Introduction
This information has been specially prepared for you, so that you, your family and friends can find answers to your questions on these pages.
More than two million people, thanks to a pacemaker, live a full life - study, work, travel, and play sports. Most patients with pacemakers remember it only when they come for a medical examination, and in everyday life their activity in the family, on vacation and at work is no different from the people around them. First of all, the main purpose of pacemaker implantation is to eliminate life-threatening arrhythmias and improve your quality of life. All subsequent restrictions and your regimen will depend on your physical condition, manifestations of the disease and the recommendations you receive from your doctor.
After operation
The patient is under the supervision of medical personnel for a week. During this time, the sutures heal and can be removed. The patient is preparing for discharge. Before sending the patient home, he is examined by a doctor. Makes appointments and issues instructions on how to behave during the rehabilitation period and move on with your life.
After discharge, the patient registers at his place of residence and promptly visits the doctor. In the first 3 months, it is important to follow the recommendations:
- temporarily stop physical activity;
- you cannot lift weights;
- You can’t drive;
- MRI cannot be done;
- avoid radar technology;
- refuse thermal procedures;
- Report any ailments to your doctor.
You should visit a cardiologist regularly for the next six months. It is allowed to use household appliances. You need to turn them on with the opposite hand to the installed pacemaker, including when talking on the phone, and place the phone on the opposite side of the installed pacemaker. Metal detectors should be avoided in stores, airports, and concert halls.
Lifetime rules after pacemaker implantation:
- monthly visit to a cardiologist;
- daily measurement of blood pressure and pulse. It is advisable to keep a diary and mark the data;
- complete cessation of bad habits;
- carry your pacemaker passport with you.
Pacing and why it is necessary for your heart
The most common condition that requires a pacemaker is called bradycardia, which means the heart rate is too low for the body's needs. Possible symptoms of bradycardia are dizziness, extreme fatigue, shortness of breath, and fainting. Bradycardia is usually caused by one of the following heart diseases (or complications of the underlying disease) or a combination of them:
- Sick sinus syndrome (SSNS) – the sinus node sends impulses infrequently, at too long or irregular intervals.
- Heart block is a disruption of the normal passage of electrical impulses from the heart. Heart block can occur at various levels of the conduction system, but usually this term refers to conduction block at the level of the atrioventricular (atrioventricular) node. In this case, the impulses produced by the sinus node do not reach the ventricles. The ventricles contract very rarely, in their own rhythm, asynchronously with the atria.
Your heart rate usually beats between 60 and 80 beats per minute. A reading below 60 beats per minute is called bradycardia. For many people in good physical shape (or such a rhythm occurs during rest and sleep), such a rhythm is the norm. A distinctive feature of such bradycardia is that with increasing physical activity, the heart rate begins to accelerate, covering the body’s needs with its frequency.
We talk about bradycardia as a disease when the rhythm has a very low frequency, does not respond by increasing frequency to physical activity, or large pauses occur in the rhythmic contraction, which can reach or even exceed more than 2 seconds.
When bradycardia is confirmed diagnostically and such a rhythm is the only manifestation, then such a rhythm is effectively corrected by a pacemaker.
Electrocardiac pacemaker (Pacemaker)
Modern pacemakers are miniature computers that monitor your heart's own rhythm. Stimulants can come in a variety of shapes and are generally small and light (approximate weight 20 to 50 grams).
The pacemaker consists of a titanium housing that contains a microcircuit and a battery.
The main function of a pacemaker is to monitor the heart rhythm and stimulate if a rare or irregular rhythm occurs with skips in contractions. If the heart beats with the correct frequency and rhythm, the pacemaker in this case does not work, but constantly monitors its own heart rhythm.
Each type of pacemaker is designed for a specific type of heart rhythm disorder. The indications for implantation are determined by your doctor based on the data obtained from your examination.
Pacemakers can be either single-chamber or multi-chamber (two or three stimulating chambers). Each stimulation chamber is designed to stimulate one part of the heart. Dual-chamber devices stimulate the atrium and right ventricle, while three-chamber cardiac resynchronization devices (CRT) stimulate the right atrium, right and left ventricles.
Cardiac resynchronization stimulators are used to treat severe forms of heart failure, eliminating uncoordinated contractions of the heart chambers (dyssynchrony).
Pacemakers may be equipped with sensors. Such stimulators are called frequency-adaptive; they use a special sensor that detects changes in the body (such as movement, nervous system activity, respiratory rate, body temperature). Frequency-adaptive stimulators (indicated by a special letter R - indicates frequency adaptation) are used for rigid, i.e. Since the heart rate does not change depending on physical activity and emotional state, then in this case the increase in rhythm due to physical activity will occur due to the pacemaker.
The pacemaker consists of:
- Battery (accumulator) The battery supplies electrical energy to the pacemaker and is designed for many years of uninterrupted operation (up to 10 years). When the pacemaker battery capacity is depleted, the pacemaker is replaced with another one.
- Microcircuit The microcircuit is like a small computer inside a pacemaker. The microcircuit transforms battery energy into electrical impulses to stimulate the heart. The microcircuit controls the duration and power of electrical energy expended for the pulse.
- Connector block A transparent plastic block is located at the top of the pacemaker. The connector block is used to connect the electrodes and the pacemaker.
Electrodes
The pacemaker is connected to the heart through veins using special electrodes. The electrodes are attached to the cavities of the heart and play a connecting role between the activity of the heart and the stimulator.
The electrode is a special coiled conductor that is flexible enough to withstand the torsion and bending caused by body movements and heart contractions. The electrode transmits the electrical impulse generated by the pacemaker to the heart and carries back information about the activity of the heart.
The electrode contacts the heart through a metal head at the end of the wire. With its help, the stimulator “monitors” the electrical activity of the heart and sends electrical impulses (stimulates) only when the heart requires them.
Programmer
The programmer is a special computer that is used to control and change the settings of the pacemaker. The programmer is located in medical institutions where pacemakers are implanted or where there is a consulting room for working with patients with pacemakers.
The doctor analyzes all the functions of the pacemaker and, if necessary, can change the settings necessary for the pacemaker to function correctly. In addition to technical information about the pacemaker operation, the doctor can view all recorded cardiac events in chronological order. Such events include atrial and ventricular cardiac rhythm disturbances (atrial flutter and fibrillation, supraventricular and ventricular tachycardia, ventricular fibrillation).
