BABUNASHVILI AVTANDIL MIKHAILOVICH
, Doctor of Medical Sciences, Professor of the Department of Hospital Surgery of the RUDN University, Head of the catheterization operating room of the Center for Endosurgery and Lithotripsy Since 1986, he has been actively involved in the development and implementation into clinical practice of new, progressive minimally invasive methods for the treatment of diseases of the cardiovascular system, in particular, coronary heart disease and acute infarction myocardium, malformations of the heart and its valve apparatus. He is one of the leaders in the field of domestic minimally invasive endovascular surgery.
Performed for the first time in Russia
- laser angioplasty for stenotic and occlusive lesions of the coronary arteries of the heart in ischemic heart disease - February 1989
- removal of a foreign body from the lumen of a coronary artery during a complicated angioplasty operation - April 1991
- stenting of the coronary artery for atherosclerotic lesions of the coronary artery – January 1992
- implantation of an original device to close a cardiac septal defect – March 1995
- retrograde recanalization through the collateral canal of a blocked coronary artery – September 2006
- hydrodynamic recanalization for coronary artery occlusion – March 2007
Experience in endovascular operations for coronary artery disease and structural pathologies of the heart - more than 6,000 successful operations!
Types of cardiac arrhythmias
“Arrhythmia” literally means “lack of rhythm.” This term combines heterogeneous pathologies of the conduction system of the heart, in which the heart rate, rhythm and sequence of contraction of various parts of the myocardium can be disrupted. The classification of myocardial contraction rhythm disturbances is quite complex. Arrhythmias are distinguished: • by the localization of pathological pacemakers, • by the level of blockade of impulses, • by the type of heart rate disturbance, etc. • according to the mechanism of development of arrhythmia, they are divided into four groups: 1. Automatism disorders - pathology of the sinus node as the main pacemaker. 2. Excitability disorders - the occurrence of pathological pacemakers that cause extraordinary contractions (extrasystole) or even attacks of non-sinus rhythm (paroxysmal tachycardia). 3. Conduction disturbance – blockade of impulse conduction or impulse conduction along an abnormal path (DAVC, WPW syndrome as a special case). 4. Mixed forms of violation .
Scientific work
Author of more than 200 scientific papers
printed works, including in foreign scientific medical journals (American Journal of Cardiology, Eurointervention, European Heart Journal).
Author of 2 monographs and 7 chapters in monographs, including one monograph published in France together with prof. Martial Hamon. Under the leadership of Babunashvili A.M. 3 candidate's dissertations were defended. Member of the Board of the Russian Society of Interventional Cardiangiologists
, Head. Section of the Russian Therapeutic Society, member of the editorial board of the international journal of interventional cardioangiology.
Sphere of professional interests
Area of professional interests: minimally invasive endovascular surgery of the heart and blood vessels:
- endovascular operations for chronic blockages of the coronary arteries of the heart, including using the latest technologies
- endovascular operations for valvular heart pathologies
- combined endovascular operations for atherosclerotic lesions of peripheral and coronary arteries
- minimally invasive procedures for structural pathologies of the heart (oblation of septal branches in hypertrophic cardiomyopathies)
- endoprosthetics of the coronary arteries of the heart
How it all began . . .
1988 He performed his first operation on the coronary arteries of the heart as a clinical resident at the All-Union Scientific Center of Surgery of the USSR Academy of Medical Sciences, under the guidance of prof. Rabkina I.Kh. After a successful start, further intensive development of new minimally invasive methods of treating coronary heart disease and structural pathologies. The first operation using a laser beam and the thinnest light guide to eliminate atherosclerotic lesions, first during coronary bypass surgery, then using a puncture (puncture) in the femoral artery.
Then there was an unexpected twist.
