Laser therapy: what is it?
Diseases of the heart and blood vessels are treated in the department using different methods. Laser therapy is a highly effective and painless type of treatment that uses laser irradiation as the main active factor.
In medicine, laser therapy in the red and infrared ranges is most widespread. The red ray penetrates tissue depths of several millimeters, while the infrared ray can penetrate to a depth of several tens of millimeters. This irradiation is low-intensity and does not heat the tissue exposed to the laser.
The laser can be used to irradiate pathological areas either in contact with the problem area or at a distance. Intravascular laser therapy is also used.
The high effectiveness of laser therapy is explained by the powerful positive effect of laser radiation on vascular and blood cells.
The use of laser therapy leads to improved blood circulation, elimination of vascular spasms, improvement of their tone and blood flow in them, and relief of inflammatory processes. After laser irradiation sessions, processes in the heart muscle are normalized, and blood microcirculation is significantly improved.
Atrial fibrillation classification (ESCGuidlines):
- The paroxysmal form is a sudden onset of AF, lasting from several minutes to 7 days, recovering on its own (usually within 24-48 hours).
- The persistent form is atrial fibrillation lasting from 7 days to 1 month. It does not recover on its own, but there are indications and the possibility of cardioversion.
- Long-term persistent form - atrial fibrillation lasting more than 1 month, persisting or relapsing, despite attempts at cardioversion.
- The permanent form is atrial fibrillation in which cardioversion is contraindicated, was not performed, or was unsuccessful.
The prevalence of atrial fibrillation is 6% in elderly and senile people and about 2% among the entire population. In 6-10% of patients with coronary artery disease, the disease is complicated by atrial fibrillation, and in patients with mitral heart disease who require surgical treatment, atrial fibrillation develops in 60-80% of cases. Observations indicate a significant increase in the incidence of this arrhythmia.
In patients with atrial fibrillation, mortality is approximately 2 times higher than in patients with sinus rhythm. Dissociation of the atria and ventricles leads to a decrease in cardiac output by 20-30% due to the lack of atrial contribution to cardiac output, as well as inadequate filling of the left ventricle with blood. Thus, long-term atrial fibrillation leads to the development of dilated cardiomyopathy, which is accompanied by dilation of the cavities of the heart, severe systolic dysfunction of the left ventricle (decreased ejection fraction), the occurrence of mitral and tricuspid regurgitation (reverse reflux of blood), which leads to an increase in heart failure.
The presence of atrial fibrillation leads to blood stagnation and thrombus formation in the left atrial appendage with a high risk of blockage of the arteries of the brain, the main arteries of the upper and lower extremities (systemic circulation), and the vessels supplying internal organs. Every sixth stroke occurs in a patient with atrial fibrillation. The risk of such a complication in patients with atrial fibrillation is 5 to 7 times higher than in people without arrhythmia. In patients with heart defects of rheumatic etiology, complicated by atrial fibrillation, the risk of developing acute cerebrovascular accident (ACVA) is 17 times higher than in patients without atrial fibrillation.
Diagnostics
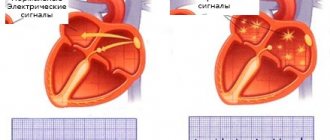
The main method for diagnosing atrial fibrillation is electrocardiography (ECG) and Holter monitoring - continuous long-term (for 1 - 7 days) ECG recording.
If the diagnosis of AF is confirmed and indications for endovascular catheter ablation of AF are determined, the patient undergoes an electrophysiological study (EPS) to identify zones of ectopic foci and construct a map of these zones.
Diseases of the heart and blood vessels treated with laser
The laser therapy method is intensively and purposefully used in cardiology, as it has a wide range of effects on blood vessels and the heart.
In our department, laser therapy is used for the following vascular and cardiac pathologies:
- Coronary heart disease (acute, chronic)
- Angina pectoris
- Vegetative-vascular dystonia
- Hypertonic disease
- Atherosclerosis
- Arrhythmias
- Peripheral vascular diseases
Only a department specialist can prescribe laser irradiation. To determine exactly how much laser exposure is required for your specific case, the department uses special technology that can measure certain parameters of red blood cells.