Single-chamber pacemaker
A single-chamber stimulator uses a single endocardial lead placed in either the right atrium or right ventricle to stimulate the cardiac chamber (atrium or ventricle).
Isolated atrial stimulation is used in cases where the generation of sinus rhythm (SSRS) is impaired while the atrioventricular junction (atrioventricular node) is functioning intact. In this case, cardiac pacing completely or partially replaces the function of sinus rhythm.
Ventricular stimulation is used if the patient has a permanent form of atrial fibrillation or transient atrioventricular blockade of the sinus rhythm into the ventricles occurs. In rare cases, it can be implanted with complete atrioventricular block.
Dual chamber pacemaker
A dual-chamber pacemaker uses two endocardial leads to pace the right atrium and right ventricle. The electrodes are placed in the appropriate areas, thereby stimulating two chambers of the heart at once.
Dual-chamber stimulators are used to synchronize the atria and ventricles in cases of impaired atrioventricular conduction (AV junction dysfunction), which makes the heart rhythm closest to natural.
Both single-chamber and dual-chamber pacemakers can be equipped with a frequency adaptation function. The frequency adaptation function is used to increase the heart rate if one’s own, natural rhythm cannot respond by increasing the frequency to physical activity or to the emotional state of a person.
Frequency adaptation is marked with the Latin letter R. In single-chamber stimulators the designation SR is used, in dual-chamber stimulators - DR.
What types of ICDs are there?
Single chamber ICD
A single-chamber ICD is used in cases of atrial fibrillation or when the patient does not have transient conduction blocks and the heart rate fully corresponds to the needs of the body.
The stimulator has one ventricular electrode, which is placed in the cavity of the right ventricle. When VT or VF occurs, the pacemaker delivers a defibrillator shock.
The stimulator has an algorithm for ultra-frequent and programmed stimulation to prevent an attack of VT with “painless stimulation”. In addition to the high efficiency of the painless stimulation algorithm in stopping VT, this mode practically does not consume the pacemaker battery charge. In this case, the defibrillator does not discharge.
If the patient has bradycardia, the ICD works like a regular pacemaker.
Dual chamber ICD
A dual-chamber ICD contains two pacing chambers designed to stimulate the right atrium and the right ventricle. Electrodes are placed in the appropriate areas, thereby tracking the heart rhythm in the atria and ventricles.
During AV blockade, the ICD paces the atrial and ventricular rhythms. Antitachycardia therapy is carried out at all levels, including the ability to stop a sudden increase in atrial rhythm during atrial flutter, atrial tachycardia, and supraventricular tachycardia with antitachycardia pacing (ATS). ATC is widely used to provide pain-free therapy for VT, thereby preserving ICD battery charge.
Three-chamber ICD (CRT/ICD)
Cardioverter-defibrillator with cardiac resynchronization therapy. CRT/ICD is used to treat heart failure (HF) by synchronizing the ventricles of the heart into a single heartbeat cycle.
CRT/ICD can provide the full range of antiarrhythmic therapy, including defibrillator shock therapy to restore heart rhythm.
Pacemaker implantation procedure
Pacemaker implantation is a surgical procedure in which a small incision is made in the right (if you are left-handed) or left (if you are right-handed) subclavian region. Depending on which pacemaker you are implanted with, one, two or three electrodes will be inserted through a vein and placed inside the heart under X-ray guidance.
As with most surgical procedures, a short course of prophylactic therapy with antibiotics and anti-inflammatory drugs will be prescribed after pacemaker implantation.
Before surgery, your doctor will limit or stop certain medications you take, and the choice of anesthesia will be determined by your anesthesiologist before surgery. The operation of implanting (sewing in) a stimulator seems simple, since it causes little damage to tissue, and is carried out in an operating room equipped with an X-ray machine. A vein is punctured (pierced) under the collarbone, a special plastic tube (introducer) is inserted into it, through which endocardial electrodes are inserted into the superior vena cava (transvenously). Under X-ray control, the electrodes are directed into the right atrium and right ventricle, where they are fixed.
The most difficult procedure is to install and secure the tip of the electrode in the atrium and ventricle so as to obtain good contact. Usually the surgeon makes several tests, all the time measuring the threshold of excitability, i.e. the smallest impulse value (in volts) to which the heart responds with a contraction, visible on the ECG. The challenge is to find the most sensitive spot and at the same time get a good ECG graphic recorded from the electrodes being installed. After fixing the electrodes, they are connected to a stimulator, which is placed in a formed bed under the fascia of the fatty tissue or under the muscles of the chest.
Of course, the operation requires strict sterility and careful control of bleeding to avoid accumulation of blood under the skin and suppuration. The stimulator itself and electrodes are supplied sterile. In total, all manipulations take from one to two hours.
The described method is most often used for pacemaker implantation in surgical practice. There are other implantation methods that are used in connection with certain characteristics or concomitant diseases of the cardiovascular system.
If a patient is scheduled to undergo open heart surgery due to an underlying medical condition and there is an indication for pacemaker implantation, then, as a rule, the leads will be placed epicardially (the outer lining of the heart) and the pacemaker will be placed in the rectus abdominis muscle. This placement of electrodes is optimal because the electrodes do not come into contact with human blood and are not located in the heart cavity.
Preparing for surgery
Before the operation, the patient must undergo a full examination and pass a list of tests. Our cardiology center of the Federal Scientific and Clinical Center FMBA offers its patients planned hospitalization. During your stay in the cardiovascular surgery department, you will undergo all the necessary tests. The list of examinations includes:
- clinical and biochemical blood test (total protein, creatinine, urea, total bilirubin, direct bilirubin, glucose, pancreatic amylase);
- determination of blood group and Rh factor;
- detailed coagulogram;
- platelet aggregation indicator ADP;
- markers of infections: HIV, hepatitis B, hepatitis C, syphilis;
- general urine analysis;
- chest x-ray;
- ECG;
- EchoCG;
- EGDS;
- Ultrasound scanning of brachiocephalic arteries;
- Ultrasound scanning of the arteries of the lower extremities and veins of the lower extremities;
- FVD;
- Ultrasound of internal organs;
- TEE;
- coronary angiography.
