What complications can occur after stenting of the coronary arteries and heart vessels?
Complications after stenting can occur both immediately after surgery and in the long term. Immediately after implantation of the endoprosthesis, it is possible to develop allergic reactions to medications used during the intervention or over the next few days. Some stents have special coatings that contain substances whose action is aimed at preventing re-narrowing of the vessel. Patients predisposed to allergies may have a reaction to their release into the blood.
When performing stenting of cardiac vessels, complications may include repeated narrowing of the lumen of blood vessels and the formation of blood clots. These are the most common complications, and the attention of medical scientists is currently focused on combating and preventing them. Complications after stenting cannot be excluded, such as the occurrence of perforation of the vessel walls, the development of bleeding and the formation of hematomas at the site of catheter insertion or other parts of the path of passage of the balloon with the stent.
Repeated stenting
The patient’s most common question after stenting is how long the stents will function and whether repeat stenting is possible.
It should be noted that the vast majority of people who undergo this procedure do not have any complications and live with an implanted stent all their lives, since they are made from materials that can perform their intended function constantly, that is, for decades.
This occurs due to the fact that some time after the operation the stent begins to become overgrown with endothelial cells, becoming one with the arterial wall. But there are cases when stent restenosis occurs. More often this happens when a stent is installed at the location of a large atherosclerotic plaque or a large extent of vessel narrowing.
Recently, in order to prevent restenosis, specialists have begun to actively use drug-eluting stents, from which, after implantation into the coronary vessel for several weeks, a pharmacological drug is released that prevents excessive growth of the intima (inner lining) of the artery and the increase in atherosclerotic plaque. Taking into account modern capabilities, successful results of stenting are observed in 95% of patients who have undergone it.
The choice of a specific type of stent is determined by an x-ray endovascular surgeon based on diagnostic data obtained during a preliminary examination of patients, as well as concomitant pathology (for example, diabetes mellitus).
Non-drug drug therapy reduces the likelihood of restenosis: lifestyle changes, regular dynamic physical activity, quitting smoking, proper nutrition, taking drugs to prevent thrombosis (aspirin and clopidogrel) for a year, constant use of statins in adequate doses under the control of biochemistry and other drugs for the treatment of coronary heart disease.
Often the cause of deterioration is not restenosis of an already installed stent, but the progression of atherosclerosis in other coronary arteries with the development of severe stenosis. Therefore, after stenting, if you have new attacks of angina or decreased tolerance to physical activity, you need to consult a doctor for further examination: echocardiography, stress tests. If ischemia is confirmed, you will be offered a repeat coronary angiography.
Based on its results, it is determined which vessel is affected. If stent restenosis has developed, then there are 2 ways to get rid of it: the stent blocked by a thrombus is expanded with an air balloon inserted into it (angioplasty) or another stent is inserted inside the blocked stent. If stenoses are detected in other previously unaffected arteries, then stenting is performed.
How to avoid complications after stenting of heart vessels and coronary arteries
Patients most prone to complications after coronary artery stenting are those with various serious chronic diseases - kidney pathologies, diabetes mellitus, various disorders of hematopoietic and coagulation functions. Factors that increase the risk include old age and poor general condition of the patient’s body at the time of surgery.
In order to prevent the development of complications associated with the above reasons during coronary artery stenting, a thorough examination of the health status of the candidate for angioplasty is carried out even at the stage of preparation for the operation. This includes not only an assessment of the condition of the blood vessels, but also a comprehensive examination with attentive attention to all the patient’s complaints, taking into account all the medications he is taking and their possible reactions with medications administered during and after the operation.
The role of coronary artery stenting in patients with stable coronary artery disease
Transcript of the author's program by Professor S.R. Gilyarevsky, broadcast on March 14, 2012.
Drapkina O.M.: - Good evening, dear colleagues! We continue meetings within the framework of the evidence-based cardiology program. And again with you is the author and presenter - Professor Sergei Rudzherovich Gilyarevsky, scientific director of the department of emergency cardiology of patients with myocardial infarction at the Scientific Institute named after. Sklifosovsky.
Gilyarevsky S.R.: - Good evening. Yes, the Institute of Emergency Medicine named after. Sklifosovsky. And, probably, Oksana Mikhailovna wanted to say that I am visiting your program today as a representative of emergency cardiology.
Drapkina O.M.: - No, I can’t say that, you’re at home. As a representative of emergency cardiology and why - because today we will talk specifically about a fragment of this emergency cardiology, namely, stents. Sergei Rudzherovich, you are always in store, somewhere looking for evidence of such sometimes sensational facts. What awaits us today? What are we going to talk about?
Gilyarevsky S.R.: — We will talk about the role of coronary artery stenting in patients with stable coronary heart disease. And, probably, for us, cardiologists in Russia, this is much easier to discuss than, say, for interventional cardiologists, since abroad there is no division between (as far as I know) interventional cardiologists and specialists in X-ray endovascular treatment methods, because in general, recently There has been a trend towards a more cautious determination of indications for coronary artery stenting. And in one of the programs, if you remember, we presented a case published in the Journal American Cardiology, where one patient had 67 stents implanted, and the patient had both coronary artery bypass surgery and then stenting simply in the coronary arteries , and in shunts. And, of course, this approach, which is a consequence of such a negative phenomenon, which is designated by the term “stenism.” Stentism is when the decision to implant a stent is made by the operator, although now all clinical guidelines say that the decision to stent in most cases or in some doubtful cases should be made taking into account the clinical manifestations of the disease.
