- Doctor of Medical Sciences, Prof. L.M. BASILETS,
- Doctor of Medical Sciences, Prof. A.V. TUEV,
- Ph.D. A.Yu. VYSHENSKAYA,
- Ph.D. N.S. KARPUNINA,
- HE. SARAPULOVA,
- V.V. VUSTINA,
- K.V. TRENOGYNA,
- A.A. CURVE
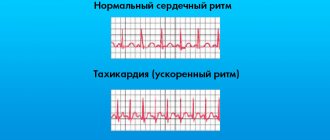
Premature excitation syndrome, or preexitation, of the ventricles (PES) occurs in different age groups of the population, from newborns to the elderly, including 0.04 - 0.31% of cases in children and 0.15% in adults. Preexcitation, or preexcitation, is defined as the excitation of a greater or lesser part of the ventricular myocardium by an impulse conducted from the atria along the accessory pathways (APP) earlier than when the impulse is transmitted to the ventricles through the atrioventricular node and the His-Purkinje system. The most common types of ventricular preexcitation syndrome are Wolff-Parkinson-White syndrome and short P-Q(R) interval syndrome, also known as Clerk-Levy-Christesco syndrome. It is customary to distinguish between two concepts: phenomenon and PEJ syndrome. According to the proposal of the WHO expert working group (1980), in the presence of electrocardiographic signs of pre-excitation along the Kent bundle, the term “Wolff-Parkinson-White phenomenon” is used, and in the case of the addition of paroxysmal tachyarrhythmias. Over the past 20 years, significant relationships have been identified between the autonomic nervous system (ANS) and mortality from cardiovascular causes, including sudden cardiac death. An important role in the formation of arrhythmias in PE syndrome is played by a violation of the autonomic status, since in the presence of additional conduction pathways, the autonomic imbalance can affect conduction along normal and abnormal conduction pathways. It has been proven that a shift in autonomic tone towards the predominance of sympathetic influence can be a provoking factor for cardiac arrhythmias. T. Honda et al. concluded that increased sympathetic activity in patients with PE syndrome contributes to the development of atrial fibrillation (AF). There is much clinical and experimental evidence that the autonomic nervous system plays an important role in the genesis and maintenance of malignant arrhythmias. An accessible and informative method for assessing the vegetative status of patients in the clinic is the analysis of heart rate variability (HRV). The presence of autonomic disorders in heart pathology serves as a pathogenetic basis for the use in complex therapy of drugs that combine anxiolytic, anti-anxiety properties and normalize autonomic imbalance. Currently, the daytime anxiolytic-adaptogen adaptol (Olainfarm, Latvia) is widely used for this purpose, which has pronounced anxiolytic, vegetostabilizing, stress-protective and antioxidant properties, as well as high safety (being a derivative of bicyclic bioureas, adaptol is close to natural metabolites of purine metabolism ). An important advantage of adaptol is the absence of “behavioral toxicity”, i.e. drowsiness during the daytime, muscle relaxation, disturbances of attention and coordination of movements, as well as the absence of dependence and limitation of physical and mental activity. Positive effects of the drug were detected in patients with neurocirculatory dystonia, hypertension, in patients with coronary artery disease with post-infarction cardiosclerosis, and with cardialgia of inorganic nature. The effect of the drug on autonomic imbalance in cardiac arrhythmias has been practically not studied.
The purpose of this work is to study HRV and arrhythmogenic readiness of the myocardium in patients with the syndrome and phenomenon of ventricular preexcitation and to evaluate the effect of adaptol in complex antiarrhythmic therapy.
Archives
Short Wiklad
L Eckardt, G Breithardt, P Kirchhof Heart 2006;92:704–711.
Diagnosis of wide-complex tachycardia (WCT), when the QRS complex is more than 120 ms, is a difficult problem, regardless of the numerical recognition of the criterion for differentiating between ventricular and supraventricular tachycardias (with VT) due to conductivity aberration. Correct diagnosis is important both for the provision of uncomplicated assistance and for the careful management of patients with TSC.
