Cardiac output is a concept used in medicine that refers to the amount of blood ejected by the heart in one minute. Technically, it is calculated as the product of heart rate and stroke volume.
An increase in heart rate is a compensatory mechanism for increasing oxygen supply to tissues.
Factors that influence systolic volume are the volume of blood pushed by the heart into the aorta during the contraction period, preload, afterload, and contractile function.
Today, there are a number of techniques that allow us to obtain cardiac output measurements in a very efficient and non-invasive way. The Fick technique, which was used previously, has been replaced by more modern methods.
Pulse wave analysis resulted in a continuous and minimally invasive measurement of cardiac output. Other techniques, such as bioremediation, Doppler or echocardiography, allow us to obtain cardiac output measurements in a non-invasive, rapid and reliable manner.
Strengthening the heart muscle
Digitalis is one of the oldest drugs still used, mainly as a derivative known as digoxin (Lanoxin). The muscles of the ventricles contract to remove blood from the heart. Digoxin increases the strength and speed of this contraction. It may also help control abnormal heart rhythms that reduce EF. Other drugs similarly increase the pumping effect, such as milrinone (Primacor) and dobutamine (Dobutrex). These drugs are not generally recommended for heart failure and are reserved for the closely monitored treatment of acute heart failure that is refractory to other treatments.
Patient with low left ventricular ejection fraction
November 11, 2017 0
Introduction. Treatment of chronic heart failure (CHF) is one of the most socially significant problems in our country. According to epidemiological studies in Russia, there are more than 8 million people with symptoms of CHF. Decompensation of CHF causes hospitalization in hospitals, increasing cardiovascular mortality and disabling the working-age population. This clinical example shows the possibilities of modern methods of interventional treatment of CHF.
Description of the case. Patient I., 59 years old, was hospitalized with complaints of rapid irregular heartbeat, compressive pain and shortness of breath with minimal physical activity, swelling of the lower extremities, weakness, and decreased performance. At the age of 50, atrial fibrillation was diagnosed, and no attempts were made to restore sinus rhythm. On an outpatient basis he took cardiac glycosides, beta-blockers, and ACE inhibitors.
He was sent to the Federal Center for Agriculture (Astrakhan) to determine further tactics. According to ECHO-CS, dilatation of the left ventricle (LV) and left atrium (LA) was revealed: LA – 52 mm, LV EDV 297 ml, LV ESV 178 ml, LVEF 23%, diffuse LV hypokinesis, mitral regurgitation of the 2nd degree. The ECG shows AF, tachysystolic form with an average heart rate of 120 per minute. LBBB (QRS 158 ms).
Taking into account the pain syndrome, as well as to exclude the ischemic genesis of AF, a coronary angiography was performed: no coronary pathology was detected. Drug therapy was adjusted: rhythm-slowing therapy was intensified, diuretics and oral anticoagulants were added.
At a follow-up visit to the clinic after 3 months, against the background of recommended therapy, ECHO CS showed positive dynamics: LV EDV - 288 ml; LV ESV - 188 ml; LVEF - 35%, mitral regurgitation 2-2.5 degrees.
Considering the low LVEF and the presence of LBBB on the background of optimal drug therapy for three months, for the primary prevention of sudden cardiac death and treatment of CHF, implantation of a CRT with a cardioverter-defibrillator function was performed. The operation was uneventful; the left ventricular electrode was implanted into the lateral vein of the heart. After implantation, the patient was connected to a remote monitoring system, allowing him to remotely receive messages from the implanted device according to a programmed transmission schedule.
After 3 months, the device was tested - no malfunctions were detected, the percentage of biventricular stimulation (BVS) was 74%. Unmotivated shocks were delivered twice due to incorrect discrimination of AF with tachysystolic conduction to the ventricles. Subjectively, he notes an improvement in health (shortness of breath has decreased, swelling of the lower extremities has disappeared). On ECHO-CS, LV EDV is 208 ml; LV ESV - 123 ml; LVEF - 41%, mitral regurgitation grade 2.
Considering the need for 100% BVS, the occurrence of unmotivated shocks, and the tachysystolic form of AF, resistant to drug therapy, RFA of the AV junction was performed.
At discharge on the 4th day, during ECHO-CS, an increase in LVEF up to 50% and a decrease in LV size were noted - LV EDV - 203 ml, LV ESV - 101 ml.
