Eosinophils consist of a bilobed nucleus and three types of eosinophil granules (lipid bodies, eosinophils, small and primary). They contain protein structures with the help of which foreign cells are neutralized. Eosinophils are quite large cells: their diameter reaches 20 microns.
Eosinophils got their name due to the fact that when stained according to Romanovsky, they are easily stained with eosin (an acidic dye), while other types of dyes have no effect on them. Eosin itself was invented in 1873 by the German scientist G. Caro and, due to its bright pink color, was named after the ancient Greek goddess of the dawn Eos (in the German version the name sounds like “eosin”).
Blood test for eosinophils
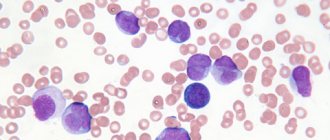
To determine the level of eosinophils, a general blood test is used, which is familiar to all of us since childhood. Eosinophils by themselves do not give an accurate idea of the nature of pathological changes in the body, however, in combination with other values of the leukocyte formula, they allow a specialist to judge the nature of the pathology. In the analysis form, eosinophils are designated as EO. Their content is indicated as a percentage of the total number of leukocytes. A formula is also used to calculate the absolute number of eosinophils in peripheral blood and it looks like this: number of leukocytes * 10 to the 9th power. For a general analysis, blood is most often taken from a finger prick, but venous blood is also suitable.
Figure 1. Causes of eosinophilia (increased number of eosinophils in the blood). Image: kavusta/Depositphotos
Forecast
It is impossible to predict the risk of certain consequences for human health and life based on eosinophilic leukocytosis in the blood alone. The prognosis is always determined by the underlying disease and the timeliness of its diagnosis - it can vary from favorable in allergic conjunctivitis to a high probability of death in malignant neoplasms or myeloproliferative pathologies. Therefore, any excess of the reference values of eosinophils in a clinical blood test requires a thorough examination to determine the cause.
Indications for analysis
A complete blood test with a count of eosinophils is prescribed for most people who visit the clinic. The range of indications is very wide, but in modern clinical practice, the initial eosinophil count is most often used as a biomarker to assess the effectiveness of drugs prescribed to patients with bronchial asthma. In this regard, the absolute number of eosinophils is of greatest value to the physician.
Eosinophils belong to microphages. This means that they can only absorb small foreign particles.
The study is relevant when confirming a preliminary diagnosis, checking the effectiveness of the prescribed therapeutic course, assessing the state of a person’s health during medical examinations or medical examinations. The doctor also prescribes a general blood test in the postoperative period. In addition, counting eosinophils is important when the development of infectious, oncological and autoimmune diseases is suspected.
Eosinophils in allergies:
It is well known that eosinophils indicate the presence of allergies; during allergic reactions, their content in the blood can increase several times relative to the norm. However, it would be a mistake to assume that they increase the allergic reaction. On the contrary, eosinophils strive to balance the disturbed balance of the immune system, in which it gives such an explosive reaction to a stimulus. For example, these cells absorb histamine, a mediator of allergies. If there is too much of it in the body, it can cause a very serious situation: anaphylactic shock, from which you can die. Eosinophils save allergy sufferers from this, as they regulate the strength of the reaction and reduce it.
Norms of eosinophils in the blood
When deciphering the analysis, the patient’s age is taken into account, since these factors affect the content of eosinophils in the blood.
Table 1. Norm of eosinophils by age
| Children under 5 years old | Children 5 – 14 years old | Adults |
| 0,5 – 7% | 1 – 5% | 0,5 – 5% |
It should also be taken into account that in women in the first days of menstruation there is a slight excess of the norm in the content of eosinophils, while after ovulation their number may be slightly below the norm.
In absolute terms, the norm for adults is 0.15-0.450X10.0⁹ per liter of blood plasma. Exceeding the normal percentage of leukocytes is called eosinophilia. There are three stages of eosinophilia:
1. Light (no more than 10% of the total number of leukocytes).
2. Average (up to 15%).
3. Heavy (over 15%).
What are eosinophils
Eosinophils are a type of white blood cell (leukocyte). They fight harmful microorganisms, mainly parasites, bacteria and protists. These foreign and dangerous cells are found in the blood and tissues of the body. Eosinophils create receptors that bind to immunoglobulin-E, and in this way create a complex that destroys the dangerous cell. This property of these blood cells is called cytotoxic.
A mature eosinophil consists of a bilobed nucleus and eosinophil granules with a diameter of 1 micron, which store proteins necessary for the destruction of the harmful cell. The diameter of the eosinophil reaches 18–20 microns, that is, the cell is quite large. The eosinophil consists of three types of granules: lipid bodies, eosinophils, small and primary granules.