The next thing to look at is to discuss the main reasons, as well as clinical and electrophysiological criteria for TSC (Table 1) in patients without structural heart disease.
Table 1. Causes of TSC in patients without structural heart disease
| Supraventricular | Shlunochkova | |
| Monomorphic | • Blockade of the bundle branch of His (Fig. 1, 2): a) functional (right - more often, lower left); b) background c) frequency-delayed • Antidromic (retrogradely carried out through the atrioventricular vein) (Fig. 3, 4) • Non-specific conductivity damage: a) antiarrhythmic drugs of class I or III; b) electrical failure | • Left bundle branch block (LBBB), downward stimulation of the electrical axis of the heart (Fig. 7): idiopathic right ventricular tachycardia • Right bundle branch block (RBBB), dilation of the electrical axis of the heart upward (Fig. 8): idiopathic left ventricular tachycardia • PC, a mediator that is a pacemaker |
| Polymorphic | • Atrial fibrillation with preexitation (Fig. 3) | • Rapid tachycardia (long QT syndrome) (Fig. 9) • Brugada syndrome • Catecholaminergic polymorphic ST (Fig. 10) • Short QT syndrome |
Note. All patients with TSC need to be treated in the same way as with ST, if another type of tachycardia has not been identified.
Up to the main categories of TSC, cover schular tachycardia (ST), SVT with damaged internal socket conduction, as well as rhythms during cardiac pacing of the sac. The presence of background structural heart disease does not allow us to exclude the presence of HT and does not necessarily indicate a good prognosis for illness. However, since the patient experienced similar episodes throughout the anterior stages, SVT is more significant, lower PCS. Implementation of tachycardia with the help of the Valsalvi maneuver or injection of adenosine also allows for supraventricular gait, although several types of VT can also be administered with the help of vagal tests (for example, fascicular VT).
The use of TSC in a patient who is in the state of vascularity and is hemodynamically stable, not obstructive and supraventricular. Clinical manifestations lie under the hemodynamic inheritance of tachycardia. The smell depends on the frequency of the heart rate (HR), the level of severity of myocardial dysfunction, the level of rapture in the cob, as well as vegetative disorders. Physical examination of a patient with TSC may indicate hemodynamic disturbances (hypotension, cardiac failure or cardiogenic shock). When avoiding cardiac dysfunction and arterial pressure and/or short-term tachycardia, arrhythmia may manifest itself as heart palpitations, shortness of breath or even some discomfort.
SUPRAVENTRICULAR TACHYCARDIA WITH WIDE QRS COMPLEXES
Damage to the internal sac conduction may result in changes in heart rate, as well as damage to the cardiac conduction system. In patients with background (obvious during normal output rhythm) bundle branch block (BNBB), SVT can lead to tachycardia with wide QRS complexes. At the same time, frequency-dependent and/or “functional” (only evident during tachycardia) RBBB can also lead to TSC. Functional aberration is a consequence of rapt changes in the cardiac cycle, when parts of the His-Purkinje system frequently or completely lose restlessness. Functional RBBB occurs more frequently, while less functional LBBB occurs due to greater refractoriness. If discrete fluctuations in the cardiac cycle indicate a transition from wide complex tachycardia to narrow QRS complex tachycardia, which facilitates the diagnosis (Fig. 1). Rapt's influence on the tachycardia cycle “short-long” shortens the refractoriness of the His-Purkinje system, “long-short” shortens its refractoriness. Functional BBBB can be preserved by extending a few consecutive impulses, fragments of the blocked anterograde His bundle can be activated transseptally through its protidal component (“interconnection phenomenon”). The remnants of the triviality of the refractory period lie within the triviality of the anterior cardiac cycle (the longer the trivial anterior cycle, the shorter the refractory period), the rapt level of the triviality of the cardiac cycle (“long-short” or “short-long”) increases and likelihood of the appearance of functional RBBB - for example, in fibrillation atrium (AF) (Ashman phenomenon) (Fig. 2).
Picture 1.