It’s not for nothing that they say that sometimes incidents can decide the rest of your life. 1993 Bronstein A.S. was present during the operation of the young patient. and after a successful operation and discharge of the patient, a week later a phone call came with an invitation to establish a minimally invasive cardiac surgery service at the Center headed by Alexander Semenovich. It must be said that the surprise of the proposal set in complete stupor, because there was also a good prospect on the basis of the All-Russian Research Center for Surgery. However, I preferred more “creative freedom” and would like to test my strength in establishing a full-fledged minimally invasive cardiology service. Further events developed quite intensively, the defense of a doctoral thesis, two monographs, organization and participation in 6 Russian symposia, the first operations “live” with transmission to the meeting room, where there were colleagues taking part in scientific conferences. The first operations performed abroad (in particular, at the onze lieve vrouwe Gathius hospital in Amsterdam with Prof. Kiemeneij F.), participation and presentation of reports on our achievements in the field of minimally invasive cardiology at numerous international prestigious symposia and conferences (such as EUROpcr in Paris and Barcelona, TCT in the USA and South Korea, CCT in Japan, etc.). Participation in more than 10 international clinical studies. First stent.
. . Nowadays, implantation of prostheses (stents) into the coronary arteries of the heart has become commonplace, but in the early 90s, implantation of an artificial prosthesis into the artery of the heart seemed as fantastic as flying to the moon. . . Some said that this was very dangerous, since it increased the risk of a blood clot in the artery, with clear results, others doubted the effectiveness of these prostheses themselves. But, nevertheless, progress cannot be stopped.
One day at the beginning of 1992, almost immediately after the New Year holidays, Professor Yu.V. Tarichko came up to me, then we worked together at the Russian Surgery Center of the Academy of Medical Sciences, and said that his good friend, a researcher at one of the universities in Moscow, was suffering angina pectoris and he should be examined. After performing a diagnostic coronary angiography, he found himself with a rather dangerous lesion - an almost critical narrowing of the largest artery of the heart, the closure of which could lead to catastrophic consequences. We discussed the situation and treatment tactics together with surgeons and cardiologists and decided to perform balloon angioplasty (expansion and elimination of narrowing with an inflated balloon). At that time we had the largest experience in balloon coronary angioplasty in Russia (more than 700 operations). So, on January 24 we took it to the table and... . . During balloon angioplasty, a detachment of the inner surface of the vessel occurred (the so-called dissection of the vessel wall) with almost complete blocking of blood flow in the artery. You can imagine the situation in the operating room; there was no panic, but the situation seemed insoluble. The patient could not have been kept until the open bypass operation, since it took about 40-50 minutes to prepare the operating room for the open operation and during this time the heart could stop; there were no other ways to save the situation with the help of surgery at that time; it remained to be treated with medications unknown and absolutely unguaranteed outcome, and nevertheless, resuscitation measures were started, stress reigned in the operating room, dangerous rhythm disturbances had already begun, defibrillation twice.
Resuscitators were preparing for intubation and external cardiac massage. Prof. stood next to me. Tarichko, watching this picture, apparently regretted in his heart that they had made such a decision regarding the treatment of his friend. And suddenly it dawned on me: we have an intravascular coronary prosthesis, then this sample was given to me from Johnson & Johnson for testing. It was a Palmaz-Shatz prosthesis, which by that time was installed in only 2 or 3 clinics in the world. But in Russia, no one has ever implanted a stent! And we took a risk, because the situation was practically critical. . Preparation for implantation, as I was later told, took only 5 minutes. . I was stressed and just lost track of time. But I clearly remember the moment of control angiography after implantation, blood flow was restored, the artery was completely filled with blood, the heart began to contract at full strength, the rhythm had improved. The first feeling was that a person had been saved from an inevitable outcome. The first stent in Russia turned out to be so lucky.
By the way, this patient is still alive and well, 18 years have passed!!! and there is reason for pride - the patient was not only saved, but also given 18 years of comfortable life. What could be even better for a surgeon?