In case of IHD in the chronic or acute stage, the effect of laser irradiation is multicomponent. Thanks to laser therapy, the ischemic area decreases and the heart’s resistance to hypoxia increases. Laser irradiation relieves heart pain and normalizes arrhythmias. The dosage of antianginal drugs after a laser course can be reduced. Attacks of angina become less frequent, and sometimes stop completely, the speed of blood circulation increases, as does the contractility of the heart, which leads to the restoration of the functions of the heart muscle.
Drug treatment for hypertension mostly removes the external manifestations of the disease, without eliminating its cause. After laser therapy sessions, the blood carries and binds oxygen much better, so much more of it enters the heart and brain than usual. The use of a laser to treat hypertension significantly improves the patient’s condition: headaches appear less frequently or disappear, dizziness and discomfort in the heart area may also cease. Blood pressure indicators change significantly for the better, which makes it possible to reduce the number of antihypertensive drugs.
In the case of atherosclerosis, laser irradiation normalizes blood clotting, which can prevent the formation of blood clots in blood vessels. The laser also affects smooth vascular muscles, so blood flow increases, more oxygen enters the tissues, all metabolic processes are normalized, ischemia is reduced, heart pain goes away, and damaged vessels are restored. Atherosclerotic processes leading to vascular damage are inhibited.
Non-invasive low-intensity laser therapy is effective for angina pectoris: it produces an antianginal effect, after the procedures the doses of special medications are usually reduced.
Laser therapy is an excellent way to prevent strokes and heart attacks.
The vessels are cleansed of cholesterol deposits, strength and elasticity return to them, and blood flow is normalized.
Radiofrequency ablation of the heart
The invention and active introduction into widespread practice of minimally invasive interventions with maximum effect is the main path of development of modern medicine. Radiofrequency catheter ablation refers to precisely such operations.
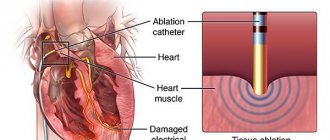
RFA is a technique for treating cardiac arrhythmias by physically destroying the focus of pathological excitation or areas of abnormal impulse conduction.
This operation made it possible to abandon complex open-heart surgery in the treatment of many types of arrhythmias, including those resistant to drug therapy.
Indications for surgery
Radiofrequency catheter ablation of the heart is the option of choice in the treatment of arrhythmias in young patients, as it allows in a relatively short time not only to improve the patient’s well-being and quality of life, but also to reduce the risks of sudden cardiac death and disability.
Pathologies for which doctors strongly recommend RFA of the heart:
- Atrial fibrillation with ventricular tachysystole.
- Paroxysmal atrial tachycardia.
- Wolff-Parkinson-White syndrome.
- Paroxysmal ventricular tachycardia.
- Arrhythmic disorders associated with cardiomyopathies.
- The presence of additional pathways, subject to a family history of sudden death.
- Intolerance or serious side effects when taking traditional antiarrhythmics.
- Tachyarrhythmias resistant to drug therapy.
If absolutely necessary, RFA can be performed even on children without congenital heart defects, starting from an early age. In this case, the indications for RFA surgery will be the development of tachycardia-dependent cardiopathy with a decrease in the pumping function of the heart and the lack of the desired effect after the use of all groups of antiarrhythmic drugs.
It is worth noting that for a number of arrhythmic disorders, radiofrequency ablation of the heart is recommended even if the patient does not want to take antiarrhythmic drugs for life or does not tolerate them well.
8
24/7
Purpose of the operation
The goals pursued when performing RFA of the heart are always aimed at eliminating the cause of arrhythmogenesis - a pathological conduction pathway or an abnormally active area of the myocardium. To do this, during cardiac ablation, a targeted destruction of a malfunctioning section of the cardiac conduction system is performed, which can have two different effects, each of which is optimal for its own group of heart pathologies. Thus, in the treatment of atrial tachycardia with anomalies of AV conduction, the method of choice is complete or partial radiofrequency ablation of the atrioventricular junction. At the same time, in the case of ventricular tachycardia or the presence of bypass paths, RFA will be aimed at destroying the most pathological area of the heart.