An episode of tachycardia with wide QRS complexes with a RBBB configuration, which spontaneously transitions from tachycardia with narrow QRS complexes with a slight increase in difficulty to the tachycardia cycle. Retrograde P waves are avoided after the QRS complex (pseudo-r' in lead V1 and pseudo-s in lead II, III and aVF (*), which suggests a typical AV nodal reentrant tachycardia.
Figure 2(A).
Atrial fibrillation due to scapular aberration due to the Ashman phenomenon and, possibly, delayed transseptal conduction of impulses. After the trival pause (*), the refractory period of the left limb of the His bundle contractions, which represents the appearance of 10 complexes of the RS type with morphology of the LBBB type. The Zbereznoy of the Aburasya, izhirno, the prekhovan of the translite was conducted by the Impulsiv (phenomenon of mutual) to the liva nіzhi, with the blockade of the Anterograd, post -worn izmpulsіv near the livіy nizhi. (B) The suture line represents the His bundle; peririvchasta (speckles) - left (right) nizhka. The strong horizontal dark spots represent the refractory period.
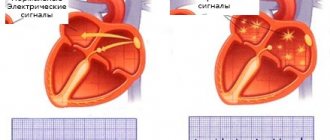
Tachycardia in Wolff-Parkinson-White syndrome involves a minority of TShK. In these tachycardias, activation of the scutulae is achieved either directly or via the accessory pathway. Change the nature of the immediate awakening (Fig. 3) at the same time as changing the trivality of the cardiac cycle and carrying out AF through the accessory pathway. The monomorphic pattern of preexitation may also be caused by reciprocal (re-entry) tachycardia (due to anterior tachycardia or anterior cardiac thrombosis due to conduction through the accessory pathway). If AF is evident, then the partial rhythm of the scutulae, caused by atrioventricular (AV) conduction through the accessory tract (Fig. 3), can lead to fibrillation of the scutum and cardiac death. If in reciprocal tachycardia the impulse passes anterogradely through the accessory pathway, the tachycardia is called antidromic. The retrograde component of the reentry ring is primarily the AV vuzol, otherwise it is another accessory pathway. By contrast, antidromic AV reciprocal tachycardia is more likely to be avoided than orthodromic tachycardia. Remnants of the accessory pathway connect the anterior myocardium and the sac at the level of the AV receipt, ECG with SVT from pre-exitation if it is impossible to dissect from the CT, as it is based on the sac.
Figure 3.
Antidromic tachycardia (A) through the left pubic accessory pathway in a patient with Wolff-Parkinson-White syndrome. (B) Atrial fibrillation from rapid transmission through the accessory pathway in the same patient (shortest RR interval 200 ms).
In TSC with the morphology of LBBB and the electrical axis of the heart moving to the left and up (Fig. 4), it is necessary to first consider the possibility of an atriofascicular accessory path (Mahaima). Patients with these pathways may exhibit episodes of tachycardia with pre-exitation, while under sinus rhythm there is no sign of pre-excitation of the pathways. In this case, tachycardias with narrow QRS complexes do not occur, since the impulse through the accessory pathway is not carried out retrogradely. Typical QRS morphology during tachycardia is characterized by a small, short cob-shaped R wave, with further sharp decreases in the led V1.
Figure 4.
ECG at 12 times during the hour of antidromic AV reciprocal tachycardia with acquisition of the right atriofascicular accessory tract (Maheim) for anterograde conduction of impulses. These paths in typical forms are located on the endocardial surface of the pilar wall with distal entrances into the apical part of the right leg of the His bundle. Differential diagnostics operates according to the rhythm of the pacemaker, since most of the pacemaker electrodes are placed at the top of the PN.
Other mechanisms of aberration in the shunts are a decrease in myocardial velocity due to the effects of drugs or electrolyte imbalance, for example, hyperkalemia. In addition, high doses of sodium channel blockers (antiarrhythmic drugs of classes IA and IC) may cause a nonspecific increase in the disturbance of the QRS complex. In case of drugs of class ІC, TSC is provoked through a controlled frequency of anterior atrial stimulation, which allows for a 1:1 ratio to be carried out (Fig. 5). They also reported episodes of induction of persistent monomorphic heart disease during an hour of physical exercise against the background of stagnation of antiarrhythmic drugs in young healthy individuals without structural heart disease.
