The mammary glands, like the rest of the body, consist of many veins, blood vessels and capillaries. Protruding veins are usually associated with some kind of medical condition. But this doesn't always happen. For example, people with fair and thin skin are known to have prominent veins throughout their lives. They do not cause discomfort and do not cause any diseases.
Venous networks are visible not only on the chest, but also on the arms and legs. Prominent capillaries on the chest are considered the safest because they are in the part of the body where the veins are close to the skin and therefore can see through it. Also, dishes can stick out after playing sports or excessive stress.
If they swell and protrude too much under the skin, consult a doctor.
This problem can occur not only in women, but also in adolescents and men. They have breast veins that dilate when levels of the hormone estrogen increase.
Protruding vessels: what is considered normal
Protruding veins on the chest are considered normal if a person experiences strong emotions for a long time, cries or laughs. This is the first reason for the appearance of veins.
The second reason could be any physical activity. As you tense, your muscles increase in size and bring your veins closer to your skin.
The third reason for venous imaging is external factors. One of them is constant exposure to the sun. Sun exposure is contraindicated for people suffering from vascular diseases. Increased body temperature in the sun causes increased blood pressure, which leads to prominent veins.
The fourth reason for blue veins can be any changes in the female body. This could be a delay in menstruation, PMS or inflammatory processes. The most common change is pregnancy.
Subjective first signs of pregnancy
Often the first changes in the body that a woman differentiates as signs of pregnancy may turn out to be symptoms of PMS. However, if you have never suffered from premenstrual syndrome before, you should pay attention to these:
- Feeling of weakness, malaise and increased fatigue even with usual exercise.
- The appearance of drowsiness during the day and insomnia at night.
- Unstable emotional state. A woman’s mood can change dramatically in a matter of seconds without good reason.
- A feeling of heaviness in the lower abdomen, lower back and pelvic area.
- Constant headache and dizziness.
- Change in libido. Moreover, it can either decrease or increase.
- Periodic sensations of heat or chills that replace each other.
- Increased sensitivity of the mammary glands to the point that any touch to the breast results in extremely unpleasant sensations and even pain.
- Increased appetite or change in eating habits. From the first days of pregnancy, a girl may want to eat more or eat dishes that she did not like before.
- The appearance of an unreasonable feeling of nausea. In some cases, heartburn and vomiting occur. This condition is called toxicosis.
- Increased sensitivity to odors and distortion of the sense of smell.
All of the above signs cannot accurately answer the question: has pregnancy occurred or not? However, they allow us to suspect it and move on to more accurate and reliable diagnostic methods.
Venous network during pregnancy
The body is completely rebuilt in the early stages of pregnancy. The mammary glands change shape and size, their growth is observed, and preparation for feeding the baby begins. The skin stretches and thins. The size of the breast and nipple increases.
Hormonal changes in the body occur, resulting in the formation of venous networks. They are also called spider veins.
Aesthetically, it looks ugly, but after the baby is born, the hormonal levels will normalize and all symptoms will go away. The cause of spider veins may be the activation of the hormones progesterone and estrogen, which help increase breast tissue for feeding the baby. This causes the blood vessels to dilate and create a venous network.
The appearance of veins on the nipples is also not uncommon. For medicinal purposes, a pregnant woman may be prescribed medicinal ointments or gels, and therapeutic exercises. The main thing is that the treatment does not put the fetus at risk.
Sometimes this pattern also appears in men who like to be in places with high temperatures - baths, saunas, in the sun.
If the problem does not disappear after childbirth, then it is necessary to use vasoconstrictor drugs to strengthen the walls of blood vessels. Sometimes doctors perform laser operations to remove small vessels, use ultrasound treatment, and sclerotherapy. The latter procedure involves the introduction of a special sclerotic agent into the vessels, which glues the walls of the vessels.
This is a safe and popular procedure. After it, bruises and swelling may appear, but they go away over time. Unlike sclerotherapy, laser therapy does not leave bruises and is effective after the first session. If the procedure is not carried out properly, minor skin burns may occur, which will resolve quickly.
Spider veins during pregnancy
Pregnancy is a special physiological state of a woman, in which the course of most processes changes. First of all, this concerns hormonal levels, as well as metabolism (metabolism). Spider veins during pregnancy are a consequence of the influence of certain hormones, the level of which increases, on the functional state of the walls of the microcirculatory structures. After childbirth and normalization of hormone levels, telangiectasias do not disappear on their own, but require treatment.