If during the examination the doctor discovers a concomitant pathology, you may be prescribed additional tests and consultation with related specialists (neurologist, ophthalmologist, endocrinologist, etc.).
Our center is equipped with high-precision modern equipment. Thanks to their extensive experience and many years of work experience, doctors guarantee the most accurate diagnosis and interpretation of indicators. Our own clinical diagnostic center is responsible for the accuracy of test results. By undergoing an examination with us before implantation of an pacemaker, you can be confident in the quality of the services provided and the speed of their provision. Collecting all the necessary research can take months, while we will prepare you for surgery in just 1 day.
Before the operation, the patient needs to prepare; to do this, just follow simple recommendations:
- A few days before surgery, the doctor may stop taking medications. Alcohol must be eliminated (preferably a week in advance);
- on the day before pacemaker implantation, the patient has breakfast and lunch as usual. In the evening, a light dinner is brought, the last meal should be no later than 6-8 hours before the operation. You can drink water in unlimited quantities;
- at night the patient is given a cleansing enema;
- In the morning, the patient takes a shower and prepares the surgical field. It is necessary to shave the hair in the chest area.
Before the patient is taken to the operating room, he is examined by a surgeon and an anesthesiologist. A mild sedative may be administered to calm and relieve anxiety.
What is CRT/ICD?
There are a large number of pacemakers (pacers) that are designed to treat cardiac arrhythmias and conduction disorders. Depending on the complexity of the arrhythmias, your doctor will suggest one type of pacemaker or another. Its size will depend on the specifics of the stimulator and its functions and battery capacity of the pacemaker. The first stimulators developed were placed on a cart and pacing was carried out through wires to the heart. Over the past three decades of technological progress, complex pacemakers with a large battery capacity and dimensions no larger than a matchbox have been introduced into clinical practice.
In the late 90s, implantable cardioverter-defibrillators (ICD) and cardiac resynchronization devices (CRT) were developed and put into practice. The first pacemakers were presented separately and had a large weight and size. Cases have been described where it was necessary to implant two CRT and ICD stimulators at once in one person.
Implantable cardioverter-defibrillator with cardiac resynchronization therapy ICD/CRT is a combined device intended for the treatment of heart failure and suppression (relief) of ventricular tachycardia or ventricular fibrillation (life-threatening arrhythmias).
ICD (ICD) implantable cardioverter-defibrillator.
Used to detect and relieve most cardiac arrhythmias. Its main function is to restore the heart rhythm by shock discharge (defibrillation) when ventricular tachycardia (VT) or ventricular fibrillation occurs. In addition to the possibility of a shock discharge, the function of painless suppression of VT through ultra-frequent and programmed stimulation is provided.
After implantation, the pacemaker operates automatically.
The stimulator is no larger than the size of a pager or the palm of a small child.
How does an ICD work?
Therapy of tachyarrhythmias
An ICD pacemaker constantly “monitors” the electrical activity of your heart. It can always tell what your rhythm is, including performing the function of a “Holter monitor” by recording fragments of the heart rhythm into memory, helping the doctor learn more about the patient’s rhythm than a regular electrocardiogram. If a tachyarrhythmia occurs in the heart, the stimulator algorithms will provide electrical therapy automatically. The type of treatment and program of stimulator functions depends on the settings that your doctor chooses.
After implanting the ICD, your doctor will tell you what therapy he has prescribed.
Ventricular fibrillation is a very life-threatening event. The ICD is specifically designed to restore sinus rhythm with a shock shock. This is called defibrillation. Your ICD has pain-free rhythm restoration (anti-tachycardia function) and anti-bradycardia function to treat all types of bradyarrhythmias.
Defibrillation
If the ICD detects VF, it delivers a high-energy shock. This is called defibrillation. During defibrillation, a shock is delivered directly to the heart. Restoring sinus rhythm requires much less energy (1/10th) compared to external defibrillation, which is performed by doctors in emergency situations.
The total time from the onset of a VF attack to the defibrillator shock is about 10 seconds. During this time, energy accumulates in the ICD, which is necessary to produce a high discharge during defibrillation.
Cardioversion is the restoration of heart rhythm by a defibrillator discharge (shock energy discharge). There are two types of electrical cardioversion: external, by applying special plates to the chest, and internal, through an electrode in the right ventricle with an electric current discharge.
Antitachycardia pacing (ATP)
Antitachycardia pacing has been widely used to suppress most cardiac tachyarrhythmias, including VT. The meaning of ATS is to determine heart rhythm disturbances and suppress an attack through ultra-frequent or programmed stimulation.
ATS is widely used to provide pain-free therapy for VT, thereby preserving battery charge. If the ATS is ineffective or in VF, it produces a defibrillator discharge.
If ventricular tachycardia occurs, your ICD will check for the abnormal rhythm and provide the necessary therapy to restore sinus rhythm. The type of antitachycardia function program is determined by your doctor when programming the ICD. If an antitachycardia function is established (painless relief of tachyarrhythmias), then during an attack of VT the stimulator will restore the correct heart rhythm with frequent electrical stimulation with a certain sequence. This stimulation is called antitachycardia therapy; when it occurs, the patient does not feel it.
Antibradycardia pacing
If your heart rhythm becomes very slow or skips (pauses) occur, the ICD can work like a simple pacemaker used for bradycardia. The atrial and ventricular pacing chambers synchronize the upstream and downstream rhythms, thereby creating the optimal pacing pattern.
Alarm system
The ICD may have a built-in function to alert the patient to the need to see a doctor for evaluation. The ICD can be programmed to sound 30-second beeps when conditions require urgent medical attention. The two different beep tones correspond to different reasons. The signals are repeated every 24 hours until the doctor reads the information using the programmer. If the ICD beeps, consult a doctor immediately!
Why does my doctor recommend CRT/ICD implantation?
The doctor’s recommendations are based on the results of studies confirming the diagnosis and the presence of a threat to your life.
In many patients, severe systolic heart failure is accompanied by significant intra- or interventricular conduction delays, which lead to disruption of the synchrony of contraction, which is accompanied by a decrease in the efficiency of the pumping function of the ventricles.