Figure 5.
Application of TSC against the background of administration of the antiarrhythmic agent class IC flecainide in a patient with atrial fibrillation. Flecainide induces this tachycardia through matching the rhythm of the anterior heartbeat with the appearance of AV conduction in a 1:1 ratio.
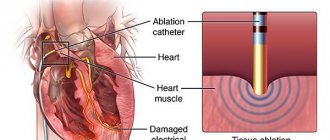
Depending on the situation, the management of patients with SVT with wide complexes can be different: for infrequent and unstable episodes - without therapy, in others - drug therapy or radiofrequency catheter ablation. The introduction of catheter-based debridement techniques has dramatically changed approaches to the management of patients with SVT. The current approach is to evaluate the possibility of radiofrequency catheter ablation in all patients who require a cleanse. Trival pharmacotherapy (for the reason that there is no preexitation - method of AV blockade) should be selected from those patients who are undergoing catheter ablation, if it is ineffective or is associated with high rizikom made it difficult, such as AV blockade is irrevocable.
ELECTROCARDIOGRAPHIC CRITERIA FOR DIFFERENTIAL DIAGNOSTICS OF SVT AND ST
Zagalom, since the configuration of the QRS complex during the hour of TCT does not predict the aberration of the internal socket conductivity, the most common is the ST (Fig. 6). If there is any doubt about the procedure for TSC, the patient should be treated as if he had a CT. The presence of a complex of the RS type in any precordial conduction or the presence of an interval from the cob of the R wave to the lowest point of the S wave is more than 100 ms indicates the high homogeneity of the PC. In addition, use the following ECG criteria for differential diagnosis between ST and SVT with aberration:
- Troublesome to the QRS complex. CT is the most significant, since the QRS waveform in complex type RBBB is more than 140 ms, and in the morphology of LBBB it is more than 160 ms.
- The entire QRS complex. The frontal everything at the intervals from –90° to ±180° cannot be obvious with any type of RBBB and this allows one to think about the ST. Also, it is important that negative QRS complexes in divisions I, II and III are a basic criterion for the detection of PT.
- Concordant negative ECG complexes in breastfeeding patients. Since in all chest abductions the QRS complexes are predominantly negative, the definitive diagnosis is PC. Since all thoracic outlets have positive QRS complexes, it is necessary to carry out a differential diagnosis between antidromic tachycardia and those caused by the left pubic accessory tract and PC.
- QRS morphology in V1 and V6 leads. When configuring the QRS type of RBBB, the R wave is monophasic, wide (> 30 ms) R, and the qR in the lead V1 indicates the high mutability of the pcs. Monophasic R, or S with a larger amplitude, lower R in the withdrawn V6, also allow the allowance of PCs. With QRS type LBBB, a wide R wave (especially with a duration of more than 30 ms) and/or a further decrease to the lowest point of S at the V1 and Q at the V6, note the core of the PC.
ATRIOVENTRICULAR DISOCIATION
This is one of the most important criteria for the differential diagnosis of ST and SVT. This is avoided in 20–50% of cases of ST and in the majority of cases with SVT. AV dissociation is characterized by a changeable pulse pressure, irregular beats in the jugular veins and a change in the sonority of the first heart tone. In order to detect AV dissociation, three elements of ECG recording at 12 leads and a final analysis of the ECG are necessary. In addition, approximately 30% of VT episodes are associated with retrograde conduction 1: 1. With AV dissociation, severe rapidity can be avoided, as a consequence of the one-hour conduction of awakening from the anterior to the sacs.