Drapkina O.M.: - Who is the operator?
Gilyarevsky S.R.: — The operator is the person who directly installs the stent. Naturally, there is no need to stent everything that is narrowed. There are special methods that allow you to identify hemodynamically significant arteries. Of course, stress tests are also performed, but, unfortunately, stress tests are not always so sensitive, and sometimes not even so specific, as to refuse to perform coronary angiography. There are methods for assessing hemodynamic significance by determining the fractional reserve of blood flow of the coronary arteries, when they look at the difference between the aorta and the distal coronary artery. And if the difference in pressure is 20%, then the issue is resolved after stimulation with aminazine and vasodilators, then a decision is made about stenting the coronary artery.
But again, this still needs to be approached individually. And the complexity of the evidence-based history in this area lies in the fact that the first studies, a meta-analysis of which indicated a positive effect of angioplasty on prognosis compared to drug therapy, were performed when, firstly, there was no stenting of the coronary arteries, it was only angioplasty, on the one hand. This could reduce the effectiveness of the intervention. On the other hand, there was no drug therapy like what we have now. Those. the patients took anti-ischemic drugs, and ACE inhibitors, and that’s it. There were no statins that fundamentally changed the course of coronary heart disease. And therefore, the results of a meta-analysis, which was published not so long ago in the journal Archives of Internal Medicine, are of interest, in which they tried to analyze what effect coronary artery stenting has, i.e. angioplasty with stenting on the course of coronary heart disease compared with optimal drug therapy. Those. stenting with therapy and one optimal therapy.
During the course of this analysis, 8 randomized clinical trials were included in this analysis, and if you see, such famous studies as the COURAGE trial, the OAT trial, the BARI 2D trial. In the course of, say, the COURAGE study, if we recall, patients with coronary heart disease were compared with either standard therapy, which included very powerful lipid-lowering therapy regimens, i.e. there, patients received statins and most patients received ezetimibe, and the level of low-density lipoprotein cholesterol actually decreased to the levels that are given in the recommendations.
Against this background, stenting did not lead to a statistically significant improvement in prognosis. The well-known BARI 2D studies have been performed in diabetic patients with inducible ischemia or angina and found similar results. You can see on this slide what the characteristics of the patients were: the average age is about 60 years, as always in such studies, patients with coronary heart disease were mostly men. Diabetes mellitus was presented differently - you see, from 14 to 100% of the BARI 2D study had previously suffered a heart attack, in some studies all patients, in particular in the OAT study, which assessed the effectiveness of coronary artery angioplasty in the majority with stenting in patients at long-term terms after acute myocardial infarction, relatively long-term, 3-28 days after the development of symptoms of myocardial infarction. And the number of vessels that were tampered with was not so large. On average, this is an intervention on one or two, mostly on one vessel. And this, too, probably influenced the results of the study, including the meta-analysis, since it is well known that with single-vessel lesions, drug therapy is...
Drapkina O.M.: - Undoubtedly better.
Gilyarevsky S.R.: - Yes. But, nevertheless, such a meta-analysis was performed, and in this slide, indeed, it confirms that the therapy was very good. Patients received both antiplatelet agents and a beta blocker, most of the patients received ACE inhibitors (in most studies there was still a high frequency of use) and the use of statins from 45 to 100%. It is very important that this is a modern stage. The data that was obtained earlier concerned the previous stages, when the therapy was not so effective. Now this is what happened against the backdrop of such highly effective therapy. Here's what happened. As you can see, coronary artery stenting in patients with stable coronary artery disease did not lead to a decrease in overall mortality compared with optimal drug therapy.
The next indicator is the incidence of non-fatal myocardial infarction. And here (at first glance, these data may seem paradoxical) there is a clear tendency to increase the risk of developing non-fatal myocardial infarction with stenting compared... i.e. clear advantage of optimal drug therapy. Why? They explain it this way. Firstly, intervention on the coronary artery, stenting of the coronary artery - after all, the participation of patients is accompanied by embolization of the distal sections. This can lead to the development of myocardial infarction. Of course, this myocardial infarction usually does not have the same clinical significance as spontaneous myocardial infarction, and diagnostic approaches have also been very different. Some authors believed that any increase in troponin levels after intervention is a consequence of clinically significant necrosis, but now it has become clear that this is not so, that troponin increases quite often and that it is better to focus in this situation, oddly enough, on the concentration of CPK. And it is believed that if after the intervention the concentration of creatine phosphokinase increases 5 times, the MB fraction increases 5 times or more compared to the upper limit of normal, then this already indicates a clinically significant heart attack associated with the intervention.
Drapkina O.M.: — I want to say about the troponin test. Its specificity is within the first 3 hours, sensitivity is 33%.
Gilyarevsky S.R.: - Yes, special sensitivity. If it is coronary heart disease, and you know that the patient had ischemia and there is an increase in the concentration of troponin in the blood over time, then this is still a fairly specific method. If there is no dynamics, then, of course, an increase in troponin levels may occur in patients with renal failure or heart failure. But there should be no dynamics there.
Drapkina O.M.: - It’s no coincidence that the latest recommendations are already included twice, because the first ones are these...
