What function do basophils perform in the body?
What are basophils?
Basophils are a type of white blood cell. They have a round shape. Their core is divided into segments. When stained with alkaline dyes, they acquire a dark purple color. This distinguishes them in a blood smear from neutrophils and eosinophils.
Where are they formed?
Like all blood cells, basophils are formed in the bone marrow. The precursor of basophils are basophilic myeloblasts.
All granulocytic leukocytes (basophils, neutrophils, eosinophils) have a common precursor - the myeloblast cell. From it, during differentiation, the corresponding cells develop.
Basophils are granulocytic leukocytes. This means that in the cytoplasm of these cells there are granules containing various substances.
Normal blood content
Basophils are normally found in very small quantities in the blood.
There are two ways to express the number of basophils: absolute and relative. Relative - the number of basophils and other leukocytes per 100 counted cells is calculated. Absolute – expressed as the number of cells per 10*9 per liter of blood. Normally, the relative number of basophils is 0 – 1%. Absolute – 0.01 – 0.065 per 10*9 per liter.
Main functions
The functions performed by basophils are determined by the content of their granules. The granules contain various substances, for example, serotonin, histamine, prostaglandins, in general, mediators of allergic and inflammatory reactions.
Therefore, basophils determine the development of inflammation and allergy reactions.
A general blood test in pediatrics is a mirror of a child’s health.
Timely and effective treatment of any disease always depends on a correct diagnosis. Any adult, visiting a pediatrician with their child about an illness, wants his child to recover as quickly as possible. On the other hand, it is very important for the attending physician, in addition to complaints, medical history and the objective condition of a small patient, to have data from laboratory and instrumental examinations when making a diagnosis. The most universal of them are general clinical blood and urine tests. Their value lies not only in the speed and ease of implementation, but also in the highly informative content of the results. A general blood test is always taken on an empty stomach (except in emergency cases), i.e. Before coming for the procedure, you must avoid taking any food and limit your fluid intake. Therefore, blood is taken for analysis in the morning so that the child does not have to starve for a long time. The material for analysis is blood taken from a finger or vein. The importance of this rule is due to the fact that after eating, some indicators (the level of white blood cells - leukocytes, ESR) may deviate from the norm, thereby creating a false picture of the disease. If possible, you need to prevent stress when taking blood from a child over 2 years old by talking with him the day before about the upcoming examination, encouraging him after the procedure, etc. Now for you, dear Parents, a little information about the most frequently determined indicators included in the general blood test form.
Hemoglobin is a substance that is part of red blood cells and acts as a carrier of oxygen and carbon dioxide, consists of protein and iron. Normal hemoglobin levels: – newborns – 160-230 g/l; – children under one year old – 110-130 g/l; – from one to 4 years – 110-140 g/l; – from 4 to 7 years – 110-146 g/l; – from 7 years and older – 110-152 g/l. An increase in hemoglobin levels is observed during high physical activity, excitement, stressful situations, dehydration (vomiting, diarrhea), burns and some blood diseases. A decrease in hemoglobin levels is typical for anemia of various origins, degenerative processes, and may be a side effect of certain medications.
Hematocrit is an indicator indicating what part of the blood volume is occupied by formed elements (cells). The norm for newborns is 40-60%, for children from 2 months to 4 years 30-41%, from 4 years and older 34-43%. An increase in the hematocrit level is observed with blood thickening associated with dehydration or diseases that increase the number of cells (erythremia, leukemia). A decrease in this indicator occurs with anemia.
Erythrocytes are red blood cells that contain hemoglobin. Responsible for the transport of oxygen, carbon dioxide, amino acids, antibodies, drugs and toxins. The lifespan of these cells is 120 days. Normal indicators for children: – from birth to 2 months. — 3.9-6.2 T/l; – from 2 to 4 months. — 3.1-4.5 T/l; – from 4 months to 4 years – 3.0-5.4 T/l; – from 5 years and older – 3.5-5.0 T/l. An increase in the level of red blood cells is characteristic of oxygen starvation, chronic lung diseases, congenital heart defects, some blood diseases and neoplasms. A low level of red blood cells is observed with anemia, infections, helminthic infestations, bleeding, obesity, due to increased background radiation. The cause and form of anemia can be determined by the average volume of red blood cells. For children aged 4 months to 4 years, the norm is 75-115 fL, from 5 to 7 years 76-108 fL, from 8 years and older -76-96 fL. An increase in this indicator is observed in anemia associated with deficiency of vitamin B12, folic acid, liver diseases, dysfunction of the bone marrow and thyroid gland, and after bleeding. A decrease in the indicator is characteristic of iron deficiency anemia; hyperfunction of the thyroid gland; anemia associated with chronic diseases; congenital anemias.