Registration of a 12-channel ECG under the hour of ST helps to approximate the placement of the device. The morphology of the ST of the LBBB type in the lead V1 is characteristic of tachycardia originating from the right sac (RS) or the intersac septum. The straightness of the electrical axis of the heart upward indicates tachycardia from the posterior wall, while straightness downward indicates tachycardia from the anterior (upper) wall of the heart. The dominance of R waves in leads V2–V4 is indicated by those whose tachycardia core is located near the base of the sac. In case of idiopathic tachycardia from the outflow tract of the prostate tract, the frequency of the QRS complex at the hour of the heart rate is usually >140 ms, if it is from the outside wall of the outflow tract of the arrhythmia, and <140 ms, if the arrhythmia is from the side of the towns exiting the tract PSh. The transition zone of the R wave in case of tachycardia from the outflow tract of the PN is especially careful at the leads from V2 to V4, the earlier the more the tachycardia core is displaced upwards at the septum. The transition zone of the R wave at the adducted V2 allows for the placement of the nucleus directly below the valve of the pulmonary artery or at the outflow tract of the left sac.
SLUNOCHKOV TACHYCARDIA IN PATIENTS WITHOUT STRUCTURAL HEART CONCERNS: “IDIOPATHIC”
“Idiopathic” ST is a nonspecific term that denotes a heterogeneous group of arrhythmias. Patients may be completely asymptomatic or experience transient symptoms such as palpitations, confusion, or presyncope; In this case, with arrhythmias, behind the culprit of the Swedish polymorphic CT, which occurs with inflated arrhythmic syndromes, it is rarely life-threatening. The mechanisms of arrhythmia formation are rhinestones, trigger activity, and catecholaminergic automatism. “Idiopathic” PT varies due to clinical manifestations (instability or stability), associated factors (for example, exercise), place of gait (left or right shunt), and responses to antiarrhythmic drugs. and medications (for example, adenosine and verapamil) or for primary electrical disorders.
PATIENTS WITHOUT STRUCTURAL HEART CONSISTENCY ARE SUBJECT TO RADICAL HEART CARE
Idiopathic tachycardia from the right outflow tract
Arrhythmia, which should be located at the outflow tract of the heart, manifests itself as a shock with QRS complexes of the LBBB type and the downward direction of the cardiac axis (Fig. 7). They occur more often in young patients (more often in women, less often in men) without structural heart disease; This tachycardia accounts for up to 70% of all types of idiopathic strokes. Although it is important that this tachycardia occurs sporadically, without relief in the family, it is considered as a “primary electrical illness.” This type of tachycardia may be of significance in the differential diagnosis of mild or subclinical forms of arrhythmogenic cardiomyopathy PS. These studies suggest that the main mechanism is trigger activity, triggered by late post-polarizations, a mediator such as adenyl cyclase. Idiopathic tachycardia from the outflow tract is strongly associated with anxiety or stress. They can also manifest themselves as portal extrasystoles, or unstable arrhythmias with a tendency to occur at rest, or be provoked only when forced (Galawarden's tachycardia). At the same time, these forms of tachycardia may also manifest a different spectrum of similar arrhythmias. Idiopathic tachycardias from the outflow tract are very well tolerated, probably due to the preserved function of the shunts. Looking at it, the form of CT is shown to be characterized by a favorable and satisfactory prognosis for CT with a structurally ill heart. This type of arrhythmia may respond well to treatment with beta blockers, sotalol or calcium channel blockers, as well as catheter ablation.
Figure 7.
Repeated episodes of idiopathic right heart tachycardia with a QRS complex of the LBBB type and a downward displacement of the heart axis.
Idiopathic left ventral tachycardia (fascicular ST)
Idiopathic left ventricular tachycardia most often occurs in young patients, especially men, without structural heart disease. The arrhythmia is characterized by very narrow (0.10–0.14 s) QRS complexes with RBBB-like morphology with narrow, low S waves in the thoracic outlets and ventricles of the cardiac axis to the left and up (Fig. 8). It is important to note that tachycardia is indicated to be due to the re-entry mechanism or as a result of trigger activity against the background of late post-depolarization. It appears in the area of the septum or next to it, near the back of the left limb of the His bundle. Rarely, CT may originate from the anterior limb of the left bundle of His and be characterized by a type of RBBB with a deviated cardiac axis to the right. These patients are often not responsive to treatment with beta blockers, but are often sensitive to verapamil. The prognosis is very good, but in these patients clinical symptoms are often more pronounced. When treating symptomatic patients early, consider the possibility of catheter ablation (Fig. 8).