Gilyarevsky S.R.: - Even now it is proposed to take such an algorithm with an interval of 3 hours upon admission. And if there is dynamics and at least one indicator exceeds 99%, then we can already talk about a diagnosis of a heart attack.
Drapkina O.M.: - But the biggest one is day 4.
Gilyarevsky S.R.: - Still, yes. But in this case, increasing the level of troponin is not enough... it is too sensitive, because slight damage to the myocardium can occur and embolization in areas, destroyed plaques, this happens. Therefore, in order for the diagnosis of “heart attack” in this case to truly reflect the clinical situation, they began to focus on MB, CK, if it increases 5 times compared to the upper limit of normal, then yes. If we go back to the slides and try to explain these results further. Why does coronary artery stenting in patients with stable coronary heart disease not reduce the risk of developing a heart attack? Yes, because, paradoxically, the affected area of the artery that causes the development of angina pectoris, as a rule, does not cause the development of a heart attack, because angina pectoris develops where there is a dense, usually large, hemodynamically significant plaque, and it does not is torn. And myocardial infarction occurs precisely in those areas of the coronary arteries that do not cause the development of myocardial ischemia. Even if the patient has stable angina, his heart attack does not develop due to the area that causes ischemia, so when you restore the patency of the artery in the area that causes the development of ischemia and, accordingly, angina, then you relieve the patient from angina, but you do not influence in any way those areas that later cause the development of myocardial infarction.
This is why drug therapy that targets atherosclerosis as a systemic process and leads to plaque stabilization reduces the risk of heart attack. So there is actually no paradox here, and this, of course, needs to be remembered. Still, the need for unplanned revascularization - the trend was slightly better in the group of patients who had coronary arteries stented... Well, either acute or due to worsening angina pectoris is also possible... Therefore, not all patients here were acute, i.e. revascularization was not only for acute coronary syndrome. But even here you can see how statistically it is better, but there is no statistically significant difference. Those. This graph shows that the confidence interval border still crosses unity. This means that the difference overall is not statistically significant. Well, such an indicator as persistent angina pectoris during observation. It is obvious here that there were positive dynamics in the stenting group. It is clear that stenting still relieves angina, but still does not achieve it, although this was a meta-analysis that included more than 7 thousand patients, i.e. statistical power was quite high. But, nevertheless, there were no statistically significant differences in this indicator. Thus, the authors concluded that to date, the initial tactics of coronary stenting in stable coronary heart disease have no advantage over optimal drug therapy.
Drapkina O.M.: — Most importantly, it should be optimal.
Gilyarevsky S.R.: — The main thing is that therapy should be optimal. Those. optimal therapy is antiplatelet agents, ACE inhibitors, statins and, of course, anti-ischemic therapy, this is understandable. Thus, these data suggest that it is necessary to more carefully approach the issue of stenting the coronary arteries and still, as an initial tactic, if this is a stable course of coronary heart disease, we still use optimal drug therapy, and only in In cases where it does not help, we raise the question of performing stenting. This in no way applies to an acute situation. In acute coronary syndromes, it has been precisely proven that stenting the coronary artery, which led to the development of acute coronary syndrome, myocardial infarction, that its stenting leads to an improved prognosis. And the numbers themselves speak about this. For example, mortality from acute myocardial infarction has decreased from 20% to 5%, and much of the credit lies in the methods of mechanical revascularization. But as for chronic patients, the prognosis of such patients depends largely on the stability of plaques in the coronary arteries as a whole, and not at all on...
Drapkina O.M.: - Sergei Rudzherovich, let’s remind you again at the end of the program. You said optimal therapy. And with a stable course of angina pectoris, the target levels of our main indicators are still the same: lipids, blood pressure, glucose.
Gilyarevsky S.R.: - This is downright difficult, because when it comes to blood pressure levels, then, probably, here the optimal pressure can be considered within the range of 140/80 mm Hg. Art. At least in the large TNT study, where there were 10 thousand patients with coronary heart disease...
Drapkina O.M.: - No higher than...
Gilyarevsky S.R.: — Most likely, not lower, because during this study (and there were all patients with stable coronary artery disease, there were 10 thousand of them), the lowest risk of complications was at a pressure level of 140/81 mm Hg. Art. Therefore, the more severe the coronary atherosclerosis, the more careful the reduction should be, especially for diastolic pressure. If, of course, you perform myocardial revascularization, then these numbers may be lower. But if there is a hemodynamically significant stenosis, it is better to approach carefully. As for the level of glycosylated hemoglobin, today after the ACCORD study it is less than 7. Well, again, if this is the initial stage of diabetes mellitus, then maybe it’s possible here... If this is a transition from prediabetes to diabetes, then, of course , in such patients one should strive for lower numbers. And this, by the way, is also in clinical recommendations that some patients may have less.
But if it is long-standing diabetes mellitus, within 10 years, of course, less than 7 and approach it very carefully, since this can worsen the prognosis, as was the case in the ACCORD study. As for lipids, everything is more or less clear. We can say that European recommendations are even stricter. And the European recommendations say that in any patient with coronary heart disease it is necessary to reduce the concentration of low-density lipoprotein cholesterol to less than 1.8 mmol/l, and this is the main indicator, because the level of triglycerides and the level of high-density lipoprotein cholesterol are still additional indicators. To date, there are no results from clinical studies that would prove that a decrease in these indicators, triglycerides, and an increase in high-density lipoprotein cholesterol leads to an improved prognosis, so we focus on low-density lipoprotein cholesterol and, following European recommendations, and now Russian ones, less than 1.8 mmol/l.