Eosinophils remain in the blood for 0.5–18 hours and are then sent to the body tissues for 10–12 days. These cells are able to bind to extracellular materials and also recognize foreign bodies in the body.
Eosinophils perform many important functions:
- destruction of multicellular parasites, including helminths;
- fight viruses and protect the immune system;
- release of bactericidal substances and fight against bacteria;
- regulation of the development of sexual processes in women, including pregnancy;
- influence on the processes of tumor development and foreign organ rejection reactions after transplantation;
- participation in enhancing the immune response that T cells create.
These blood bodies get their name due to the fact that they are stained with eosin. This bright pink dye was first discovered by the German chemist Heinrich Caro in 1873. The dye is named after the ancient Greek goddess of dawn and dawn Eos. Anna Peters, the sister of one of the chemists and an acquaintance of Heinrich Karo, had the same nickname.
Causes of an increased number of eosinophils in the blood
An increase in the level of eosinophils indicates that the body is resisting the inflammatory process, and tissues and cells are experiencing oxygen deficiency. Possible reasons for the increase in the number of eosinophils:
- Allergy. This is one of the most common reasons. Hypersensitivity reactions always increase the production of eosinophils in the bone marrow. In turn, eosinophils reduce the production of allergy mediators.
Allergies are a common cause of elevated eosinophil levels. Photo: Dmyrto_Z / Depositphotos
- Asthma. In bronchial asthma, there is a moderate increase in the number of eosinophils in the blood, and in the allergic form they can also be found in sputum and bronchoalveolar fluid.
- Helminthic infestations. When infected with helminths, the number of eosinophils in the blood increases for two reasons: first, they release eosinophil cationic protein and reactive oxygen species to kill parasites. Secondly, the metabolic products of parasites provoke hypersensitivity reactions, and here the mechanism for increasing the production of eosinophils is the same as in allergies.
- Lung diseases. Despite the fact that the mechanism of increased eosinophil production in lung diseases has not yet been fully studied, experts note the relationship between these phenomena. Eosinophilia is observed in Churg-Strauss syndrome (in this case it reaches a frightening figure of 50%), allergic bronchopulmonary aspergillosis (an increase in the level of eosinophils is observed only in the acute phase and rarely exceeds 15%), as well as in eosinophilic pneumonia (up to 20%).
- Blood diseases. First of all, we are talking about hematological pathologies of a malignant nature (eosinophilic leukemia, myeloid leukemia). Eosinophilia is also characteristic of mastocytosis, but in leukemia its severity is much higher (up to 70%).
- Gastrointestinal diseases. An increased number of eosinophils in a general blood test is observed in gastritis, esophagitis and enterocolitis. All these diseases are accompanied by inflammatory processes, which causes accelerated formation of eosinophils.
- Oncological diseases. When confirming the diagnosis, the leukocyte count is not a priority indicator, but an increase in the number of eosinophils in malignant diseases is indeed observed. After therapeutic interventions such as radiotherapy, the increase in the number of eosinophils also increases significantly.
- Weakened immunity. In immunodeficiency conditions (Wiskott-Aldrich syndrome and Jobe syndrome), the level of eosinophils can reach 60%, which is associated with increased production of immunoglobulin E.
- Endocrine diseases. In diseases such as primary adrenal insufficiency (Addison's disease), congenital adrenal dysfunction, Schmidt's syndrome and panhypopituitarism, eosinophil levels increase to moderate levels and normalize after treatment with glucocorticoids.
- The recovery period after surgery. This is especially true when transplanting donor organs to a patient and removing the spleen.
Correction
Self-correction of eosinophilia is impossible. To normalize the level of eosinophils, it is necessary to combat the cause. If eosinophilia is mild, is associated with taking drugs or vaccination, or occurs during the period of convalescence, there is no need to worry. It is necessary to observe the blood dynamics after 7-10 days. If persistent or high eosinophilia is detected in a blood test, you should contact a specialist so that, based on examination, complaints, and medical history, he can conduct a diagnostic search for the etiological factor and prescribe appropriate treatment. To treat most diseases accompanied by eosinophilia, drugs from the group of antihistamines or glucocorticosteroids are used.
Causes of a low number of eosinophils in the blood
A decrease in the number of eosinophils below 0.02*109/l is called eosinopenia. There are several possible reasons:
- Taking glucocorticoids and steroids. These are hormonal drugs that help reduce the number of leukocytes (including eosinophils) in the blood due to their destruction. At the same time, eosinopenia is not a strong enough reason to discontinue a course of glucocorticoids, since in itself it does not pose a threat to health, while the therapeutic effect of these drugs for allergic reactions or autoimmune diseases fully justifies their use.