Leukocytes are white blood cells whose main function is to protect the body from foreign influences. Leukocytes participate in inflammatory, allergic, and immune reactions, destroying cell breakdown products, viruses and bacteria. Normal indicators: – for newborns – 13-20 G/l; – for children from 1 week to 1 month – 5-20 G/l; – for children from 1 month to 1 year – 6-15 G/l; – from 1 year to 6 years – 5-14 G/l; – from 6 years and older – 6-11 G/l. An increase in the level of white blood cells (leukocytosis) is observed after acute bleeding; for neoplasms; blood diseases; for most infectious diseases of a bacterial nature (both acute and chronic). Short-term physiological leukocytosis is provoked by food intake, pain, emotional stress, physical effort, and exposure to ultraviolet radiation. A decrease in the level of leukocytes (leukopenia) is observed in infections such as influenza, ARVI, measles, psittacosis, viral hepatitis and malaria. Long-term bacterial infections, depleting the body, also reduce the level of leukocytes. Dangerous causes of leukopenia are blood diseases, autoimmune diseases, and the consequences of exposure to radiation.
The leukocyte formula includes a group of cells of different structure and function (neutrophils, eosinophils, basophils, monocytes, lymphocytes), the quantitative determination of which provides a lot of valuable diagnostic information.
Neutrophils are the most numerous type of leukocytes. According to the degree of maturity, young, band and segmented neutrophils are distinguished. The main function of these cells is protective. Normally, the majority of neutrophils should be represented by segmented cells. The appearance of young forms and a large number of band neutrophils in the child’s blood most often indicates an acute inflammatory process. The normal content of neutrophils in the blood of a child from 4 months to 4 years is 30 - 55%, at the age of 5-7 years - 40 - 60%, 8 - 14 years - 45 - 70%. An increased number of neutrophils is observed during inflammatory processes, after surgical interventions, against the background of bacterial, fungal and some viral infections, parasitic infestations, during intoxication, blood diseases, and neoplasms. A low level of neutrophils is characteristic of anemia, acute viral and chronic infections.
Eosinophils are cells that indicate allergic reactions in the body. In children at any age, the norm is from 1 to 5%. An increase in the rate is observed in allergic diseases: bronchial asthma, urticaria, Quincke's edema, hay fever, hypersensitivity to drugs, a number of skin diseases, scarlet fever, helminthic infestations, and some neoplasms.
Basophils are participants in allergic and inflammatory reactions. Normally, the number of basophils ranges from 0 to 5% of the total number of leukocytes. Of clinical significance is the increase in the number of basophils, which is observed in allergic reactions, leukemia, lymphogranulomatosis, and decreased thyroid function. Lymphocytes are the most active cells of the immune system, taking part in all types of its activities. The level of lymphocytes changes significantly throughout a child's life: in children under 5 years of age, the number of lymphocytes normally exceeds the number of neutrophils, and after 5 years the situation changes to the exact opposite. If at the age of up to 5 years the norm is 45 - 65% of lymphocytes, then by 7 years the normal figure decreases to 30 - 55%, and then at 8 years and older to 20 - 40%. An increased number of lymphocytes in the blood is observed in most viral infections: viral hepatitis, infectious mononucleosis, whooping cough, rubella, cytomegalovirus, herpes, as well as tumor diseases. A decrease in the level of lymphocytes is characteristic of bacterial diseases, tuberculosis, systemic lupus erythematosus, renal failure, bone marrow dysfunction, and immunodeficiency conditions.
Monocytes are also immune response cells. The norm for children of any age is up to 8%. An increase in the rate is observed in viral and fungal infections, septic endocarditis, during recovery from infectious diseases, tuberculosis, neoplasms, and rheumatoid arthritis. A low level of monocytes is characteristic of leukemia, severe forms of anemia, and exhaustion of the body.
Erythrocyte sedimentation rate (ESR). The value of this indicator depends on the viscosity of the blood, the presence of normal and pathological proteins in it, and the number of cellular elements. By itself, the ESR value does not mean anything, however, in combination with other changes in the general blood test and the condition of the child, the indicator can provide very useful and necessary information. For children, the normal level of ESR is considered to be 2-10 mm/h (in newborns 1-2 mm/h, in children under 6 years old the rate can be increased to 15 mm/h). An increase in ESR is observed during infections, inflammatory diseases, anemia, tumors, and while taking certain medications. A decrease in ESR is characteristic of some types of anemia and blood diseases.