Drapkina O.M.: - Dear colleagues, we again encourage you to write and communicate with us. We are waiting for your suggestions on the topics of our future meetings.
Gilyarevsky S.R.: — And we wish everyone to look for evidence to validate our clinical practice.
Drapkina O.M.: - Thank you.
Gilyarevsky S.R.: - Goodbye. Thank you.
How is stenting surgery performed?
Stenting, like coronary angiography, takes place under local anesthesia, which is very convenient for both the patient and the doctor: the person being operated on is conscious and can communicate.
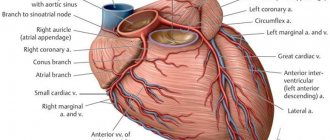
The operation is performed through an injection into an artery in the arm or leg. Thus, a special catheter is delivered into the vessels of the heart, through which a contrast agent is injected so that the operating surgeon can determine which vessel is affected and what length and diameter of the stent must be selected in this case. After the doctor decides on the extent of the surgical intervention, he will need such special tools as a guidewire and the stent itself. A guidewire is a thin metal wire with a diameter of less than 1 millimeter, which is inserted behind the narrowed section of the artery in order to then deliver a balloon catheter to the affected area. Next, dilatation (inflation) of this balloon occurs - the stent expands, is pressed into the wall of the artery and remains in this position: it expands its lumen and restores patency.
After dilatation is completed, the doctor removes the balloon catheter, injects a contrast agent and makes sure that the stent is positioned correctly, the vessel is dilated and there are no complications. At the end of the operation, all instruments, except the stent itself, are removed from the body, and the patient is transferred from the cath lab to the department. Within 24 hours he may be home.
As part of compulsory medical insurance, the patient has access to coronary angiography, stenting of the heart vessels, arteries of the lower extremities and carotid arteries.
Operation description
The essence of this intervention is that a special device, a stent, is inserted into the narrowed artery. Cardiac stenting surgery is endovascular. Before the operation, the patient must undergo tests and have an ECG and an X-ray of the lungs. Operation stages:
- local anesthesia is administered to the groin area (the place where the instrument is inserted);
- a special catheter is inserted into the lumen of the femoral artery, which will be used for manipulation;
- the catheter is gradually passed along the aorta in the direction of the heart, a radiopaque substance is injected through it so that the surgeon can see the condition of the arteries and the location of the catheter on the screen of the X-ray machine;
- Having reached the heart, the doctor injects contrast into the coronary vessels and determines where exactly the narrowing is located;
- A stent is placed in the narrowed area, which is expanded by inflating the balloon located in it.
Are there complications after stenting?
Possible, but they are extremely rare. The most common ones include an allergy to the contrast agent, injury to the arterial wall when installing a stent, a hematoma at the injection site, and the formation of a blood clot in the area of the stent.
To prevent all this from happening, the patient must strictly take special blood thinners, which are prescribed to him even before the operation.
If pain occurs in the area of the heart or at the site of surgical access (where there was an injection into the artery), you must immediately contact the clinic where the operation was performed, and the problem will be eliminated.
When may stenting be needed?
There are several pathological conditions in which this intervention significantly improves the quality and life expectancy, and sometimes even saves. These are the diseases:
- stable angina;
- silent myocardial ischemia;
- acute coronary syndrome with and without ST segment elevation.
All of these are forms of coronary heart disease, which occurs due to partial or complete blockage of the lumen of the arteries that supply the heart muscle. The cause of such blockage is most often atherosclerosis.
Relapses of angina after stenting and bypass surgery
Cardiology Tags:
D. Volyanskaya:
Good cheerful Saturday morning, dear friends! Your favorite channel “MediaDoctor” and the program “Online Reception” are on air. At the microphone is me, Daria Volyanskaya, and my wonderful co-host Yulia Titova. Julia, good morning. Today we have a very interesting guest from the wonderful city of St. Petersburg. This is Rashad Abyshev - candidate of medical sciences, cardiologist, chief physician of the Mentor-Clinic. Hello Rashad.
R. Abyshev:
Hello, good morning.
D. Volyanskaya:
Today we are talking about relapses of angina after stenting and bypass surgery. We want to talk about types of heart surgeries, thrombosis of large arteries, the rehabilitation period, symptoms, and how important it is to monitor your heart and your health. How often should you visit a cardiologist?
R. Abyshev:
Observation by a cardiologist is necessary as needed. We are not talking about medical examination, which is prescribed by state regulations: over 45 years old - once every 5 years, etc. If there are problems, it is better to contact them in a timely manner. Problems in terms of cardiology are complaints of pain that can be noted in the heart area or headaches, which can be symptoms of high blood pressure. Every complaint must be shown to a doctor in a timely manner. Our people are arrogant guys, that’s why people die at the age of 45-48. These are famous people who have the financial ability to be examined without restrictions. But they also die suddenly.
D. Volyanskaya:
What is the most modern diagnostics available today to protect yourself?