Causes of cardiac arrhythmia
The most common cause of the development of heart rhythm pathology is organic damage to the myocardium, which occurs due to heart defects, degenerative processes in the heart muscle (cardiomyopathy), and complications of coronary artery disease (myocardiosclerosis, myocardial infarction). Functional disorders in myocarditis and myocardial dystrophies, which are reversible, can also lead to rhythm pathology. Non-cardiac causes of cardiac arrhythmias include: • diseases of the thyroid gland; • pathology of the adrenal glands; • diseases of the nervous system; • metabolic disorders of potassium, calcium, magnesium; • drugs (cardiac glycosides, diuretics, sympathomimetics). Arrhythmia in a healthy person can be triggered by injury, high fever, oxygen deprivation, drinking coffee, tea, alcohol, drugs, and smoking. If the cause of the rhythm disturbance cannot be found, they speak of idiopathic arrhythmia.
Weekdays . . .
It’s not for nothing that cardiovascular disease is called the No. 1 killer. In all civilized countries they are the main cause of disability and mortality, and in Russia more than a million people die from heart and vascular diseases every year! Therefore, it is easy to imagine the intensity of patients with this pathology coming to us. At the same time, the disease spares neither the old nor the young. Every year we perform more than 600 operations for minimally invasive treatment of atherosclerosis of the coronary arteries of the heart in angina pectoris and coronary heart disease, in acute myocardial infarction. In addition, we perform operations on the carotid, renal, peripheral arteries and much more. Our main achievement is the optimization of care for vascular diseases of the heart. Thus, a diagnostic study (coronary angiography) is performed on an outpatient basis (maximum delay in hospital is 2 hours), recently the so-called computer multilayer angiography, which takes only 15 minutes. The operation is performed on the day of admission, and the patient is discharged within a day, starting normal life and work without a rehabilitation period!! People often ask what is better: coronary artery bypass grafting or minimally invasive angioplasty and stenting. With incomparably less surgical trauma, angioplasty and stenting provide the same result in the vast majority of patients as coronary artery bypass grafting. Moreover, the effect persists long after the operation for 5 years or more! And in case of acute myocardial infarction, angioplasty is generally a recognized method of choice for treatment, giving better immediate and long-term results than other treatment methods. In general, I think that minimally invasive (endovascular) treatment is the future. Indeed, in addition to the attractiveness of the method (minor surgical trauma, without opening the chest and other cavities, without anesthesia, there is no need for special rehabilitation), angioplasty is also the most “science- and technology-intensive” method. It is amazing how quickly more and more high-tech diagnostic and treatment methods are appearing. . here is a miniature ultrasound sensor, being inserted into the lumen of the artery and transmitting from there a “report” on the state of the lumen of the artery, here is an optical coherence tomograph, which gives a comprehensive description of the wall and lumen of the artery and allows a comprehensive assessment of the result of the operation and implantation of the prosthesis into the lumen of the artery, and intravascular angioscope and much more. Further, apparently, there will be robotic assistants, three-dimensional imaging of the artery, magnetic navigation inside the lumen of the artery, implantation of heart valves without opening the chest (surgery is still considered the only non-alternative operation). The development prospects are truly impressive.
The most common rhythm disorders
1. Sinus disorders
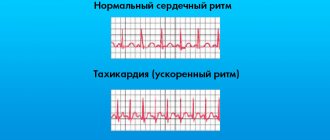
The most common type of cardiac dysfunction is sinus tachycardia , which is diagnosed when the resting heart rate (HR) increases from 100 beats per minute or higher. Rapid heartbeat naturally occurs in response to increased nervous or physical stress, as well as when taking tonic drinks (coffee, tea, alcohol), so the influence of these factors should be excluded during diagnosis. Sinus bradycardia is said to occur when the primary pacemaker provides a rate below 60 beats per minute. Low heart rate (30-50 beats at rest) can occur in trained people. This condition is considered normal if there are no symptoms of oxygen deficiency (weakness, headache, dizziness). Sinus arrhythmia of the heart is a violation of the rhythm of contractions while maintaining sinus rhythm. Doctors consider a variant of the norm to be a respiratory arrhythmia, common among adolescents, characterized by an increase in heart rate during inspiration.