What diseases can blood vessels in the mammary glands tell you about?
If venous threads on the chest do not appear due to pregnancy or other physiological reasons, then most likely this is a harbinger of some kind of disease. Only a specialist doctor can say this. It could be a blood problem, breast inflammation, an infection in the body, or lumps forming.
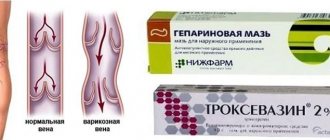
The most common diseases of the blood system include varicose veins and thrombophlebitis.
Most often, the lower limbs are affected; if the disease has spread to the mammary glands, it means it is already in an advanced stage.
Blue spider veins are symptoms of varicose veins in the breast. They bring not only aesthetic, but also physical problems; the disease can be accompanied by pain. Treatment of varicose veins leads to untimely swelling of the capillaries and their green color. Complex treatment is required.
The inflammatory process in the mammary glands occurs during mastitis and mastopathy. During these diseases, lumps in the chest, increased temperature, and deterioration in general condition occur. Infectious diseases may cause inflammation of the lymph nodes, followed by swelling of the veins. Another pathological cause of protrusion of the venous network onto the mammary glands can be neoplasms: adenoma, cyst or lipoma. They are also accompanied by lumps in the chest, high fever and weakness.
Spider vein removal
The basis of radical therapy for telangiectasias is their removal using various methods of physical or chemical influence, as well as taking measures to prevent re-exposure to the provoking factors of their development. High-quality removal is carried out in our medical center using the following methods:
- Sclerotherapy is the introduction into the lumen of the affected vessel of a special chemical compound (sclerosant), which leads to its gluing.
- Laser therapy is exposure to laser, which leads to “evaporation” of the tissues of the inner surface of blood vessels, followed by gluing.
- Electrocoagulation is the destruction of telangiectasia using local point exposure to electric current of a certain strength and frequency.
- Radio wave surgery – excision of the formation is performed, in which radio wave radiation plays the role of a scalpel.
The choice of method for removing telangiectasia on the chest is carried out individually by a phlebologist-mammologist.
Non-dangerous causes of bulging veins on the chest
Dangerous causes of protruding veins include the following:
- The period of adolescence, hormonal changes (in adolescence, girls develop mammary glands, the skin stretches and thins).
- Long-term exercise (saturation of blood with oxygen causes vasodilation).
- Breast changes after miscarriage (pregnancy also affects changes in the breasts, which can thin the skin on the breasts and veins and red blood vessels begin to appear).
- Sharp weight loss (the fat layer under the skin disappears, the skin becomes thinner, and veins appear under the skin).
- Visiting patients with infectious diseases.
- Mood swings (strong emotions cause an active rush of blood to the vessels);
- Taking hormones (many of them have side effects in the form of blood clotting, which worsens the condition of the veins).
- Menopause (hormonal imbalance causes protruding veins).
- Abrupt cessation of breastfeeding.
Diagnosis of varicose veins
At the appointment, the phlebologist performs a visual examination of the patient. An experienced specialist will recognize varicose veins at the earliest stages.
During diagnostic procedures, the doctor establishes or excludes the presence of varicose veins, then he determines the nosological variant of chronic venous disease and determines treatment strategies. It is at the stage of determining the treatment strategy that the doctor decides which methods are suitable for correcting varicose veins of the extremities - whether it is possible to limit ourselves to conservative non-surgical methods, or whether only surgical methods of treating varicose veins are possible.
Next, the treatment tactics are determined - is it possible to treat with one technique or is a combination of several techniques better suited for the treatment of varicose veins. At the final stage, the doctor objectively evaluates the effectiveness of treatment procedures.
Methods for diagnosing varicose veins of the lower extremities
:
In addition to the traditional history taking, examination and palpation in modern medicine, the diagnosis of diseases of the veins of the lower extremities is carried out using ultrasound angioscanning - USAS.
Ultrasound angioscanning is a modern express method that allows you to diagnose the condition of veins and arteries and can determine signs of venous reflux (backflow of blood from the deep superficial vein).
Ultrasound ultrasound is the most basic method for diagnosing varicose veins of the lower extremities.
Next, the doctor determines the treatment strategy for the disease. Modern methods of treating varicose veins of the lower extremities allow the procedure to be carried out painlessly and absolutely safely.