1. Due to progressive symptoms of heart failure, which are accompanied by shortness of breath, swelling of the legs, weakness:
- Patients in whom the ventricles of the heart do not contract together (ventricular dyssynchrony).
- Patients with symptoms refractory to drug therapy - without improvement in quality of life (NYHA functional class III or IV).
- Patients with ineffective heart function – low ejection fraction (35% and below), increased volume and size of the heart.
Pacemakers with CRT/ICD function are able to restore synchronous contraction of the heart and, as a result, eliminate symptoms associated with heart failure. Studies have shown that most patients after CRT/ICD implantation experience improved well-being and quality of life, and increased exercise tolerance.
2. Your heart may be susceptible to very life-threatening palpitations. Heart rhythm disturbances can occur in almost every person, but are more often caused by coronary heart disease, myocardial infarction, heart defects, cardiomyopathies and inflammatory diseases.
Ventricular tachycardia is a life-threatening rhythm disorder. With excessively frequent contractions, the ventricles of the heart do not have time to fill with enough blood. As a result, insufficient blood flows to organs, including the brain. In addition to palpitations, you may feel weak, dizzy, and possibly lose consciousness.
Ventricular tachycardia is accompanied by a decrease in blood pressure and in some cases can cause ventricular fibrillation. Cardiac arrest is a very serious event that requires emergency medical care and defibrillation to restore heart rhythm. Unfortunately, this procedure is not always possible in the first minutes of cardiac arrest. Therefore, the implantable CRT/ICD has a built-in defibrillator that provides the emergency therapy (shock) needed to restore normal rhythm.
Are there alternative treatments?
Alternative treatment for heart failure.
The possibility of alternative treatment depends on the form and stage of heart failure.
Mild forms of heart failure respond well to medication, lifestyle changes and diet. The mainstays in the treatment of heart failure are a strict diet and the use of drug therapy aimed at eliminating the causes of heart failure.
If the cause of heart failure is coronary artery disease or valvular heart disease, your doctor will refer you to a heart surgeon. Surgical correction of valve pathology and angioplasty of the affected arteries of the heart can completely eliminate all symptoms and manifestations of heart failure.
In the most complex cases of heart failure with ineffective drug therapy to save the patient's life, the issue of cardiac transplantation or the use of left ventricular bypass systems (artificial heart ventricle) will be considered.
Cardiac resynchronization devices (CRT) are considered as an alternative to heart transplantation (HT).
The advent of cardiac resynchronization devices in medical practice has made it possible to effectively combat the manifestations of HF in cases where the cause of HF is myocardial dyssynchrony, low ejection fraction and left bundle branch block (LBBB). Numerous implantations of devices have given reason to consider the effect of such therapy not only as a “bridge to transplantation,” but also as a “bridge to recovery.” CRT implantation is indicated for patients with severe forms of heart failure, NYHA functional class III-IV.
Alternative treatments for life-threatening cardiac arrhythmias.
Heart rhythm disturbances can occur in different parts of the heart and manifest themselves in the form of extrasystole or very fast rhythm (tachycardia). As a rule, heart rhythm disturbances are divided into functional (reversible) and organic (non-reversible). Functional disorders include those types of heart rhythm disturbances that are caused by endocrine and metabolic disorders, poisoning, alcohol use, and severe stress. Timely correction and elimination of the causes of arrhythmia leads to recovery.
The most dangerous arrhythmias are considered to be rhythm disturbances caused by damage or changes in the myocardium, which are observed with myocardial infarction, myocarditis, cardiosclerosis, arrhythmogenic dysplasia of the right ventricle, etc.
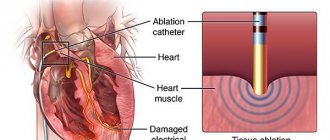
Most cardiac arrhythmias respond to antiarrhythmic therapy. An effective method of surgical treatment is radiofrequency ablation (RFA) of pathological heart rhythms. However, for many patients, antiarrhythmic therapy may not be effective, and RFA is contraindicated due to the anatomical features and severity of the patient’s condition. In such a situation, pacemakers with ICD function are the best method and choice to prevent serious complications of VT.
It is obvious that severe forms of HF are often accompanied by attacks of VT, the occurrence of which can be fatal for a patient with HF. Many studies conducted around the world have confirmed the high effectiveness of implantable pacemakers with CRT/ICD functionality.
Thus, CRT/ICD provides resynchronization therapy for severe forms of heart failure and high protection against the risk of death from life-threatening arrhythmias and cardiac arrest.
Indications and contraindications for CRT/ICD implantation
Indications for implantation of CRT/ICD cardiac resynchronization devices are determined by your doctor based on your medical history and medical studies.
Indications for CRT/ICD implantation:
- Moderate and severe degree of heart failure (III-IV functional class), when the symptoms of heart failure are not amenable to drug therapy in compliance with all diet regimens (water restriction, etc.).
- Decreased contractility of the heart. The ejection fraction is equal to or lower than 35%.
- Uncoordinated contractions of the ventricles with the manifestation of electrical dyssynchrony of the myocardium on the electrocardiogram (QRS duration greater than 120 milliseconds), and/or during an echocardiographic study with the identification of mechanical dyssynchrony of the walls of the myocardium of the left ventricle.
Patients with heart failure who are not candidates for CRT/ICD implantation and who do not meet the indications for cardiac resynchronization (as determined by the treating physician):
- Patients with moderate heart failure (functional class I-II), whose symptoms are well controlled by drug therapy and diet.
- Patients whose heart failure is not associated with uncoordinated ventricular contractions (no dyssynchrony).
High technologies in the treatment of cardiac arrhythmias
Republican Scientific and Practical Center "Cardiology"
D. Goncharik, leading researcher at the laboratory of cardiac arrhythmias, candidate of medical sciences, associate professor
Irregular or fast beating of the heart is called arrhythmia. There are many different types of arrhythmias - from the usually harmless atrial extrasystoles to the truly life-threatening paroxysms of rapid ventricular tachycardia. An episode of acute rapid heartbeat is called paroxysm. Many arrhythmias can respond well to treatment with medications or disappear with rest (vacation), reducing alcohol consumption, caffeine, and quitting smoking.