R. Abyshev:
The minimum set includes an electrocardiogram, which is the gold standard for research in cardiology; ultrasound diagnostics of the heart is necessary if there are problems with the valves and system and the need to confirm the diagnosis of high blood pressure. Screening for certain blood tests, which includes blood lipids, liver function, kidney function, blood sugar levels, to rule out diabetes. At the clinic, we usually do a check-out format - it can match the budget of the patient who is applying, it can be minimal or maximum. Then we can predict complications that could threaten the life of the patient who contacted us. We give a forecast: for what period of time he can feel calm, what needs to be adjusted in his health.
D. Volyanskaya:
Which patients come to you most often?
R. Abyshev:
Recently, myocardial infarction has become seriously younger. A man can get a myocardial infarction at 43-45 years old. This is often associated with office work and a sedentary lifestyle, which is accompanied by increased body weight. Often these are people with stress loads, in leadership positions. Even if a person is not a leader, he is still nervous, worried, and emotional. There are various disasters in life, so you need to protect yourself from negative elements.
D. Volyanskaya:
What do you most often operate on?
R. Abyshev:
We don't operate. We take patients before and after. Primary complications are when myocardial infarction develops, secondary complications are prevention so that there are no recurrent complications. If a person has had a stroke, the likelihood of developing a recurrent stroke increases 25 times than developing a primary stroke. Therefore, it is necessary to deal with the problem. It is very rarely explained to anyone that a one-time complication or a one-time surgical intervention (after the complication) does not solve the nature of the disease. The processes are based on atherosclerotic changes in the vascular wall. If you have had heart surgery, this does not solve the main problem of atherosclerosis processes. This can easily lead to the development of repeated complications.
D. Volyanskaya:
In what cases do patients consult before surgery?
R. Abyshev:
First of all, patients who have not yet had a heart attack or stroke apply. They address problems that bother them: headaches, pain in the heart. Our task is to verify whether this is related to the pathology of blood vessels and the heart. We make basic diagnostic elements that allow us to diagnose the presence of a problem. Recently, patients came to me from Moscow who complained of high blood pressure. A woman has been recording elevated blood pressure levels since she was 20 years old, but no one has yet identified the problems that could be the cause of these phenomena. During the inspection, we also did not find any serious problems. I think the basis needs to be looked deeper. There are a lot of reasons for arterial hypertension, they do not lie on the surface. If we are talking about patients who have suffered a myocardial infarction, accurate diagnosis, identification of problems and medicinal or non-medicinal adjustments are necessary.
Risk factors are divided into two types: modifiable and non-modifiable. Modifiable risk factors can be changed on your own. If a person smokes, he can quit smoking. Non-modifiable risk factors require our intervention, either medicinal or surgical.
D. Volyanskaya:
When do patients come in after surgery?
R. Abyshev:
When the patient has undergone surgery, stenting or bypass surgery has been performed, secondary prevention is necessary so that after surgical treatment there are no recurrent complications. There can be complications even during the operation - intraoperative complications, most often these are thrombosis, but I am not the one who deals with them, surgeons deal with them more.
D. Volyanskaya:
What is stenting?
R. Abyshev:
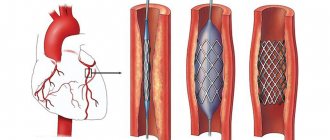
A stent is a metal mesh bent into a tube. This tube is installed inside the vessel. Its goal is to maintain the diameter of the vessel from the inside so that there is no spasm (narrowing of the internal lumen of the vessel), which leads to a limitation in the supply of oxygen to the blood flow upstream. The stent will maintain this diameter and allow you to constantly have normal blood flow.
In stenting, a stent—a metal mesh—is inserted into the vessel and supports it.
D. Volyanskaya:
What indications is this used for?
R. Abyshev:
Indications are constantly expanding; endovideosurgical treatment methods, which include stenting, have become quite widely used in practice. If previously the indication was only a single-vessel lesion or a lesion of no more than 3 vessels, now endovideo surgeons widely use stents. One of the comic cases: in Sweden there was a lawsuit against surgeons who installed 7 stents like a train, one after another. At this point, it would be enough to perform bypass surgery. The issues of expanding or narrowing the indications for stenting are constantly discussed, the rules are changing. Currently, the indication for stenting is one or two vessel lesions, when not all vessels are affected. It is advisable that the right coronary artery is not affected, because it is more difficult to place a stent in it. We are also talking about the rehabilitation period, because the rehabilitation period after bypass surgery, during which the chest is dissected at the level of the sternum, lasts up to 6 months. In the case of stenting, rehabilitation takes 2-3 weeks, the patient spends 5-7 days in the hospital and is discharged. Stenting is performed without general anesthesia, i.e. the patient is conscious. This operation can take from 15-20 minutes to an hour, depending on the complexity. Sometimes, unfortunately, there are times when a technically incorrectly performed operation leads to the patient being transferred to intensive care.
D. Volyanskaya:
Is it technically easy?
R. Abyshev:
Technically this is not difficult, everything depends on the hands of the one who performs it, this is the human factor. Therefore, you need to choose a person who does this every day, whose abilities are beyond doubt. The operation does not take much time, its prognosis is much better, its safety is better, so its choice is advantageous.
D. Volyanskaya:
When is a drug-eluting stent used?
R. Abyshev:
This is solely the choice of the operating doctor either or depending on the volume of purchases. If the stent is coated with a drug, there is a cytostatic agent inside, which prevents smooth muscle cells from growing inside the stent and forming a narrowing zone inside the stent. The stent has a longer shelf life and a greater guarantee that there will be no problems in this area. The average shelf life of a stent is 5-7 years.