Remember that you absolutely cannot prolong the course of the disease, since varicose veins can cause all sorts of complications.
Alarming causes of swollen capillaries on the chest
If the bulging vessels on the mammary glands do not subside over time, have a bright color and become very bulging, you should consult a doctor. A mammologist deals with this problem. If a patient develops lumps or nodules, he is referred to a phlebologist, a specialist who studies vein diseases. He will refer the patient for additional tests, ultrasound, ductography and sonography.
Thrombosis has alarming symptoms with varicose veins. The skin turns blue, a feeling of heaviness appears in the chest, the mammary glands swell and enlarge. This requires urgent intervention from a medical specialist.
Treatment of vein disease in women
There are two types of treatment for varicose veins in women: conservative and invasive. In the first case, we are talking about measures that are aimed at preventing and stopping the development of the disease: following a diet, wearing compression garments, taking phlebotonics as prescribed by a doctor. Invasive treatment involves surgical interventions such as sclerotherapy, laser coagulation, miniphlebectomy, etc. The treatment method is selected individually by a phlebologist.
Treatment with folk remedies
If protruding venous threads are a sign of varicose veins, you can add the use of folk remedies for treatment.
These include: apple cider vinegar, hazel leaf tincture, nutmeg tincture, hop cones. Some of the available remedies help with varicose veins: sea salt, potatoes, lemon.
There is also a set of exercises that help thin thick blood and improve blood circulation in the vessels to avoid stagnation.
Treatment methods for varicose veins of the lower extremities
There are various methods for treating varicose veins - surgical intervention, conservative methods (compression therapy, medication, physiotherapy) and modern non-surgical methods such as laser treatment, radiofrequency ablation of veins, sclerotherapy, phlebectomy.
1. Operation
Traditional surgery today is rarely prescribed and for certain indications. First of all, this is explained by the fact that the removal of a vein itself is accompanied by significant trauma, the possible appearance of hematomas, a long postoperative period and prolonged pain.
2. Conservative treatment
Depending on the stage and severity of the venous disease, one or another type of treatment is selected. Conservative treatment methods are required at any stage of the disease - as additional therapy or as primary therapy, depending on the degree of damage to the blood vessels. Conservative treatment methods include physical therapy, compression treatment of varicose veins and drug treatment of varicose veins of the lower extremities.
2.1. Physiotherapy
This method involves performing pressotherapy. This procedure is aimed at removing excess fluid from the lower extremities, formed against the background of chronic venous insufficiency and initial venous edema.
Like any other conservative method, physiotherapy does not imply the elimination of affected vessels and their areas; it reduces the manifestation of varicose veins. With the help of physiotherapy, venous and lymphatic outflows are improved, microcirculation is improved, and discomfort in the lower extremities, such as pain and cramps in the calf muscles, disappears.
2.2. Compression treatment of varicose veins
Compression therapy is used to apply pressure to the superficial and deep veins. The fastest outflow of blood occurs at the very bottom, in the legs - the veins are narrowed there, and the outflow of blood is the fastest. External pressure helps the blood flow and, as a result, the valves work more efficiently.
Compression treatment is used without fail as an additional therapy for all modern methods of treatment, less often - as the main method of treatment (in cases of the very initial stage of the disease and for its prevention).
Compression garments help relieve symptoms of varicose veins such as swelling, fatigue of the lower extremities, and a feeling of heaviness.
2.3 Drug treatment of varicose veins of the lower extremities.
Drug therapy involves taking medications that can improve the structure and function of the venous walls. However, the veins will remain tortuous and dilated; it is impossible to completely cure varicose veins with the help of medications, creams and ointments. Increased tone of the venous walls with the help of medications is not able to correct the improper functioning of the valves. Medicines (venotonics), ointments, creams reduce swelling and pain symptoms, and are also prescribed for the prevention of thrombosis and healing of trophic disorders.
With the help of conservative treatment, it is impossible to prevent the further development of venous disease and cure the patient.
3. Modern technologies and methods of treating varicose veins of the lower extremities
Today, medicine has made great strides forward; traditional operations remain far in the past; they have been replaced by modern methods of treating varicose veins without surgery. These include gentle methods such as radiofrequency ablation of veins, sclerotherapy, phlebectomy and laser treatment of varicose veins.