- Nervous tension and stress. During times of severe mental stress, depression and emotional turmoil, the level of cortisol, which is called the stress hormone, increases in the blood. It is cortisol that destroys eosinophils.
- Allergic reactions. The level of eosinophils in allergies is a rather paradoxical issue. With moderate hypersensitivity reactions, eosinophilia is observed, but with severe allergies, the level of eosinophils, on the contrary, decreases.
- Infectious diseases. Eosinopenia is characteristic of diseases of a viral and bacterial nature, which include coronavirus infection. A decrease in the number of eosinophils is also observed in purulent-septic processes (abscesses and phlegmon).
- Endocrine diseases. As we already know, an increase in the level of cortisol in the blood entails a decrease in the number of eosinophils. Cortisol is produced in the adrenal glands, so adrenal diseases (for example, Cushing's syndrome) cause eosinopenia.
- Bone marrow diseases. Since eosinophils are formed in the bone marrow, any associated pathologies and injuries cause eosinopenia.
- A decrease in the level of eosinophils in the blood can also be observed in the first days after a heart attack, with appendicitis, sepsis, acromegaly, lupus erythematosus, burns and injuries.
Figure 2. Eosinopenia (low eosinophil count). Dr Graham Beards / Wikipedia (CC BY-SA 3.0)
Why basophils may be elevated
Basophilia is diagnosed when the number of cells exceeds 0.2*109 /l. The use of drugs with estrogen hormones, as well as the use of thyreostatic drugs, can distort the picture. An increase in the rate is observed at the beginning of the menstrual cycle in women.
Basophils are increased:
- for chronic diseases of the gastrointestinal tract: inflammation of the gastric mucosa, enterocolitis, ulcerative inflammation of the large intestine, ulcerative lesions of the stomach and duodenum;
- at the stage of weakening of acute symptoms of an infectious disease;
- for blood diseases: acute form of leukemia, chronic myeloid leukemia, anemia, polycythemia, hemophilia, lymphogranulomatosis;
- for allergies and diabetes;
- with a decrease in the hormonal activity of the thyroid gland - hypothyroidism;
- oncology of the lymphatic system, blood cancer, lung cancer;
- due to prolonged exposure to low doses of radiation.
The main reasons for the increase in the indicator are a violation of immune defense and active invasion of the pathogen. In an adult, basophils may be elevated after removal of the spleen.
A child's concentration may increase:
- due to taking medications that cause allergies;
- due to a hidden inflammatory process;
- due to a recent vaccination or mosquito bite that gives rise to allergies;
- due to the introduction of foreign proteins.
To exclude pathology, a repeat analysis is recommended a week after the cessation of the above reasons. If the indicators are high again, a comprehensive examination is prescribed to identify the exact cause.
Consequences of deviation from the norm
A change in the normal level of eosinophils in the blood is not a criterion by which one can get an idea of possible pathological changes in the body. Simply put, the level of eosinophils in the blood itself means little - you need to pay attention to the disease that caused its change. Therefore, the consequences can be very diverse - from completely insignificant (as in the case of physical activity) to deadly (for example, in the case of oncology).
Eosinophilia itself, in rare cases, can lead to damage to tissues in which the greatest accumulation of eosinophils is observed. The mechanism of such damage has not been fully studied to date, but it has been established that eosinophils exhibit the most severe damaging effect in conditions such as eosinophilic fibroplastic endocarditis and idiopathic hypereosinophilic syndrome. The nature of the damage directly depends on the duration of eosinophilia and the severity of eosinophilic tissue infiltration.
Eosinophils and phagocytosis:
The entire immune system is mobilized to protect health, and each of its elements works in its own way. The eosinophil count also increases when any harmful object enters the body. Eosinophils have a clear reaction to the “enemy”: to fight it, they turn into phagocytes and devour foreign particles.
Unfortunately, they are not able to cope with all possible aggressors; These cells are powerless against especially large objects. However, they are capable of neutralizing small particles (viruses, small bacteria, molecules of toxic substances). Like full-fledged phagocytes, they approach the object of attack, capture it with their pseudopods, “swallow” and digest it. The destruction of the object occurs thanks to the enzymes contained in the lysosomes of eosinophils. Because the ability of eosinophils to phagocytose depends on the size of harmful particles, these cells are classified as so-called microphages.
Despite the fact that when describing the function of eosinophils, the ability indicated above is always mentioned, their main significance is not the absorption of microbes. What?
How to reduce the number of eosinophils in the blood
Eosinophilia is not an independent nosological entity, but only a consequence of a particular disease. Therefore, it cannot be treated in isolation - first of all, it is important to eliminate the cause of its occurrence, that is, the disease that caused the change in the leukocyte formula.