2. Paroxysmal tachycardia
Paroxysmal tachycardia (PT) is attacks of rapid heartbeat (130-220 beats per minute), which suddenly occur and also suddenly stop. The duration of the attack ranges from several minutes to several days. Sustained paroxysmal tachycardia, which lasts weeks or months, is extremely rare, although cases of attacks lasting more than one year have been described. The mechanism of development of paroxysmal tachycardia is the formation of a pathological path of electrical impulse, which “interrupts” the signals of the sinus node and causes an attack. Based on the location of the area that generates the pathological rhythm, supraventricular and ventricular paroxysmal tachycardias . Supraventricular ATs are often functional in nature, while ventricular ATs most often develop against the background of organic myocardial lesions.
3. Atrioventricular block
Atrioventricular block is a cardiac arrhythmia associated with a disturbance in the conduction of impulses through the atrioventricular node. There are three degrees of severity of pathology. The first degree of blockade is asymptomatic; the diagnosis is established based on ECG data, which will show an increase in the time of impulse transmission. The second degree is characterized by the loss of individual waves of excitation; the clinical picture depends on the ratio of the dropped and “broken through” impulses. The third degree is a complete block, in which the impulses generated by the sinus node do not reach the ventricles. At the moment of complete blockade, cardiac arrest may occur, but most often the underlying structures take over the function of the pacemaker and the heartbeat resumes. With complete atrioventricular block, the heart rate decreases to 45 or even 20 beats per minute, depending on the location of the new pacemaker.
4. Atrial fibrillation (atrial fibrillation)
Atrial fibrillation develops by a mixed mechanism . The pathology is based on the emergence of several pathological pacemakers that generate excitation impulses circulating through the atria. As a result, a chaotic contraction (fibrillation) of the atria occurs with a frequency of 350-600 per minute. Under such conditions, the atrioventricular node allows only the strongest impulse waves to pass through. According to the frequency of ventricular contractions, they are distinguished: • tachysystolic forms (over 90 beats per minute); • bradysystolic forms (below 60 beats per minute); • atrial fibrillation with a normal heart rate (normoform)
Atrial fibrillation can occur in the form of suddenly occurring and suddenly ending attacks ( paroxysmal atrial fibrillation ), as well as in the form of chronic atrial fibrillation . The risk of developing this type of rhythm disorder increases with age.
If there is pain in the chest. . .
What to do? The eternal Russian question. My advice is, don’t be patient, don’t engage in self-diagnosis or self-medication, and, most importantly, God forbid you ignore them, they say they will go away on their own, it’s temporary. This could end badly!!! According to statistics from the American Heart Association alone, up to 1 million cases of sudden circulatory arrest are recorded annually in the USA (1 every 33 seconds!!), which in 75% of cases is caused by diseases of the artery of the heart. Therefore, there are defibrillators hanging everywhere in crowded places!!! For quick and effective restoration of heart rhythm and function. But while our emergency care for acute cardiac situations is not so clearly established, do not test yourself, CHEST PAIN CAN VERY OFTEN SIGNAL ABOUT HEART ARTERY DISEASE!!! Therefore my advice. It is most reasonable to seek a consultation, let the doctor rule out the “heart cause” of chest pain, but at least you will have peace of mind. More specifically, I would advise you to undergo an examination of the arteries of the heart - called CORONAROGRAPHY!. It can be done in two ways: either using modern multi-slice computed tomography or by probing the heart artery using thin catheters (probes). In both cases, the procedure is diagnostic, performed on an outpatient basis and takes no more than 10-20 minutes!! you will receive comprehensive information about the condition of your heart arteries, and at least you will know how to continue living. After all, if you know, it means you are calm and confident.