D. Volyanskaya:
And then do I need to have another operation?
R. Abyshev:
No, not necessarily. This was precisely the main goal of my scientific work. For 13 years, I observed patients who underwent heart surgery. If the risk factors that brought the patient to the operating table were not corrected, this problem led to the minimization of the positive effect of the operation performed. Repeated stenoses and myocardial infarctions developed in the shortest possible time. Even if the patient has undergone surgery, he must take care of his health and correct risk factors. This is blood pressure, smoking, obesity, cholesterol - these must be dealt with, otherwise there will be a risk. If they manage to install a stent or have time to do a bypass, it will be luck. Therefore, technically, coronary heart disease, which was the reason for the initial hospitalization and heart surgery, continues to exist in the postoperative period. It needs to be dealt with. We were even able to identify the stages of development of this disease in the postoperative period. At the same time, we know for sure that adjustments to treatment and risk factors can lengthen the period before recurrent complications. If a patient does not care about his health, it is impossible to help him.
D. Volyanskaya:
What is bypass surgery?
R. Abyshev:
Bypass surgery is a more complex method of operation. He uses grafts. These are pieces of arteries or veins that are used as a bypass, creating a new blood flow. The narrowing zone is no longer touched; a new vessel is inserted upstream and downstream. Whether it is an artery or a vein does not matter. Grafts are taken exclusively from the patient. On the arm, on the leg, in the chest. They are sewn in and the blood flow is started naturally.
The operation is more complicated because it is used for more extended areas of narrowing, for more extensive atherosclerotic plaques, for more inconvenient localization of plaques. The operation takes longer, lasting an hour or two. Even two teams of surgeons can work: some isolate the vessels, others sew them in. These are angiosurgeons and cardiac surgeons. A more difficult question for anesthesiologists, because the operation is under anesthesia. Previously, these operations were also performed under artificial circulation, with cold cardioplegia, i.e., the heart was removed from the chest or was placed in an ice bed and covered with ice.
Bypass surgery creates a bypass for blood flow.
D. Volyanskaya:
It turns out that when bypassing a new channel is created?
R. Abyshev:
Imagine that you have a traffic jam on one road, and you build another road so that there is a parallel flow. The idea is to deliver oxygen and other nutrients upstream to the heart muscle. Because without this, upstream the tissue will simply die. This is the basis of myocardial infarction.
D. Volyanskaya:
In what cases should bypass surgery be performed?
R. Abyshev:
Of course, the choice is made exclusively by cardiac surgeons, but the main thing is extended areas of vascular narrowing, long, large plaques, very inconvenient localization along the lower wall, along the right coronary artery, which would be difficult for stenting. This is a method of treating coronary heart disease.
The rehabilitation period is more pronounced - up to 6 months.
D. Volyanskaya:
How long do people generally live after bypass surgery? Should this operation be performed on people over 75?
R. Abyshev:
There are currently no age restrictions. My experience of communicating with American surgeons has shown that they do not have an upper age limit for performing this type of operation. Here I have encountered bypass operations on patients aged 83 years. Previously there was a limit of 70-75 years.
Survival after surgery is quite good. Because the skills, hands, and equipment are good. Intraoperative complications are rare, although one of my patients died during bypass surgery last year. It is necessary to take into account risk factors as much as possible, the patient must be prepared for surgery. This is not done at random: the patient is stabilized in terms of blood pressure, the patient’s hemodynamic factor is stabilized, and only after that a fully prepared patient undergoes surgical treatment.
D. Volyanskaya:
Is the preparatory period for surgery long?
R. Abyshev:
If it's acute coronary syndrome, emergency hospitalization, it's literally calculated in hours, if not minutes. Bring the patient to the operating table as quickly as possible and perform the operation. Strategically, you can prepare it six months in advance.
D. Volyanskaya:
Is it true that they teach a special breathing technique?
R. Abyshev:
Breathing techniques are necessary after bypass surgery. Previously, when cold cardioplegia was used, it was necessary to prevent pneumonia by adequately opening the left lung. Therefore, in the past, patients were often given a glass of water and a straw, and asked to strain their lungs and breathe as intensely as possible, especially considering that the patient was in a supine position in the intensive care unit for the first period of time after the operation. A horizontal position is not the best option, because the peridiaphragmatic, lower part of the lungs is poorly ventilated, this can be the basis for pneumonia. The patient's stay in the hospital may be prolonged.
D. Volyanskaya:
I read that the most dangerous period is the postoperative period.
R. Abyshev:
Yes, sure. In general, mortality from heart attacks and strokes reaches 15-30%. The spread is very large. Russia ranks first in mortality from heart attacks and strokes in Europe. Our forecasts are not the best, and we have been holding this place tightly for the last 15-20 years.
D. Volyanskaya:
How often do you need to come for checkups after surgery? Do I need a special diet or a healthy lifestyle?