Possible treatment options:
- Desensitizing therapy. For allergies, antihistamines are used to reduce hypersensitivity reactions. Some of them may cause mild drowsiness (for example, chloropyramine), but newer generation drugs such as cetirizine, levocetirizine, desloratadine and rupatadine do not have this side effect and have a mild anti-inflammatory effect.
- Antibacterial therapy - for infectious diseases, antibiotics are prescribed (amoxicillin, ceftriaxone, azithromycin, erythromycin, etc.). The choice of antibacterial drug depends on the pathogen and its sensitivity to a specific group of antibiotics.
- Anti-inflammatory therapy. An increase in the level of leukocytes (including eosinophils) is observed during inflammatory processes. When they are severe, glucocorticosteroids (prednisolone) are used.
- Chemotherapy. This treatment method is aimed at eliminating malignant tumors. For this purpose, cytostatics and antimetabolites are used.
- Hormonal therapy. For multisystem diseases accompanied by immunodeficiency (for example, Jobe's syndrome), the use of steroid drugs and interferon gamma is indicated. Treatment is supplemented with antibiotics, calcineurin inhibitors, H1-histamine blockers, and antifungal drugs.
- Antihelminthic therapy. To combat helminthic infestations, drugs such as albendazole, levamisole, bephenia hydroxynaphthoate, piperazine, tetrachlorethylene, and mebendazole are prescribed. The choice of medication depends on the type of parasite and the stage of infestation. Additionally, antibiotics, enterosorbents, enzymes, probiotics, and glucocorticoids are prescribed.
Additionally, the following measures can be taken:
- Normalize your lifestyle. It is important to avoid frequent drinking of alcohol and give up cigarettes (or at least significantly limit the number of them).
- Avoid chronic intoxication. In people working in hazardous industries or living in environmentally unfavorable regions, the number of eosinophils in the blood increases as a result of constant chemical intoxication.
- Maintain a healthy diet. You should not overuse spicy, smoked, canned and fatty foods. To increase the level of eosinophils, you should limit the amount of meat, poultry and fish in your diet (consume mainly low-fat varieties). The menu should include yogurt, cheeses, vegetables, fruits, beans, bran and whole grain bread.
Giving up bad habits will help normalize the level of eosinophils. Photo: vgstockstudio / freepik.com
Classification
Today, there are two main classifications of eosinophilia - according to the level of increase in eosinophils and according to the etiopathogenetic factor. Based on the number of cells, the following eosinophilias are distinguished:
- Lungs
. Eosinophil level from 500 to 1500. - Moderate
. The concentration of eosinophils is from 1500 to 5000. - Expressed.
The content of eosinophils is more than 5000. They are most typical for helminthiases and hematological diseases.
Moderate and severe eosinophilia are combined under the term hypereosinophilia. According to the pathophysiological mechanism, eosinophilia is divided into:
- Clonal.
Eosinophils are part of the malignant clone. Occurs in myeloproliferative hemoblastoses (leukemia), systemic diseases of mast cells (mastocytosis). - Reactive.
The general mechanism of occurrence is the overproduction of interleukin-5 by T helper cells, which stimulates the bone marrow production of eosinophils. They develop as a response to various external influences on the macroorganism - allergens, parasitic infestations, etc. They make up about 90% of all eosinophilias.
Separately, transient (short-term) eosinophilia is distinguished, which is not directly related to specific diseases. The number of eosinophils may increase with the use of certain medications (antibiotics, anti-tuberculosis drugs), administration of the hepatitis A vaccine, hemodialysis, or exposure to local radiation therapy. The exact pathophysiological mechanism of the increase in eosinophils under these circumstances is unknown.
How to increase the number of eosinophils in the blood
A decrease in the level of eosinophils in the blood is a sign of weakened immunity. As in the case of eosinophilia, the primary pathology should be identified and eliminated, as well as lifestyle adjustments: minimize bad habits, ensure an adequate level of physical activity, and also take care of a normal daily routine (it is important to sleep at least 8 hours a day) .
The normalization of the leukocyte formula is facilitated by the consumption of vitamins B12, C, D. They can be obtained from food (meat, fish, cottage cheese, rose hips, currants, garlic), or from pharmacy multivitamins. It is advisable to exclude foods with a high allergenic potential: milk, soy, wheat, eggs, seafood, peanuts.
When treating diseases that result in eosinopenia, the same groups of drugs are often used as in the case of eosinophilia. For example, antibiotics are prescribed for infectious diseases, as well as diffuse and localized purulent-inflammatory processes (cellulitis and abscess). As mentioned earlier, allergies can provoke not only an increase, but also a decrease in the number of eosinophils in the blood, so antihistamines can also be used in the treatment of eosinopenia.