3.1 Radiofrequency ablation of veins (RFA of veins)
This is modern technology and one of the most effective ways to treat varicose veins of the lower extremities. RFA has great advantages over any other method of treating varicose veins. The procedure is a modern alternative to traditional surgery and is performed under local anesthesia. The essence of the method is to introduce a special conductor into the affected vein that produces thermal radiation. With the help of radiofrequency radiation, a thermal effect occurs on the walls of the affected area of the vein; the structure of the damaged vessel is destroyed, the vein is excluded from the general blood flow system. The operation lasts from 30 to 60 minutes and does not require hospitalization.
The procedure is absolutely safe for the patient and most effective. Important advantages of this method are the elimination of incisions (the operation involves a small puncture) and the fastest possible recovery after the procedure - after 15-20 minutes the patient can go home.
3.2
Sclerotherapy
This method involves the treatment of varicose veins of the lower extremities by gluing the walls of blood vessels, in other words, closing the vein. A drug in foam or liquid form is injected into the lumen of the vein, which glues the vein together. This method does not require any damage to the skin and is virtually painless. The procedure lasts about 30 minutes, and afterward compression therapy is required - compression garments or bandages help the process of gluing the veins.
With the help of sclerotherapy, both capillary networks and large veins are removed; This method eliminates postoperative scars and defects.
3.3 Phlebectomy
The method involves removing the altered vein. Phlebectomy is used in cases where the disease has gone beyond the initial stages, is severe, and other methods become ineffective.
The procedure is carried out through small incisions of a few millimeters and lasts about two hours; This implies hospitalization of the patient for 1-2 days. Further compression therapy is also required.
3.4 Laser treatment of varicose veins of the lower extremities (ELVE)
The endovasal laser coagulation (EVLC) method is one of the most common methods of treating varicose veins and involves the thermal effect of a laser beam on the vein walls. A light guide inserted into a vein acts on it with a laser beam, resulting in gluing of the venous vessel.
The procedure does not require general anesthesia and lasts about 40-60 minutes. Further compression therapy is mandatory.
The method of treating varicose veins is determined by the doctor, who first conducts all the necessary studies and, based on them, selects the most preferable method of treating the disease.
Prevention of venous disease
You can prevent such troubles with protruding veins by following certain preventive measures:
- A proper, nutritious diet with vegetables and fruits containing vitamins.
- Regular fluid intake.
- Avoid bad habits.
- Maintain personal hygiene.
- Temporary restriction of sports activities.
- If you have high blood pressure, avoid saunas.
- Normalization of the emotional background.
- Protecting the mammary glands from hypothermia.
If you have a sedentary lifestyle, exercise more often to avoid blood embolism in the vessels. All these preventive measures will help prevent the appearance of veins on the chest in the future.
Treatment results for our patients
Disease: varicose veins
Treatment method: EVLT + MINIFLEBECTOMY
Combined treatment of varicose veins. Endovasal laser obliteration of the vein on the left leg (EVL) + Miniphlebectomy
Disease: varicose veins
Treatment method: EVLT + MINIFLEBECTOMY
Laser treatment (EVLT) followed by miniphlebectomy of the tributaries of the great saphenous vein on the thigh and shin of the right leg. Miniphlebectomy of varicose veins.
Disease: Telangiectasia
Treatment method: Foam sclerotherapy
To remove the stars, the patient underwent a session of microfoam sclerotherapy (Foam-Form) of the reticular veins under the control of laser transillumination.
Disease: varicose veins
Treatment method: EVLT + MINIFLEBECTOMY
Upon examination of the patient, varicose veins were diagnosed on the right leg. Combined treatment with EVLT + miniphlebectomy was performed.
I'll wait a little longer Make an appointment
Therapeutic measures
The key to a quick recovery without the development of serious consequences is correctly prescribed treatment by the attending physician. If the veins on the mammary glands are visible for natural reasons, then therapeutic intervention is not required. Disorders in the body and other concomitant diseases are the main reasons for visiting a specialist.
Hormonal disorders are eliminated by restoring hormone levels with special medications. You can also improve the endocrine state of the body by changing your lifestyle.
Concomitant diseases require modern diagnosis and treatment. The lack of competent therapy is fraught with more serious complications than a cosmetic breast defect. In this case, the attending physician prescribes drug or surgical therapy. To improve your well-being, you need to follow a diet and engage in physical therapy.