*****
However, in some patients, arrhythmias occur so frequently that they interfere with normal life or cannot be treated with medications. In such cases, modern cardiology has a wide arsenal of highly effective minimally invasive and surgical treatment methods. “Minimally invasive” means that elimination of arrhythmia is achieved using special catheters that are inserted into the heart through the vessels of the legs, without cutting the chest, and the patient is conscious only under local anesthesia, without experiencing pain.
This procedure is called ablation, a complex, high-tech heart surgery. On average it takes several hours. Such minimally invasive operations are the most effective method of treating heart rhythm disorders, as they allow patients to completely get rid of arrhythmia.
First, several catheters are inserted into the patient through the veins and/or artery of the thigh under local anesthesia - thin wires that make it possible to record an electrocardiogram of the heart directly from the inside. This is necessary to correctly establish the diagnosis and further treatment tactics. The doctor can control the movement of the catheter tip inside the patient's body using a special device. Such intracardiac cardiograms, recorded from several points, make it possible to most accurately diagnose arrhythmia and determine its source.
After the doctor determines the point in the heart that is responsible for the arrhythmia, it can be eliminated using a special ablation catheter. An ablation catheter differs from other catheters inserted into the heart in that its tip can heat up to 45 - 60 C and “cauterize” the source of the arrhythmia.
All ablations have some risks, although they are usually not particularly dangerous. Fortunately, complications occur in only about 1% of patients. The most common types of arrhythmias that can be successfully treated with catheter ablation in a single procedure are atrioventricular nodal and some other atrial tachycardias, atrial flutter and fibrillation, WPW, and some types of ventricular tachycardias. Unfortunately, not all types of arrhythmias can be successfully eliminated using modern treatment methods, but science and technology do not stand still and new technologies are being introduced every year.
*****
One of the most common types of tachycardia (fast heartbeat) in young people is atrioventricular nodal paroxysmal tachycardia. With such an arry inside the atrioventricular node (connection). To prevent repeated paroxysms of tachycardia, prophylactic administration of special medications may be required. However, most patients do not want to take medications for a long time: they stop taking them or take them irregularly, so attacks of arrhythmia recur. Lasting recovery of patients suffering from such tachycardia can be achieved by cauterization (ablation). To do this, it is necessary to cauterize a small area in the atria in the area of the AV junction and thus break the ring along which the arrhythmia “runs.” After this, it completely disappears and the patient feels like a completely healthy person.
Another arrhythmia that often requires calling an ambulance is arrhythmia in patients with Wolff-Parkinson-White syndrome (or WPW syndrome). WPW syndrome is a congenital defect—an additional abnormal conduction pathway (besides the normal atrioventricular junction) through which impulses can also travel from the atria to the ventricles and vice versa, causing severe cardiac arrhythmias. Some of these arrhythmias can be truly life-threatening.
Patients with WPW syndrome often require special medications to prevent heart rhythm disturbances. It should be noted that although medications can usually provide some control of arrhythmia attacks, complete resolution of symptoms cannot be achieved with medications alone. Therefore, many doctors recommend catheter ablation as the best treatment method.
It is often difficult to localize this additional pathway, but modern computer equipment can significantly increase the efficiency of operations.
One of the most common cardiac arrhythmias in middle-aged and elderly people is atrial fibrillation. In atrial fibrillation (AF), the upper chambers (atria) of the heart contract chaotically and uncoordinatedly (fibrillate) at a rate of approximately 400 times per minute. This chaotic heart rhythm has an adverse effect on the heart, which ultimately leads to the formation of heart failure.
In most cases, patients experience palpitations, dizziness, shortness of breath and fatigue. For some, atrial fibrillation is completely asymptomatic. The tricky thing about atrial fibrillation is that it can cause strokes.
A new episode of arrhythmia is called paroxysm. When AF paroxysm persists for a long time, blood clots (thrombi) can form in the atria, which travel through the bloodstream into the arteries and cause their blockage. The area of tissue that does not receive oxygenated blood dies. The most dangerous is the entry of blood clots into the arteries of the brain, which is accompanied by a stroke. To prevent strokes, patients must take blood thinners such as aspirin or warfarin.
Restoring the rhythm in a patient with atrial fibrillation can be achieved with pills or intravenous medications, or with an electrical shock (electrical shock therapy).
It is extremely important not to delay restoring the rhythm, because if paroxysm persists for a long time, this can be difficult. For example, if a patient's paroxysmal AF persists for more than 48 hours, clots may form in the heart. Before restoring the rhythm, the doctor must make sure that the patient does not have thrombi (blood clots) in the cavities of the heart. For this purpose, transesophageal echocardiography (ultrasound of the heart using a probe similar to a gastric tube) is performed or the drug warfarin is prescribed for 3 to 4 weeks immediately before the cardioversion procedure to thin the blood.
Although electrical cardioversion can restore normal heart rhythm in approximately 90% of patients, unfortunately, in a significant proportion of patients, the rhythm is re-disturbed within a year for various reasons. If AF recurs repeatedly, the doctor decides whether it is advisable to restore the rhythm again in a particular situation or whether it makes sense to transfer AF to a permanent (chronic) form.
Some patients cannot maintain rhythm with medication. There are modern surgical and minimally invasive treatment methods for them.
*****
The labyrinth type surgery is performed under general anesthesia while the heart is stopped. The right and left atria are cut with a scalpel and then stitched together. In this way, it is possible to form a normal “path” for the propagation of a normal rhythm from the atria to the ventricles. However, this operation is complex and requires cutting into the chest.
Physicians with experience in treating cardiac arrhythmias are constantly developing new methods to identify the sources of arrhythmia without cutting into the chest (mapping) or cauterizing the sources of atrial fibrillation so that AFib disappears once and for all.
The mapping and cauterization procedure has been in use since the late 1990s, with new variations being introduced every year. During the ablation procedure, doctors use special catheters to eliminate the sources of arrhythmia in the atria, and if there are too many such areas, they “isolate” them from healthy heart tissue by drawing circular ablation lines. This is a rather complex and lengthy procedure, lasting several hours. Sometimes it is carried out in several stages. The advantage of this invasive operation is that it is performed under local anesthesia; the patient is conscious, there is no need to cut the chest.