Platelets are blood platelets. The main function of platelets is to clot blood and stop bleeding. Normal values for children under 7 years of age are 150 - 400 G/l, 8 - 14 years old - 150 - 380 G/l. An increase in platelet levels is observed in cases of blood cancer, tuberculosis, rheumatoid arthritis, anemia, after surgery or physical activity. A decrease in the rate is typical for viral and bacterial infections, chronic bleeding, liver and kidney diseases, severe anemia, diseases of the immune system, tumors, congenital heart defects, and impaired thyroid function.
Dear parents, I would like to draw your attention: the limits of normal blood counts may vary depending on the laboratory that conducted the study. Therefore, always compare the results obtained with the reference values indicated in the analysis form!
The results of a general blood test can only be interpreted in conjunction with all available medical information: taking into account complaints, medical and life history, examination data, and the results of other laboratory and instrumental examinations.
Only an experienced doctor can understand such a volume of information, so be sure to discuss the results of your child’s general blood test with your pediatrician.
Be healthy!
Why are basophils elevated?
A condition where basophils are elevated is commonly called basophilia. It occurs in allergic reactions, as basophils secrete allergy mediators. Allergy can be confirmed by eosinophil levels.
Eosinophils are also a type of white blood cell containing granules. They will be increased during allergic reactions and in the presence of a parasite in the body.
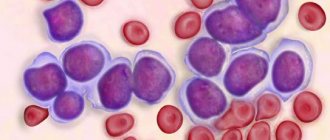
The most unfavorable cause of an increase in the level of basophils in the blood is myeloproliferative and malignant diseases. For example, chronic myeloid leukemia. It is confirmed by the presence of atypical cells in the blood, blasts. This type of leukemia is characterized by an eosinophilic-basophilic association, that is, an increase in the level of basophils and eosinophils in the blood at the same time.
Only relative numbers can indicate that basophils are elevated in a child; absolute numbers are normal. The blood should be re-donated, as there is a possibility of incorrect basophil counting.
In cases where the absolute content of basophils is increased, cell counting is not required. Specialist consultation is required.
Reasons for the increase
If basophils are elevated in a child’s blood , this may indicate a weakened immune system and the influence of negative factors such as allergens, toxins, various infections or helminths on the body. The reasons for the increase in this indicator are also diseases:
- myeloid leukemia and other blood pathologies;
- infectious diseases;
- allergic manifestations;
- inflammatory processes;
- interruptions in the functioning of the endocrine glands;
- influence of radiation;
- anemia.
When a child has elevated basophils, only a professional can identify the reasons. To establish an accurate diagnosis, it is not enough to just take a blood test - the doctor will conduct an examination and refer you for additional tests.
What analysis allows you to determine the level of basophils?
The level of basophils in the blood can be detected in 2 ways.
- A modern hematology analyzer that is capable of counting the type of granulocytes.
- Microscopic examination of a stained blood smear - calculation of the leukocyte formula.
How to prepare for analysis?
To study the level of basophils, blood is donated: venous or capillary. It is necessary to prepare for donating blood.
It is important to donate blood on an empty stomach. Infants should not be fed for half an hour before donating blood. Children under 3 – 4 years old – 4 hours. Older children are advised to donate blood after an overnight fast.
It is recommended not to stress your child. The day before the test, do not engage in excessive physical activity - live these days as usual.
If you are prescribed any medications, consult your doctor about their effect on the test results.
If a patient is prescribed any physical procedures or other research methods, first of all donate blood. For example, X-rays change the quantitative composition of blood.
The essence of the determination method
Let us dwell on the most commonly used method for calculating the number of basophils - the leukocyte formula. Its essence lies in counting 100 leukocyte cells, divided by type:
- segmented neutrophils;
- band neutrophils;
- eosinophils;
- basophils;
- lymphocytes;
- monocytes;
- juvenile forms, blast cells and so on.
That is, you can look at a blood smear and roughly imagine what is happening to the blood cells.
Where can I get tested?
Analysis of the level of leukocytes, including basophils, is included in the CBC. Therefore, it can be done free of charge under the compulsory health insurance policy (CHI) at your local clinic. This analysis can also be taken for a fee in centers equipped with the necessary equipment. The issue price is 200 – 400 rubles. In addition to this amount will be the cost of drawing blood from a vein or finger.
Indications for the purpose of analysis
Using a blood test and detecting changes in it, it is assumed that there is some pathology in the body. Sometimes analysis can reveal pathology at an early stage, when there are no main symptoms yet.
If there are clinical manifestations of the disease, the study helps to determine the nature and intensity of inflammation. The analysis is used to identify inflammatory pathologies, allergies, and blood diseases. Repeated testing allows the doctor to evaluate the effectiveness of therapy.