Figure 8.
Non-contact mapping of idiopathic left ventricular tachycardia with RBBB configuration, displacement of the electrical axis of the heart to the left.
A - Multiple electrode at the left little hole. Vikoristano system, which ensures the possibility of mapping the surrounding screw complex. Use electrograms one hour at 3000 points in the endocardium. Non-depolarization of myocardium readings by the erysipelas on the trivial isopotential map.
B — A white stake is indicated at the site of the greatest early depolarization. Radiofrequency ablation was carried out in the distal part of the posterior limb of the left leg of the His bundle, which may have caused a serious injury to the PC.
C - Tachycardia is no longer induced.
RECIPROCURRENT TACHYCARDIA OF THE BOTTOM OF THE HISTORIC BUNCH
On the re-entry in the His-Purkinje system, a significant proportion of monomorphic CTs in patients with heart failure falls, unless tachycardia occurs in a structurally unchanged heart. The spine of the reentry widens through one leg (usually to the right) and rotates through the pro-leg. As you look at it, a QRS complex is formed, which has a configuration of LBBB and either normal or displaced to the left electrical system of the entire heart at the frontal plane. Also, tachycardia meets the ECG criteria for SVT with aberration, and often with signs of AV dissociation. The significance of this tachycardia lies in the fact that it can be easily eliminated by catheter ablation of the right leg of the His bundle.
PATIENTS WITHOUT STRUCTURAL HEART CONSISTENCY ARE STILL NOT AFFECTED TO RADICAL RELIEF
The mechanism of these arrhythmias is a change in ion transmembrane channels (channelopathy), or in proteins that bind potassium in the middle of the cell. The remaining time revealed a significant number of mutations.
Long QT syndrome
Long QT syndrome is characterized by increased QT interval prolongation on the surface ECG, reversal attacks of syncope, and the onset of raptoid death against the background of polymorphic TSC with characteristic circling of the RS complexes near isoelectrically and lines (torsade de pointes) (Fig. 9). The frequency of guilt syndrome is 1: 7000–1: 10,000 living children. More than 250 mutations have been described in seven genes (long QT syndrome type 1–7). 30–40% of patients do not have genetic defects, which indicates the heterogeneity of genetic loci. In some patients with prolonged QT interval, the effects of drugs are known to increase the potential for cardiac dysfunction, bradycardia or electrolyte imbalance. In case of congenital short QT syndrome, beta blockers are prescribed prophylactically. The usefulness of prophylactic implantation of cardioverter-defibrillators is considered in patients with attacks of syncope, which are not prescribed when beta-blockers are taken, or when this type of seizure is evident. in rapt death.
Figure 9.
The episode triggers tachycardia in a patient with long QT syndrome.
Short QT syndrome
Recently, a new syndrome has been described that is associated with cardiac death in patients without structural changes in the myocardium - short QT syndrome. Its width is unknown. These patients have a QT interval < 270 ms, episodes of rapid death in the family, palpitations, syncope or rapid cardiac arrest due to polymorphic CT with high heart rate. Today, the only method of therapy is implantation of an internal cardioverter-defibrillator.
Catecholaminergic polymorphic schular tachycardia
Catecholaminergic polymorphic schular tachycardia is a clinically and genetically heterogeneous disease. It is characterized by episodes of syncope or rapt death in response to physiological or emotional stress against the background of a structurally unchanged heart. Documentation may be bidirectional ST (Fig. 10), polymorphic ST, or idiopathic fibrillation of the scutula. Approximately one third of cases have a strong family history of juvenile raptoid death or stress-induced syncope. Mortality is high and reaches 30–50% before the age of 30. Approximately 40–60% of patients have mutations in genes that encode calcium binding. Current treatment includes beta-blockers, calcium channel blockers, antiarrhythmic agents and/or implantation of an internal cardioverter-defibrillator. It is important that it is empirical and based on the results of serial surgical and medical testing.
Figure 10.
Bidirectional tachycardia after stimulation in a patient with catecholaminergic polymorphic PS.