Currently, the best results are achieved using a special catheter navigation system inside the heart cavity (CARTO system), which allows you to control the catheter that cauterizes arrhythmia inside the heart cavities with an accuracy of 1 mm. This catheter allows you to build a map of arrhythmia.
The procedure is more effective for patients with frequent short paroxysms of AF; the effectiveness against long-standing AF is significantly lower.
The AF ablation procedure is not without risks. About 2 to 3% of patients experience serious complications such as blood leaking into the heart (tamponade), strokes, nerve damage, narrowing of the pulmonary veins, or a hole forming between the atria and esophagus (atrioesophageal fistula). Many of these complications are treatable but require the patient to remain in the clinic for an extended period of time.
Therefore, to decide on the advisability of a procedure, the doctor weighs the potential benefits and possible risks for a particular patient, choosing the optimal solution for the given case at the time.
*****
Atrial flutter is often an arrhythmia related to atrial fibrillation, in which the atria contract at a high rate of up to 200 to 300 beats per minute, and this rapid rhythm is conducted to the ventricles and causes them to contract at a rate of 100 to 150 beats per minute. This leads to rapid disruption of the normal pumping function of the heart. Treatment of atrial flutter with medications is usually ineffective.
The best treatment for atrial flutter is ablation (cauterization), which produces positive results in approximately 90% of patients.
Excessively fast heartbeats that originate from the heart's ventricles are called ventricular tachycardia (VT). This arrhythmia often poses a serious threat to the patient's life, often leads to loss of consciousness and requires the use of special medications, the use of invasive (catheter ablation) or even surgical treatments.
Typically, severe ventricular tachycardia is treated by sewing a special device under the skin - an implantable cardioverter-defibrillator (ICD), which allows you to interrupt severe attacks of arrhythmia using an electrical discharge from the inside.
Some forms of ventricular tachycardia are less life-threatening and occur in people with nearly normal heart function. Although these forms of the disease can be treated with medications, a permanent cure can be achieved with the help of an ablation procedure and save the patient from repeated breakdowns once and for all. Sophisticated computer systems make it possible to create a map of cardiac excitation during such tachycardia, which makes it possible to identify its source.
Often, a paroxysm of ventricular tachycardia develops into an even more severe arrhythmia - ventricular fibrillation (VF), in which the heart contracts uncoordinatedly at such a high speed that it is unable to pump blood, and this is tantamount to cardiac arrest. With ventricular fibrillation, a person always loses consciousness.
There are many causes of VT and VF, but most often it occurs due to disruption of the blood supply to the heart muscle due to narrowing of the coronary arteries or the presence of scars in the heart muscle. The most effective means of stopping repeated paroxysms of ventricular fibrillation (rhythm restoration) are implantable cardioverter defibrillators (ICDs).
An ICD is an implantable device (similar to a pacemaker) that monitors the heart's rhythm. Unlike a pacemaker (which prevents the heart from beating too slowly), an ICD can also detect and interrupt excessively fast heartbeats - ventricular tachycardia, as well as ventricular fibrillation. If a severe arrhythmia occurs, the cardioverter-defibrillator commands the restoration of the normal rhythm (using a series of rapid electrical impulses or an electrical discharge from the inside). Information about each episode can be downloaded using the programmer and can be read from the ICD memory without cutting the skin. The clinic of the Republican Scientific and Practical Center "Cardiology" has sufficient experience in treating such patients.
In general, the lives of patients with ICDs are almost no different from the lives of other people. Although ICDs successfully treat VT and VF but do not prevent them, patients should avoid situations where they might lose consciousness in a life-threatening situation, such as during unaccompanied swimming, etc. If the patient is touched by another person at the time of the shock, You may feel a slight, momentary tingling sensation, but it poses absolutely no danger. Modern ICDs last for four to six years before the generator needs to be replaced.
Electrical system of the heart
The heart has its own electrical (conducting) system, consisting of an electrical impulse generator - the main pacemaker (sinus node) - and conduction pathways (atrioventricular junction, His bundle and its branches) connecting the entire electrical circuit. The main pacemaker (sinus node), located in the right atrium, generates regular electrical impulses at a certain frequency, like a metronome. In response to each impulse, the heart contracts in a strict sequence - first the atria, then normally through a single connection (atrioventricular, in which its short-term delay occurs), the impulse passes to the ventricles, spreading through the system of fibers, causing the ventricles to contract synchronously.
Bradycardia and pacing
At rest, our heart beats at approximately 50 to 90 beats per minute, although athletes and patients taking certain medications, such as beta blockers, may contract slower. Heart rate increases during exercise, and the maximum varies greatly among individuals.
A slow heartbeat (bradycardia) may cause no symptoms or may cause dizziness, blurred vision, shortness of breath, or fatigue. Bradycardia can occur due to problems with the main pacemaker of the heart (sick sinus syndrome) or a delay in the impulse at the atrioventricular junction (heart block).
Patients with high-grade heart block and sick sinus syndrome usually have a pacemaker fitted.
Pacemakers
A pacemaker is an implanted device that monitors a person's heartbeat and prevents the heart from beating too slowly.
It consists of a “pulse generator” (the pacemaker itself) to which one or two wires (electrodes) are attached. Typically, the pacemaker is placed under the skin or in the muscle just below the collarbone. Almost all modern pacemakers work “on demand”, that is, they turn on only when necessary - when the heartbeat is too slow to set the correct rhythm. The rest of the time, the device only monitors the patient’s own heart rhythm without interfering with its work.
There are many different types of pacemakers available today. Belarusian clinics have all the necessary types. There are physiological pacemakers: they can recognize when the patient is sleeping or, conversely, doing hard work. In response to exercise (fast walking or running), the stimulator increases the heart rate, and at night, on the contrary, it works even slower than during the day at rest.
The service life of modern pacemakers under standard conditions is approximately 7 - 10 years, but can be much longer for a particular patient. The expiration date of the pacemaker battery can be easily predicted during the next scheduled check of the pacemaker.
The pacemaker imposes almost no restrictions on the patient's daily life. Household appliances and mobile phones do not interfere with the operation of the device, although you should not store a mobile phone in a pocket near a pacemaker.
