen support.
- First category.
- Continue CPR immediately for five cycles (one cycle consists of 30 chest compressions and 2 breaths). You need to make 100 clicks per minute. Accordingly, the CPR break will take exactly 2 minutes.) Place an intravenous catheter and endotracheal tube. Start ventilation at a rate of 10 breaths per minute. Do not check your pulse and rhythm until this time is over.
- Check pulse and heart rhythm.
- If the rhythm is restored, defibrillation is stopped and the patient is placed under observation.
- If the first shock does not give the desired effect, it is worth repeating the shock.
- Repeat the “rhythm check-defibrillation-CPR” cycle.
The steps listed above are performed only by medical personnel.
External automated defibrillators (EADs) are now in widespread use. They can be found at airports, train stations, shopping centers and other crowded places. They are designed so that every person, without prior preparation, can save someone’s life with the help of audio prompts.
- If you witness a person losing consciousness, make sure that he is not responding to external stimuli - speak to him loudly, jog lightly.
- Call 911 or have someone else do it.
- Check if the victim is breathing and if there is a pulse. If these signs are absent or irregular, begin CPR. Have someone prepare the VAD.
- Before using the VAD, make sure that you and the victim are on a dry surface and there is no spilled water nearby.
- Turn on the device. He will guide your further actions.
- Free the victim's chest from clothing and underwear. If it is wet, wipe it off. Apply the adhesive electrodes as shown on the screen (above the right nipple and towards the armpit from the left nipple).
- Deliver a shock. Do not touch the victim at this moment. The human body conducts current, and electrical defibrillation of a healthy heart will incapacitate the resuscitator.
- Perform CPR for 2 minutes. Use a VAD to check your heart rhythm. If he recovers, continue CPR.
- If fibrillation does not stop, repeat the shock.
- Continue the cycle of actions until medical help arrives.
Defibrillation Introduction Guide
Health care professionals must have knowledge and practical skills in the use of manual and automatic external defibrillators to effectively provide resuscitation.
What is defibrillation
Defibrillation is a method of applying an electrical current to the myocardium. The technique involves emitting an electrical impulse to restore muscle activity in the heart. A correctly performed procedure allows you to resume the interrupted blood circulation process and prevent death.
Automated external defibrillators (AEDs) are used by emergency physicians and critical care physicians to improve survival rates for people experiencing sudden cardiac arrest.
Rice. 1 Automatic external defibrillator
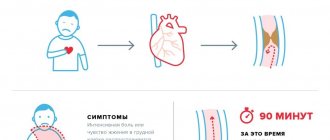
The most effective procedures are those carried out immediately after a circulatory disorder. The more time passes since the cessation of healthy myocardial activity, the lower the likelihood of saving the patient’s life. Every minute of delay increases the risk of death by 10%.
Preparing for defibrillation
Automatic devices for cardiac rehabilitation (automatic defibrillators) are equipped with voice and visual instructions. When providing emergency medical assistance, rescuers must:
- free the victim’s chest from clothing, clean it from dirt and moisture;
- attach electrodes to the victim’s skin;
- connect the electrodes to the defibrillator.
Application of electrodes
The resuscitation team should reduce the level of transthoracic resistance to improve electrical conduction. Shaving the patient's chest will help to increase the productivity of rescue efforts.
The electrodes must be pressed firmly against the surface of the skin. To increase current conductivity and prevent burns, you can use an additional conductor (conductive gel between the electrodes and the place where they are applied). The location of the electrodes depends on the nature of fibrillation (ECG monitoring will show atrial fibrillation, ventricular fibrillation, etc.). If the defibrillator does not have an ECG function, the electrodes are often placed on the patient's chest in the most standard manner - on the sides of the chest, one on the right, the other on the left (axillary). It is important to apply the electrodes so that the electrical discharge between them passes through the fibrillating myocardium.
If emergency care is provided to a person with an implanted pacemaker, the lead should be positioned as far away from the implanted device as possible to minimize the risk of pacemaker failure.
Low effectiveness of the defibrillation procedure for women is observed when electrodes are placed on the mammary glands.