R. Abyshev:
This is situational, but once every six months is standard. My patients follow a healthy lifestyle because there is no other way. The main thing is to follow a strict diet and quit smoking. A low-carbohydrate or low-cholesterol diet is widely used in practice. Our task: to adjust cholesterol levels and keep sugar levels stable so that there are no problems with the blood lipid profile and sugar, which will be accompanied by an increase in blood pressure. A healthy lifestyle is one of the main elements, physical activity. If at first the patient is recommended to have a format of minor physical activity, especially after bypass surgery, then it expands to walking 5-7 thousand steps per day. Medicinal drugs play a major role. Lifestyle adjustments and smoking cessation give 30-50%, but in this situation you cannot do without medications.
After stenting and bypass surgery, you need to see a doctor every six months.
D. Volyanskaya:
How much does such an operation cost in total?
R. Abyshev:
From open sources and clinic prices, we can say that on average a stenting operation costs 100-200 thousand rubles per stent. The number of stents is determined by the surgeon during the coronary angiography procedure. Bypass surgery is more expensive, ranging from 300-500 thousand rubles.
D. Volyanskaya:
After such operations, does the risk of heart attack really decrease?
R. Abyshev:
It only decreases if we follow the recommendations. Your money was capitalized, you had an operation, if we are talking about government funding, about the compulsory medical insurance system, then no one cares about your future fate except you. The fate of a person is solely in his hands. For now, he has been given a second chance at life. Because he had an expensive operation.
D. Volyanskaya:
Does anything really change in the patients' minds? Is a person able to change his mind?
R. Abyshev:
Most of the men who are treated by me are brought by their wives. The factor of global consciousness is the wife, who understands that if there is no main breadwinner, the family’s well-being will not be at the same level. The second option is when the man himself understands. I’m talking about men because male gender is a risk factor in itself; this problem most often affects men. Sometimes a man himself understands that it’s time to take care of his health. These people approach the problem most adequately; they understand that it is advisable to invest money in their health and maintain this health, because their family is behind them; a team that works for people. They are purposeful, work as closely as possible with the cardiologist, and follow recommendations in detail. This is my patients' favorite population.
The third group is women. The woman listens to all the recommendations, but makes her own conclusions. She herself has logical explanations for what is happening to her health. Sometimes I manage to convince of the need to follow the recommendations, then I am happy because the patient follows all the recommendations. Having the excellent student syndrome, I achieve the result of a healthy person who came to me with a problem. Sometimes I injure myself because I worry about the patient, who must be responsible for himself. The most naughty person is a young woman. Because she apparently has a lot of worries in life. She puts emphasis, she will have time to live it a little later or another time.
D. Volyanskaya:
What can cause relapses?
R. Abyshev:
Differentiation of relapses by stenting and bypass surgery does not have clear statistics. When we talk about relapses, we are more likely to talk about death. The statistics are lame for a simple reason: in Russia there is no legislation that would require an autopsy in 100% of cases. We became very concerned about this issue after my American internship, because in America autopsies are done in 100% of cases. The cause of death is reliably known. We don’t have such practice, so we don’t know why the person died.
If a patient died after undergoing surgery, this indicates one thing: he did not follow the recommendations or was treated incorrectly. Rehabilitation must be accompanied by serious psychological work. A psychologist is a mandatory element to be included in the patient rehabilitation group. Often you don’t have to visit a psychologist, the doctor himself can be a psychologist, you need to find a language, you need to reach the person’s consciousness, find out the problem that worries him. When we talk about a person who has suffered a heart attack or stroke, we can imagine a cruiser that was hit, had a hole that seriously threatened his life, the person realized this, and fears appear in his life. How likely is it for this to happen to me again? Will I survive? How long will I live? The fear that a person may suddenly die is seriously stressful. Most often this is accompanied by depression. Over the past 5 years, the active introduction of antidepressants into the treatment regimen for patients with cardiac pathology and those who have undergone bypass surgery and stenting has been discussed. The introduction of a psychologist is necessary for one simple reason: stress and depression do not allow a person to achieve a positive background in terms of psychology. Negative emotion is destructive, it destroys a person from the inside, he may even lose meaning in life.
D. Volyanskaya:
Are people who have had bypass surgery disabled?
R. Abyshev:
Technically yes. The degree of disability is determined, but later it is removed. Taking into account the fact that the rehabilitation period leads to normalization of the functioning of the entire system. A person normally, as is theoretically assumed, should return to his activities.
D. Volyanskaya:
What difficulties did you have to face? What is the most difficult case in your practice?
R. Abyshev:
The most difficult case. It is unlikely that this patient is listening to me now, but this patient has a unique ability to ignore risk factors and my attempts to reach his consciousness. It turns out like this: “Doctor, you help me, but I won’t do anything myself.” I have a problem communicating with a patient who doesn’t want to do anything himself.
D. Volyanskaya:
Every patient believes that he is a doctor.
R. Abyshev:
Agree. I spend a lot of time trying to refute what people read on the Internet. In this situation, the patient thinks that there are smarter people, and there is no way to refute everything that is written on the Internet. This is simply impossible. I don’t know who is leaking so much information there. The most difficult thing is to pull yourself together and correct the risk factors.
D. Volyanskaya:
Tell me why you decided to become a doctor?
R. Abyshev:
I come from a clan family with a lot of people who have worked in healthcare. And I told my grandmother my profession when I was a 4-year-old child: I want to be a cardiologist. I have two sisters, both have medical degrees; my father is a famous person, about whom there is even a page on Wikipedia (which I am proud of and can only strive for), he also has a medical and chemical education, he develops medicines; My mother is a pharmacist.