Heart failure
With severe damage to the heart by various diseases, its pumping function gradually decreases. When the pumping function is significantly reduced, the heart is unable to pump the required amount of blood, which is called heart failure.
Most cases of heart failure are caused by the fact that the main pumping chamber of the heart (the left ventricle) cannot contract with sufficient force, but usually the right and left ventricles continue to contract synchronously (almost simultaneously).
Resynchronizing pacemaker
As heart failure increases, the right and left ventricles begin to contract at the same time - the contraction of the left ventricle or part of it is greatly delayed in relation to the right ventricle. Asynchronous contraction further reduces the efficiency of the heart's pumping function. To treat such patients, special stimulants are used. The goal of cardiac resynchronization therapy (CRT) is to stimulate the ventricles so that they contract simultaneously, thereby improving the pumping function of the heart.
In general, the implantation procedure is similar to the procedure for implanting a conventional pacemaker. The only difference is that an additional electrode is inserted to set the correct rhythm to the left ventricle and synchronize the work of the right and left ventricles.
Currently, implantation of pacemakers, including physiological ones, is performed in all regional centers of Belarus. Implantation of more complex devices - resynchronizing pacemakers and cardioverter-defibrillators - is carried out in the republic.
It is important!
Attacks of dizziness and loss of consciousness
Approximately 30 - 50% of people experience fainting or blackout at some point in their lives. Fainting occurs for a variety of reasons, but the immediate common cause is usually a sudden drop in blood pressure, which in turn leads to a short-term reduction in blood flow and oxygen delivery to the brain.
Usually, but not always, a person immediately before losing consciousness feels lightheaded or dizzy, and also complains of darkening of the eyes and ringing in the ears. In addition, nausea, vomiting, sweating, and rapid or slow heartbeat may occur.
Fainting among people of all ages is so common that many do not immediately perceive it as a serious threat to life and may seek professional help from a doctor only after a series of fainting spells, which is a mistake.
The most common type of fainting is due to improper reflex interaction between the cardiovascular and nervous systems, as a result of which the cardiovascular system selects a heart rate and degree of relaxation of the body’s blood vessels that is inadequate to the current situation. In addition to the so-called functional, or “reflex” forms of fainting, patients may also lose consciousness due to organic heart diseases: excessively fast or slow heartbeat, dysfunction of the heart muscle or heart valves, as well as diseases of the nervous system and overdose of drugs that lower blood pressure. Differential diagnosis usually requires an electrocardiogram, as well as an ultrasound scan of the heart or “echocardiogram”, etc.
Doctors may recommend that patients who complain of recurrent “reflex” fainting avoid certain situations that lead to fainting (for example, standing up on a crowded train in hot weather), wear medicated compression stockings, prescribe certain medications, and in some cases, get a pacemaker. if such fainting is accompanied by an excessive slowing of the heart rate.
To diagnose disease of the heart muscle and/or heart valves, certain non-invasive tests are available, such as 24-hour continuous recording of heart rate and rhythm using an ECG (Holter ECG monitoring). In some cases, invasive tests may be required, such as coronary angiography (cardiac catheterization) and/or specialized tests of the heart's electrical system, known as an electrophysiological study, or EPS.
In patients suffering from organic heart muscle disease, fainting often occurs due to an excessively fast heartbeat. In such a situation, the heart simply does not have time to emit the amount of blood necessary to ensure normal functioning of the brain, and the doctor may raise the question of a special heart operation to eliminate or cauterize the source of such arrhythmia. In some cases, it may be decided to implant a special device under the skin, similar to a pacemaker, which will restore excessively fast heartbeats using an electrical current discharge from the inside (ICD).
The main thing is that if fainting occurs, you should not wait for it to recur many times (since the second or third may already be the last), but quickly seek help from a specialist.
What is ICD?
An implantable cardioverter defibrillator (ICD) is used to treat heart rhythm problems in which your heart beats too quickly or irregularly. When the ICD detects a heart rate that is too fast, it sends electrical impulses to your heart. These impulses can restore normal heart rhythm. The ICD combines a pacemaker and a defibrillator; its main functions will be described in detail in the sections of this brochure. The ICD is implanted in the upper chest and is small in size, about the size of a small child's palm or the size of a pager. Implantation is performed strictly according to confirmed indications, after research has been carried out according to the doctor’s recommendations.
Subsequent visits
After the stimulator is implanted, your doctor will schedule your next visit. It is important to remember that your health now largely depends on the correct functioning of the ICD. The effectiveness of such therapy depends on a properly selected ICD program and antiarrhythmic therapy. The frequency of consultations will be determined by your attending physician, and it will depend on your state of health and heart rhythm disorders.
During your consultation, your doctor will use a programmer to evaluate the performance of the ICD.
Your doctor will test your ICD:
• check the operation of the pacemaker;
• check the effectiveness of the main functions;
• check the battery capacity;
• will check the chronology of all events recorded by the ICD;
• if the ICD discharged the defibrillator, the doctor will evaluate the effectiveness of the therapy and possibly make adjustments to the stimulator program. After programming, the doctor may change antiarrhythmic therapy or prescribe additional tests. It is important to remember that the performance of your ICD depends on the settings of the basic functions and the correct antiarrhythmic therapy. Therapy is needed to exclude possible attacks of dangerous ventricular arrhythmias.
Why does my doctor recommend ICD implantation?
A patient’s circulatory arrest can occur due to conduction disturbances (blockades), ventricular fibrillation and ventricular tachycardia.
If a person is at high risk of circulatory arrest for this reason, a cardioverter-defibrillator is implanted. In addition to the stimulation function for bradysystolic rhythm disturbances, it has the function of interrupting ventricular fibrillation (as well as ventricular flutter, ventricular tachycardia).
ICDs are implanted:
- patients who have had episodes of sudden cardiac death or ventricular fibrillation;
- patients who have had a heart attack and are at high risk of sudden cardiac death;
- patients with hypertrophic cardiomyopathy and at high risk of sudden cardiac death;
- patients who have had at least one episode of ventricular tachycardia;
Are there alternative treatments?
Heart rhythm disturbances are a very complex branch of cardiology. The human heart works throughout life. It contracts and relaxes 50 to 150 times per minute. During the systole phase, the heart contracts, ensuring blood flow and delivery of oxygen and nutrients throughout the body. During the diastole phase it rests. Therefore, it is very important that the heart contracts at regular intervals.