Improved contact
To increase the conductivity of an electrical discharge, physicians should use specialized gels or pastes that are applied to the surface of reusable electrodes. When using disposable (adhesive) electrodes, additional improvement in conductivity in the form of a gel is not necessary, since the electrodes are soft and have good contact over their entire area with the patient’s skin, repeating the shape of the chest. It is important not to allow any liquid to flow between the two electrodes, as this may cause sparks or even prevent the discharge from passing directly through the myocardium. During the procedure, it is prohibited to use ultrasound gel as it has insufficient conductivity.
Which electrodes should you choose?
Adhesive electrodes are the most convenient. They are soft, have low transthoracic resistance, and therefore are characterized by maximum efficiency during resuscitation measures. In addition, doctors do not need to constantly hold them in their hands, lubricate them with conductive gel and apply them again for the next shock.
Soft and hard electrodes have the same speed of first defibrillation. At the same time, flexible models allow for optimal restoration of heart rhythm. Conductive gels are used in conjunction with rigid electrodes.
Features of the use of AEDs
Defibrillation success can be predicted by analyzing the fibrillation waveform. During resuscitation, the doctor may administer a single shock or a series of electrical impulses.
Studies show that mortality increases with short interruptions of chest compressions for mechanical ventilation. To improve the efficiency of emergency care, clinicians are advised to administer a single shock and resume resuscitation, followed by a second shock 2 minutes later.
First category
The effectiveness of the first discharge of an AED is 65%-90% depending on the current power and the patient's condition. Clinicians should set an initial energy level.
Otherwise, there is a high risk of myocardial damage. In general, the use of high energy levels during the first shock does not reduce survival in patients discharged from hospital.
The optimal power is 200 J. Doctors do not associate the efficiency of the device with the shape of the discharge, which can be linear or exponentially truncated.
Second and subsequent categories
The shock should be repeated at 360 J. The clinician may maintain a constant or increasing power protocol.
If the emergency technician observes a return to heart rhythm, a subsequent shock is given without increasing the energy level.
Further tactics of assisting the patient after an attempt to restore rhythm
If defibrillation is successful, the patient requires observation and care. Often, applying an electrical discharge through the conduction system can cause the development of arrhythmia. Neurological disorders associated with temporary cerebral hypoxia are also possible.
Main goals of further actions:
- diagnosis and treatment of the causes of cardiac arrest;
- minimizing negative consequences on the nervous system.
To do this, the following conditions must be met:
- conducting an ECG in 12 leads;
- conducting encephalography in cases of impaired consciousness (coma) and in patients with epilepsy;
- emergency reperfusion (restoration of blood flow) if the cause of cardiac arrest is myocardial infarction;
- maintaining stable blood pressure and blood glucose levels;
- oxygen supply;
- control of body temperature (within 35-36 ˚C);
- consultation with a neurologist.
Resuscitation actions are stopped:
- if resuscitation measures carried out within 30 minutes are ineffective;
- when declaring death based on irreversible cessation of brain function.
Cardioversion
Indications
1.Fibrillation (atrial fibrillation) or atrial flutter
A. Atrial fibrillation or flutter for more than 48 hours (or unknown duration) subject to anticoagulant therapy for 3-4 weeks with maintenance of MHO in the range of 2-3;
b. Paroxysm of atrial fibrillation or flutter, accompanied by hemodynamic disturbances or other dangerous conditions:
- angina pectoris;
- myocardial infarction;
- pulmonary edema;
- arterial hypotension;
- heart failure.
V. Atrial fibrillation or flutter of any duration in the absence of thrombi in the left atrium and left atrial appendage according to transesophageal echocardiography;
d. Atrial fibrillation or flutter less than 48 hours old (the appropriateness of anticoagulant therapy depends on the risk of embolic complications).