Brugada syndrome
In 1992, the Brugada brothers described a new clinical syndrome, which is characterized by RBBB and ST segment elevation in the right thoracic outlets with a high incidence of raptic cardiac death in patients with structural an unchanging heart. It manifests itself as episodes of polymorphic CV, syncope and heart palpitations in an adult (on average - in 40 years of age, and with pronounced palpitations in the eyelid). This syndrome accounts for approximately 4–12% of cases of raptovascular death and 20–40% of cases of raptovirus, hemorrhage in patients without structural heart disease. It is important that Brugada syndrome is diagnosed in humans. It is most widespread in the countries of Northern Asia and Japan, where this syndrome is the leading cause of natural death in young people (the average incidence of death is 26– 38 per 100,000). Diagnostic criteria are mainly based on electrocardiographic changes, excluding structural heart disease. Brugada syndrome is considered a “canalopathy” and is one of the representatives of the group of “primary electrical heart diseases”. Approximately 20–30% of patients with Brugada syndrome have genetic mutations in sodium channels. Electrocardiographic manifestations of Brugada syndrome may be transient or onset, but can be unmasked by sodium channel blockers (such as ajmaline and flecainide), vagotonic stimulation or during fever. The diagnostic and prognostic value of the episodic ECG sign of Brugada syndrome in asymptomatic individuals without specific family history has not yet been elucidated. Implantation of a cardioverter-defibrillator is the main method of secondary and primary prevention of rash death in patients with high risk of death.
| Wide complex tachycardia (WCT): key points • While the QRS complexes during TSC do not exhibit aberrant forms, the most common type is ventral tachycardia • Approximately 80% of all TSCs occur in schular tachycardias • In patients diagnosed with structural heart disease, there may be all types of TSC and ventricular tachycardias |
Prepared by Oleg Zharinov
Causes of ischemic disease. Warning the heart
If we consider organic lesions of the cardiovascular system, arrhythmias most often occur with ischemic heart disease, myocarditis, cardiomyopathies, heart defects, pathologies of large vessels (pulmonary embolism, aortic aneurysms), hypertension, pericarditis and heart tumors. Arrhythmias can also be observed in endocrinopathies (pheochromocytoma, thyrotoxicosis), drug intoxication (glycosides, catecholamines), acute infectious diseases, anemia, in violation of the body's electrolyte balance (especially potassium, calcium and magnesium) and other pathological conditions.
Sometimes heart rhythm disturbances also occur under the influence of exogenous factors: excessive consumption of coffee, alcohol, tobacco. Some types of arrhythmias can also develop in healthy people in response to physical activity or nervous tension.
The arrhythmic variant of IHD is spoken of only in cases where cardiac arrhythmias are the only symptom of this disease. The diagnosis of coronary artery disease remains presumptive until ECG, Holter monitoring and coronary angiography are performed, which reveal various heart lesions. However, in most patients, arrhythmias are combined with other clinical forms of IHD. Rhythm disturbances are also a common symptom of atherosclerotic cardiosclerosis, especially with angina pectoris or heart failure. However, despite the many reasons that can cause rhythm disturbances, all arrhythmias can be divided into three main groups: those associated with impaired impulse formation, those associated with impaired impulse conduction, and combined arrhythmias. Table 1 presents the classification of arrhythmias depending on the mechanism of their occurrence.
Table 1.
Classification of arrhythmias depending on the mechanism of occurrence
| Mechanism of occurrence | Impulse formation disorders | Impulse conduction disorders | Combined disorders |
| Types of rhythm disturbances | Sinus tachy- and bradyarrhythmias, sick sinus syndrome, ectopic rhythms (non-paroxysmal tachycardias), extrasystoles, ventricular tachycardias, fibrillation and flutter of the atria and ventricles | Blockades: sinoatrial, intraatrial, atrioventricular; premature ventricular excitation syndrome | Atrioventricular dissociations, ectopic rhythms with block, parasystoles* |
* Rarely encountered
The diagnosis of “cardiac arrhythmia” is always based on clinical and electrocardiographic data, and treatment includes therapy for the underlying disease and antiarrhythmic measures themselves.