Radiofrequency catheter ablation of the heart allows you to avoid a number of negative consequences of living with arrhythmia, such as:
- high risk of early and sudden death from arrhythmia;
- ischemic stroke;
- myocardial infarction;
- expansion of the cavities of the heart with subsequent development of heart failure;
- long-term use of a large number of medications;
- progressive decrease in working capacity;
- high risk of death for the mother during pregnancy (for some types of arrhythmias this is an indication for abortion).
Types of RFA
Since the principle of catheter ablation is to destroy a small area, all types of this procedure differ in the physical factor causing destruction:
- radiofrequency ablation;
- electroablation;
- Ultrasonic destruction;
- laser cardiac ablation;
- cryodestruction.
However, the effectiveness, controllability of destruction and implementation features for these methods are not the same. Nowadays, RFA is most often used, since it is this technique that has produced the largest number of positive results. Whereas, for example, most cardiac surgeons are moving away from ablation with direct electric current in favor of RFA of the heart and other techniques.
Preparation for surgery, necessary tests and examinations
Before the operation, when communicating with the cardiac surgeon who will perform radiofrequency ablation of the heart, it is necessary to clearly state the list of medications taken by the patient and their dosages. It is also important to provide your doctor with information about the presence of an implanted pacemaker, allergic reactions or intolerance to medications, if any.
The list of mandatory diagnostic procedures before cardiac ablation includes the following:
- General clinical blood test.
- Biochemical studies of venous blood: bilirubin and liver enzymes, glucose, creatinine and urea with GFR calculation, total protein, etc.
- Coagulogram.
- General urine analysis.
- Electrocardiography.
- Holter (24-hour) ECG monitoring.
- Echocardiographic study.
Also, in the presence of concomitant pathology, in addition to routine methods, additional tests and diagnostic procedures may be required. For example, patients with coronary artery disease may be prescribed a lipid profile, and patients with diabetes mellitus may be prescribed a study of the level of glycated hemoglobin. It is important to consider that many patients with arrhythmias receive anticoagulant therapy, so an INR study may be added to the above.
It is recommended not to take food or water the day before RFA (at least 12 hours).
Method of operation
When performing radiofrequency ablation, general anesthesia is not required, so the patient is only anesthetized at the insertion site of the catheter electrode and is also prescribed sedatives. Already in the operating room, stable venous access is provided: it will be needed for the administration of contrast agents, antiarrhythmics or other drugs that may be needed during RFA of the heart.
The main instruments of the team of electrophysiologists and cardiac surgeons are flexible catheter electrodes. They are introduced through a large vessel, preferably through the femoral artery. Other options for introducing electrodes, for example, through the subclavian vein or other vessels, are not excluded. Radiofrequency ablation is performed under fluoroscopy guidance, so the patient does not have to worry that cardiac surgeons are operating blindly.
Typically, RFA surgery is performed in two stages:
- Performing an electrophysiological study.
- Actually radiofrequency ablation.
In the case when pathology (for example, atrial fibrillation) requires destruction of the atrioventricular connection, then another stage is added - implantation of a pacemaker, since with such ablation of the heart the conduction of impulses from the tissues of the atria to the myocardium of the ventricles completely stops.
An electrophysiological study is the compilation of a kind of map of the heart, which will reflect the areas where pathological conduction or formation of electrical impulses occurs. This procedure is performed by introducing a specific contrast and electrical stimulation of areas of the heart. During this procedure, disturbances in the rhythm of the heart are usually induced, but in an operating room these arrhythmias do not pose a threat to the patient.
Upon completion of mapping, cardiac surgeons insert an ablation electrode through the same access and begin performing RFA of the heart. A catheter ablation electrode is installed in the projection of the pathological area and its destruction is carried out by the point action of radio frequency waves. If there is a large lesion or several abnormal zones in the tissues of the heart, their destruction can be performed during one operation or RFA will need to be repeated later.