2. Atrial tachycardia;
3. AV nodal reciprocal tachycardia;
4. Reciprocal tachycardia with the participation of additional pathways.
Selecting the initial discharge power
| Indications for cardioversion and recommended initial shock power for adult patients: | |||
| Type of arrhythmia | Pulse power in joules | ||
| monophasic | biphasic | ||
| Stable monomorphic ventricular tachycardia | 100 J | 100 J | |
| Atrial fibrillation | 360 J | 200-360 J | |
| Atrial flutter | 50-100 J | 50-100 J | |
| Paroxysmal supraventricular tachycardia | 50-100 J | 50-100 J | |
Contraindications
1. Thrombi in the atria in the absence of indications for emergency cardioversion;
2. Sinus tachycardia;
3. Tachycardias caused by increased automaticity:
- Polytopic atrial tachycardia;
- Accelerated AV nodal rhythm.
4. Glycoside intoxication;
5. Severe electrolyte disturbances in the absence of indications for emergency cardioversion;
6. Atrial fibrillation of unknown duration in the absence of anticoagulant therapy and transesophageal echocardiography data;
7. Contraindications to anesthesia.
Preparing for elective cardioversion
- The patient must sign consent for cardioversion;
- Before anesthesia, the patient should not take food or liquid for 4 hours;
- In patients undergoing elective cardioversion, transesophageal echocardiography is indicated to identify thrombi in the left atrium. Standard echocardiography is not informative enough in this regard;
- It is recommended to discontinue cardiac glycosides 3-4 days before the procedure;
- Potassium levels should be 4.0-5.0 mmol/L.
Anesthetic care
Patients undergoing cardioversion need to switch off consciousness. Preparation, preoperative examination, equipment are generally accepted in anesthesiology. Monitoring is standard. Features : intravenous anesthesia is superficial and short-term - pay attention to the recommended doses of anesthetics. Anesthesia is usually carried out while maintaining spontaneous breathing in the patient.
Cardioversion is performed as soon as the patient loses consciousness (floating eyeballs, loss of speech contact) - under conditions of superficial anesthesia. Due to decreased cardiac output, the onset of anesthesia may be delayed. Doctors are in no hurry to increase the dose of anesthetic above the recommended values - this is fraught with the development of hypotension and respiratory depression. Kits for tracheal intubation and temporary pacemaker should be ready.
It is recommended to pre-dilute 1 mg of epinephrine in a syringe in 10.0 ml of 0.9% sodium chloride in case of a sharp drop in blood pressure - administer 1 ml as a bolus if necessary. Advice to doctors: do not include narcotic analgesics and atropine in premedication.
Performance
1. Preoxygenation;
2. Intravenous anesthesia, one of the following drugs is used:
- Propofol 40-80 mg, drug of choice;
- Midazolam 5-15 mg, not very convenient due to prolonged sedation;
- Sodium thiopental 1% – 100-200 mg;
- Ketofol (propofol 100 mg + ketamine 100 mg) – 3-6 ml of mixture, indicated for hypotension in the patient.
All of these drugs should be administered very slowly.
Equipment
- Defibrillator with ECG monitor and external pacemaker;
- Spare defibrillator;
- ECG monitor with electrodes;
- Gel for electrodes.
Attention. A defibrillator can break down at the most inopportune moment, which can have unpredictable consequences for the patient. A spare defibrillator, even a simple one, will avoid problems.
How to correctly position defibrillator electrodes during defibrillation and cardioversion
The standard location is the anterolateral arrangement of electrodes: one on the right under the collarbone near the sternum, the second on the left above the apex of the heart. But with the same effectiveness, depending on the situation, you can use other options for the location of electrodes, for example, anterior-posterior, when one electrode is located near the sternum on the left approximately at the level of the fourth intercostal space, and the second is opposite it from the back. Or: anterior-left subscapular and anterior-right subscapular.
If the patient has an implanted pacemaker or cardioverter-defibrillator
During defibrillation and cardioversion in patients with implanted pacemakers, the electrodes are usually installed in the anteroposterior or anterolateral position. Do not place the electrode directly over the implanted device. They try to choose a position so that the distance between the electrodes and the pacemaker is > 8 cm. After the procedure, the operation of the pacemaker or cardioverter-defibrillator is checked.
conclusions
Nowadays, not only every ambulance, but also many public spaces are equipped with a defibrillator. According to statistics, the prevailing number of sudden cardiac arrests occur outside medical institutions.