Heart rhythm disturbance is a disturbance in the frequency, rhythm and sequence of contractions of the heart muscle. Heart rhythm disturbances can occur in different parts of the heart and manifest themselves in the form of extrasystole (extraordinary contraction) or a very fast rhythm (tachycardia). As a rule, heart rhythm disturbances are divided into functional (reversible) and organic (non-reversible). Functional disorders include those types of heart rhythm disturbances that are caused by endocrine and metabolic disorders, poisoning, alcohol use, and severe stress. Timely correction and elimination of the causes of arrhythmia leads to recovery.
The most dangerous arrhythmias are considered to be those rhythm disturbances that are caused by damage or changes in the myocardium, which are observed with myocardial infarction, myocarditis, cardiosclerosis, arrhythmogenic dysplasia of the right ventricle, etc. Most cardiac arrhythmias are amenable to antiarrhythmic therapy. An effective method of surgical treatment is radiofrequency ablation (RFA) of pathological heart rhythms. However, for many patients, antiarrhythmic therapy may not be effective, and RFA is contraindicated due to the anatomical features and severity of the patient's condition. In such a situation, pacemakers with ICD function are the best method and choice to prevent serious complications of VT.
Who is not eligible for ICD implantation?
Not all patients are candidates for ICD implantation. In many patients, tachyarrhythmia is temporary or in cases where the use of an ICD cannot eliminate the cause of the underlying disease.
These include:
- Patients whose tachyarrhythmias are associated with a reversible cause, such as treatment for drug addiction, electrolyte imbalance, etc.
- Patients with tachyarrhythmias as a consequence of a heart attack or non-sustained episodes of myocardial ischemia.
- Patients with frequent episodes or continuous VT.
- Patients whose tachyarrhythmias occurred after a lightning strike or electric shock.
Should I be concerned about my ICD?
The ICD is designed to improve quality of life by helping overcome symptoms and provide confidence in the face of the consequences of sudden cardiac arrest. Remember, your ICD is there to protect you from tachyarrhythmias. ICD pacemakers are extremely reliable—they save lives every day.
Give yourself and your family time to adjust to life with an ICD. Most patients quickly get used to it. However, some people feel depressed, anxious, and afraid. If these feelings do not go away after 2 months, consult your doctor. You can also consult with another person who has undergone a similar operation and ask them how they and their family members have adjusted. Over time you will feel confident. You will be able to return to work, normal activities and family life. Your family can help you. You need to give her information about the cardioverter defibrillator and what help you may need.
Replacing the ICD battery
The ICD is equipped with a large-capacity battery, which lasts for many years of uninterrupted operation. The battery drains gradually and predictably. Each time the ICD is checked, information about the state of the battery capacity appears on the programmer. If the battery reaches the end of its capacity, your doctor will warn you several months in advance and work with you to schedule ICD replacement surgery.
During surgery, the old ICD will be removed and replaced with a new one. A skin incision will be made along the old scar, and the stimulator will be placed in a ready-made pacemaker bed. As a rule, repeated operations are performed quickly, the recovery period is very short.
During the operation, the electrodes will be tested, the resistance at the end of the electrode, the stimulation threshold and sensitivity will be measured. If the lead shows no signs of damage and its electrical conductivity is intact, it will be attached to a new ICD.
In very rare cases, it may be necessary to replace the electrode. Ask your doctor for more information.
Will I experience pain or discomfort?
Adaptation to ICD occurs gradually. First of all, follow your doctor's advice. Most patients feel “protected” from the disease and are able to return to a full, active life.
After the wound has healed, pain is unlikely; discomfort at the site of the stimulator will persist for some time when raising the arm. Typically, many patients forget that they have an ICD implanted. After the scar has formed, only a thin light strip remains.
WARNING: Consult your doctor if you continue to experience pain after your wound has healed.
Upon discharge from hospital
Your doctor will tell you what kind of suture is used to close the edges of the wound at the site of the implanted ICD. In most cases, “absorbable” threads are used to suture the skin, which are not removed due to their complete dissolution in the tissues after a few weeks. In rare cases, single sutures are used, which must be removed 7-10 days after surgery. You will experience pain in the area of the implanted ICD and the skin suture for several days.
Always follow your doctor's instructions until you have fully recovered and resumed normal work activities.
For some time after surgery, you will probably be aware that you have an ICD implanted. This is a normal feeling and usually goes away with time. In the first days, you may experience discomfort in the incision area. The area may become red and inflamed. In some cases, an increase in temperature is observed. Usually all these phenomena are treated with medications that the doctor will prescribe to you.
Sometimes a “twitching” occurs over the location of the stimulator.
It is completely safe and is caused by a tiny electrical current produced by the ICD, which can excite surrounding tissue. After some time, such phenomena usually disappear spontaneously or are eliminated by reprogramming the ICD.
Such complications occur in a small percentage of patients. At the same time, the vast majority of pacemaker owners have absolutely no problems with their devices.
It will be necessary to carry out antibacterial therapy and change the regimen of previously (before surgery) prescribed drug therapy. Very often, antihypertensive drugs are canceled or reduced. This is due to the fact that with a regular heart rhythm generated by the ICD, blood pressure levels are stabilized to normal values.
Soon you will begin to forget that you are wearing an artificial pacemaker. Symptoms indicating an irregular heart rhythm will decrease and soon disappear completely. Gradually, as you feel better and follow the advice of your doctor, you will be able to return to your normal activities.
Some recommendations for quick recovery:
• the use of baths and physical exercises must be regulated by a doctor;
• try not to lift anything heavy for several weeks;
• hand movements should not cause pain in the pacemaker area;
• do not wear tight clothing that may irritate the skin over the pacemaker;
• Avoid any contact that could injure the soft tissue over the ICD.
When you visit your doctor, be sure to tell him or her that you have an ICD implanted.
WARNING : Tell your doctor immediately if there is redness, swelling, warmth, or discharge from the surgical incision at the implanted ICD site. This may indicate an infectious process and have serious consequences.
Contact your doctor if your arm is swollen and pain persists, and if you develop a fever several days after surgery.