After the RFA procedure, if indicated, a pacemaker can be installed and programmed.
Since the patient is conscious during cardiac ablation, this is sometimes associated with some discomfort. Therefore, if you experience any unpleasant sensations, it is advisable to inform your doctor. At the same time, you should not be afraid of this intervention, because almost all manipulations with the electrodes are painless for the patient.
The amount of time spent performing radiofrequency ablation ranges from 3 to 7 hours.
Description of the postoperative period and rehabilitation
One of the most significant advantages of RFA compared to open heart surgery is its low morbidity and rapid recovery. While a patient after a sternotomy will feel pain in the sternum, wear a special bandage for months, and limit his exercise, a patient after RFA will be able to return to his normal rhythm of life in a couple of weeks, which will no longer be burdened by arrhythmia.
8
24/7
Directly from the operating room, the patient is transferred to the intensive care unit, where he spends the first day after RFA. Here, constant monitoring of heart rate and blood pressure is carried out. To prevent bleeding from the ablation catheter insertion site, it is recommended to lie down for the first 4-5 hours after surgery.
If there are no complications, the patient will be able to leave the clinic where the cardiac ablation was performed the next day.
Possible complications with RFA
An intervention such as cardiac ablation has a very low risk of serious complications, but does not completely eliminate them. Most often, patients experience a hematoma at the site of electrode insertion, but they usually do not require any specific treatment and go away on their own within a few weeks.
Less common are more serious complications:
- perforation of the walls of blood vessels or tissues of the heart;
- pneumothorax;
- development of complete atrioventricular block.
The risk of death with this operation is usually about 0.2% or less.
RFA results
The effectiveness after RFA surgery will depend on the type of arrhythmia, the anatomical features of the patient’s heart and the presence of concomitant pathology of the internal organs in general and the heart in particular. The percentage of successful RFA ranges from 75% to 95%, for example, in the treatment of supraventricular arrhythmias it is about 96%. The incidence of complications when performing cardiac ablation is no more common than 1.5-2%.
Sometimes, after a successful first RFA operation, new abnormal areas are formed over time, which is associated with the peculiarities of the electrophysiology of the heart of a particular patient; in such clinical situations, repeated ablation may also be required.
In the vast majority of cases, patient reviews of quality of life after RFA are positive. They can engage in activities that were previously denied access due to the risk of arrhythmia. Patients can exercise, women of fertile age can safely carry and even give birth to a child on their own. A significant advantage is that for a number of pathologies after RFA of the heart it is not necessary to continue taking medications continuously.
Cost of the operation
Performing radiofrequency ablation requires high-tech equipment and the presence of qualified specialists, so it is not yet carried out everywhere. Typically, clinics with these resources are located in large cities, and there are even several of them in St. Petersburg and Moscow.
The cost of radiofrequency cardiac ablation is calculated individually for each patient and can vary significantly due to different volumes of intervention, the need for implantation of a stimulator, and the level of the clinic in which the operation is performed. The average price is from 150 thousand rubles.
It should be noted that in the Russian Federation there are quotas for free RFA of the heart.
General multicomponent effect of laser therapy
In general, the effect on the heart and blood vessels when using laser irradiation consists of the following improvements:
- Relieving spasms
- Expansion and strengthening of blood vessels
- Improving blood microcirculation
- Reducing blood viscosity and increasing coagulability (the risk of blood clots is reduced, and microthrombi are resolved)
- Increased hematopoiesis
- Normalizes heart rate and reduces the likelihood of arrhythmias
- Increased cardiac contractile function
- Reduction in blood cholesterol, normalization of many blood parameters
- Increasing the bactericidal properties of bloodReducing ischemic zones
- Improving oxygen metabolism
- Increased oxygen content in tissues
Indications and contraindications for laser therapy
Indications for the procedure are as follows: vegetative-vascular dystonia, neurocirculatory dystonia, hypertension, ischemia, angina pectoris class I-IV, cardiomyopathy, post-infarction condition, myocarditis, myocardial dystrophy, arrhythmia, consequences of cerebrovascular accident, vertebrobasilar insufficiency, discirculatory encephalopathy, atherosclerosis of the lower extremity vessels, obliterating endarteritis , venous insufficiency, varicose veins of the lower extremities, hemorrhoids, Raynaud's syndrome.