The sooner a victim who has lost consciousness receives first aid, the higher his chances of survival and health. It is possible to bring a patient with ventricular tachycardia or fibrillation back to life if the heart is started with a defibrillator while simultaneously performing cardiopulmonary resuscitation.
Knowledge of the principles of CPR and your concern can save someone's life.
Electrical defibrillation of the heart
One of the most interesting and voluminous sections of cardiology is arrhythmology. Within the framework of this science, specialists treat various heart rhythm disorders.
Arrhythmias are a disturbance of the heart rhythm, its frequency and regularity of contractions, which leads to disruption of the normal functioning of the heart with unpleasant subjective sensations and/or complete cardiac arrest. Sinus rhythm is normal, all deviations from it are considered arrhythmias. Arrhythmia can be an independent cardiac pathology, or also occur as complications of other cardiac problems - heart attacks, valvular heart disease, myocarditis, cardiac contusions. According to statistics, 15% of cardiac deaths are caused by arrhythmias. The most dangerous arrhythmia is ventricular fibrillation.
Every year in European countries, about 700 thousand cases of sudden death as a result of cardiac arrest are recorded, 65% of which are caused by ventricular fibrillation. Ventricular fibrillation is considered the main mechanism of sudden cardiac death.
To relieve ventricular fibrillation, the method of electrical defibrillation is used. This method is an integral part of modern intensive care. It is carried out using a defibrillator device by emergency medical services doctors and resuscitators of intensive care units. In recent years, automatic external defibrillators (AEDs) have been installed in public places in European countries. World experience in the use of AEDs shows a significant increase in the survival rate of victims of SCA: in 38% of cases of sudden cardiac arrest when an AED was used by bystanders, 22% - when used by arriving doctors, 9% - when performing only standard cardiopulmonary resuscitation, and only 1% - in other cases.
A bill on the use of AEDs is currently being considered in Russia. “The bill provides for the possibility of providing first aid to an unlimited number of people using automatic external defibrillators in the event of situations requiring the provision of such assistance,” the accompanying documents note.
Currently in Russia, only certain categories of health workers are allowed to use automatic defibrillators. Meanwhile, in case of sudden cardiac arrest, every minute of delay reduces the chance of saving a person by 10%,
What is a defibrillator ? It is a device used in medicine to treat heart rhythm disorders using an electrical impulse. Main indications for defibrillation:
- ventricular fibrillation (chaotic contraction at a speed of 200-300 beats per minute);
- ventricular flutter (contraction is rhythmic, but at a speed of about 300 beats per minute);
- atrial flutter (rhythmic but rapid contraction up to 240 beats per minute);
- atrial fibrillation (chaotic contraction, 300 beats per minute).
There are cardioversion and defibrillation.
Cardioversion is the impact of an electrical discharge synchronized with the QRS complex. For various tachyarrhythmias (except ventricular fibrillation), the impact of the electrical discharge must be synchronized with the QRS complex, since if the discharge is exposed before the peak of the T wave, ventricular fibrillation may occur. The impact of an electrical discharge without synchronization with the QRS complex is called defibrillation. Defibrillation is carried out in case of ventricular fibrillation, when there is no need or possibility to synchronize the effects of an electrical discharge. If defibrillation is successful, the shock stops the heart, after which it should resume its own normal electrical activity (sinus rhythm). Electrical defibrillation (EDF) The basic principle of EMF is that under the influence of a powerful and short-range electrical impulse, depolarization of all muscle fibers of the myocardium occurs with the subsequent development of refractoriness, after the end of which a newly arising impulse from the sinus node is able to restore spontaneous heart contractions. Methods of electrical defibrillation of the heart. There are electrical defibrillation of the heart: indirect (external), when the defibrillator electrodes are applied to the chest, and direct, when the electrodes are applied directly to the heart with the chest open. The basis of successful EDS depends to a certain extent on the training and knowledge of medical personnel. In the inpatient emergency department of the Volyn Hospital of the Presidential Administration of the Russian Federation, the staff developed resuscitation skills, including defibrillation using modern equipment. Classes are held regularly to maintain acquired skills.