I had a unique school where teachers from institutes taught. In May of the 11th grade I entered the faculty of FAVT at LETI, the faculty of management and work with electronics, which has nothing to do with medicine. But in June-July, having passed the medical exams, I entered medical school and settled on the medical direction.
D. Volyanskaya:
Rashad, I would like to thank you for coming from St. Petersburg and finding this opportunity. Thank you very much for the conversation. A good doctor is the one you talk to, and it becomes easier. Even my angina went away.
Dear friends, we remind you that today our guest was Rashad Abyshev, candidate of medical sciences, cardiologist, chief physician of the St. Petersburg Mentor-Clinic. Today we talked about bypass surgery, stenting, relapses, complications. Thank you very much.
R. Abyshev:
Thank you.
D. Volyanskaya:
It was the “Media Doctor” channel, the “Online Reception” program, which was hosted for you by me, Daria Volyanskaya, and my wonderful co-host Yulia Titova. Until we meet again, take care of yourself, don’t read nonsense on the Internet, go to the doctors regularly for examinations. Until next time.
Lifestyle after coronary artery stenting surgery
The article was published in the new issue of the journal of the Center for High Medical Technologies.
Read the entire issue
Stenting is a minimally invasive surgical intervention in which a stent is implanted into a patient’s coronary vessel narrowed by atherosclerotic plaques. A stent is a metal spiral made of cellular material, which expands in the lumen of the vessel, “presses” plaques into its wall and keeps its lumen free.
Installation of a stent leads to the fact that coronary blood circulation improves, the heart begins to receive more oxygen, and during physical activity the person does not experience myocardial ischemia. This eliminates angina attacks and improves a person’s well-being.
The apparent simplicity of stenting, the absence of the need for long recovery after it, as well as the noticeable therapeutic effect of the operation often create in patients the illusion of a complete recovery. However, stenting is aimed only at eliminating the symptoms of the disease. The cause of coronary heart disease - atherosclerosis - continues to exist and progress, creating a threat of recurrence of angina pectoris, the development of myocardial infarction, heart failure and other very serious problems. For this reason, a person who has undergone surgery must be fully aware of all the possible dangers of his situation and the need for further treatment.
After stenting
Unfortunately, the volume of drug therapy after stenting surgery will not decrease. The patient must understand that it is impossible to refuse medications for ischemic heart disease. After successful stenting of the coronary arteries, the drug therapy regimen is of great importance, in which dual antiplatelet therapy plays a decisive role (reducing the risk of stent thrombosis). Follow the treatment regimen and do not forget: your good health after surgery is largely maintained due to the fact that you follow the prescribed therapy regimen.
1) Physical activity is one of the most important lifestyle conditions after stenting. Regular exercise slows down the development of atherosclerosis, trains the heart muscle, helps stabilize blood pressure, and has a general health effect on the body. A patient who has undergone this operation should be prepared for the fact that from now on he must engage in physical activity at least 4-5 times a week. Among specific types of loads, special physical therapy exercises, walking, cycling, swimming, and jogging are recommended. Sports that require significant physical effort and potentially cause injury (weight lifting, boxing) are not recommended.
2) Nutrition after stenting
The second extremely important component of therapy is diet. It’s sad, but not all patients adhere to the recommended nutritional rules. And we can say without a doubt that this plays a big role in the high incidence of recurrent angina and repeated stenting. Diet therapy after stenting of coronary vessels should be based on the following principles:
Limiting animal fats, refined carbohydrates, sweets, and limiting salt in the diet. Limiting the consumption of coffee and other drinks and products containing caffeine (strong tea, chocolate, cocoa). Caffeine causes vasospasm and increased heart function, which creates increased stress on the cardiovascular system and harms patients with coronary artery disease and stenting. Adding vegetable oils, fresh vegetables and fruits, fish to the diet (consume at least 2 times a week). All this prevents the development of atherosclerosis. It is also worth giving up bad habits.
3) Performance after stenting. After the stenting operation, the patient will be able to return to normal work. The specific time frame for restoration of working capacity may vary; it depends on the person’s condition (the severity of coronary artery disease, the presence of a recent heart attack, etc.) and his profession. Intellectual workers can start working almost immediately after stenting, and those whose specialty is related to physical activity are allowed to start working later.
The stenting operation eliminates the symptoms of coronary artery disease, the person’s condition improves after it, therefore, it is quite rare to talk about registering disability for patients who have undergone it.
4) Travel and rest after stenting. When a person’s condition stabilizes after surgery, he is allowed to travel by any means and without restrictions.
How is stenting different from coronary artery bypass grafting?
Stenting is a minimally invasive method for treating coronary heart disease. It is fundamentally different from bypass surgery in that it causes minimal trauma to the patient and has a short rehabilitation period.
A stent is an implant in the form of a frame that is installed in a vessel. It usually consists of a metal base on which a special polymer containing a medicinal substance is applied. The stent itself is mounted on a balloon catheter, which is necessary to deliver this frame to the affected area of the artery. Drug coating on the stent is necessary to ensure that it works as long as possible, so that restenosis, or repeated narrowing of the vessel after implantation, does not occur. Medicines that are applied to the stent prevent the growth of the so-called inner lining of the capillary, thereby preventing this segment of the artery from narrowing.
Stenting belongs to the category of high-tech operations.