Contraindications are common to physiotherapeutic factors: blood diseases with bleeding syndrome, severe thrombocytopenia, deep vein thrombosis, menstruation, severe hypotension, the presence of an implanted pacemaker and pacemaker.
Academician E.M. made a great contribution to the development of low-intensity laser technologies in medicine. Meshalkin, who first introduced the technique of intravenous laser irradiation of blood into the complex treatment of patients with coronary heart disease in 1980. Currently, experts give preference to supravenous laser blood irradiation - NLBI, which gives a pronounced clinical effect in complex therapy for patients with cardiovascular insufficiency.
Contraindications to laser irradiation
The innovative laser method for treating blood vessels and the heart also has its contraindications. These include:
- Pregnancy.
- Chronic diseases of internal organs, if they are exacerbated.
- Certain blood diseases.
- Malignant neoplasms.
- Benign progressive formations.
- Active tuberculosis.
- Thrombophlebitis.
- Some blood diseases.
- Individual intolerance to light therapy.
- Anemia with a hemoglobin value less than 80 is a temporary contraindication.
How a laser therapy session is performed
- The doctor will ask you to sit or lie down.
- The area that will be exposed to radiation must be free of clothing.
- Laser therapy will be performed either remotely (at a distance from the skin from ½ meter to a meter) or contact (the light guide is pressed to the skin, the penetration depth of the azure waves is much greater).
- The department also practices intravascular laser therapy, in which a needle equipped with a disposable light guide is inserted into a vein. Often used for ischemic heart disease.
- There are usually no discomforts during laser procedures.
- The doctor monitors the laser radiation parameters and your condition during the session.
The specialists of the department select all radiation characteristics individually for each specific case. You will be prescribed treatment tactics, determine the localization of the effect, the number of procedures, and the duration of the session.
Laser therapy, a high-tech method of treating lesions of the heart and blood vessels, has been successfully used in our department for a long time. If you have chronic damage to the heart or blood vessels, our experts recommend laser therapy sessions once or twice a year. The therapeutic effect of the technique is extremely high.
What is NLOC and how does it work?
The NLBI technique is simple and accessible. It is also characterized by non-invasiveness, sterility, painlessness, lack of damaging effects on the blood and vessel walls, and no need for disposable infusion systems or light guides.
NLBI activates the circulatory and microcirculation systems, stimulates hematopoiesis, improves the rheological properties of blood and lipid peroxidation, helps reduce cholesterol in the blood, saturates cells and tissues with oxygen, corrects immunity, has an analgesic, anti-inflammatory, and anti-edematous effect. Under the influence of laser radiation, blood viscosity decreases, bleeding and coagulation time lengthens, fibrinogen content, prothrombin index, plasma tolerance to heparin decrease, the level of endogenous heparin increases, and the fibrinolytic activity of the blood increases.
The NLBI technique is an effective means of preventing and treating a wide range of diseases. It can be prescribed as an independent method or as an addition to the main laser therapy treatment program. NLBI is performed on one pair of symmetrical veins. Preference is given to the pair located closest to the source of pathology or problem area.
The impact parameters for NLBI are as follows:
- As an independent method: frequency 5 or 50 Hz, exposure 5-10 minutes for each vein, contact technique (with slight compression), stable. 1st course of treatment: 8 sessions, 1 session per day. If necessary, the second and third courses of NLBI are carried out, the interval between courses is 1-3 months.
- As an addition to the main program: frequency 5 or 50 Hz, exposure 1-5 minutes for each vein, contact technique (with slight compression), stable. The course of treatment is 10 sessions, 1 session per day or for the entire course of the main program.
The number of sessions and courses is determined by the attending physician, based on the effectiveness of the results.