Discussion. 15% of all patients with CHF have signs of electrical dyssynchrony (QRS complex duration more than 120 ms), which can be corrected by implantation of a cardiac resynchronization device. One of the important conditions for effective CRT is the presence of sinus rhythm in a patient with CHF and LBBB. The tactics of managing patients with CRT and atrial fibrillation (AF) in some cases is ambiguous and requires an individual assessment with the participation of a team of specialists (cardiologist, cardiac surgeon, electrophysiologist, functional diagnostics doctor).
To fully realize the effects of SRT, a BVS close to 100% is required. When the percentage of BVS decreases, regardless of the clinical effects of CRT, the cause of this condition should be verified. For drug-resistant types of often recurrent, persistent or permanent arrhythmias, in case of ineffective RFA of arrhythmia, the strategy of choice, which increases BVS to 100%, is the creation of artificial atrioventricular block.
Conclusion on use in clinical practice. Practicing physicians are often poorly informed about the possibilities of interventional treatment of CHF, and RFA of the AV junction is considered by many as a mutilating, unjustified procedure. This clinical case illustrates the high effectiveness of the interventional approach in cardiology, which, in combination with optimal drug therapy, can demonstrate significant clinical effects.
Relevance of the problem
Over the past 20 years, the incidence of heart failure among Europeans has been decreasing. But the number of cases in the middle and older groups of the population is increasing due to increasing life expectancy.
According to European studies (ECHOCG), a decrease in ejection fraction was found in half of patients with symptomatic heart failure and in half of asymptomatic patients.
Patients with heart failure are less able to work, their quality of life and its duration are reduced.
Treatment of these patients is the most expensive for both them and the state. Therefore, the search for ways to prevent the occurrence, early diagnosis and effective treatment of heart disease remains relevant.
Studies conducted in recent decades have proven the effectiveness of a number of groups of drugs to improve the prognosis and reduce mortality in patients with low cardiac fraction:
- adenosine-converting enzyme inhibitors (Enalapril);
- angiotensin P antagonists (Valsartan);
- beta blockers (“Carvedilol”);
- aldosterone blockers (“Spironolactone”);
- diuretics (“Torasemide”);
- "Digoxin".
Publications in the media
Chronic systolic heart failure is a clinical syndrome that complicates the course of a number of diseases and is characterized by the presence of shortness of breath during exercise (and then at rest), fatigue, peripheral edema and objective signs of impaired cardiac function at rest (for example, auscultatory signs, echocardiographic data) . Statistical data. Chronic systolic heart failure occurs in 0.4–2% of the population. Its prevalence increases with age: in people over 75 years of age it develops in 10% of cases.
Etiology • Heart failure with low cardiac output •• Myocardial damage: ••• IHD (post-infarction cardiosclerosis, chronic myocardial ischemia) ••• Cardiomyopathies ••• Myocarditis ••• Toxic effects (for example, alcohol, doxorubicin) ••• Infiltrative diseases (sarcoidosis, amyloidosis) ••• Endocrine diseases ••• Nutritional disorders (vitamin B1 deficiency) •• Myocardial overload ••• Arterial hypertension ••• Rheumatic heart defects ••• Congenital heart defects (for example, aortic stenosis) •• Arrhythmias ••• Supraventricular and ventricular tachycardias ••• Atrial fibrillation • Heart failure with high cardiac output •• Anemia •• Sepsis •• Arteriovenous fistula.
Risk factors • Refusal of the patient from pharmacotherapy • Prescription of drugs with a negative inotropic effect, and their uncontrolled use • Thyrotoxicosis, pregnancy and other conditions associated with increased metabolic needs • Excess body weight • Presence of chronic pathology of the heart and blood vessels (arterial hypertension, coronary artery disease, defects hearts, etc.).
Pathogenesis • The pumping function of the heart is impaired, which leads to a decrease in cardiac output • As a result of a decrease in cardiac output, hypoperfusion of many organs and tissues occurs •• A decrease in cardiac perfusion leads to activation of the sympathetic nervous system and an increase in heart rate •• A decrease in renal perfusion causes stimulation of the renin-angiotensin systems. The production of renin increases, while excessive production of angiotensin II occurs, leading to vasoconstriction, water retention (edema, thirst, increased blood volume) and a subsequent increase in preload on the heart •• A decrease in the perfusion of peripheral muscles causes the accumulation of under-oxidized metabolic products in them, as well as hypoxia leads to severe fatigue.
CLASSIFICATIONS Classification of the XII All-Union Congress of Therapists in 1935 ( N.D. Strazhesko, V.Kh. Vasilenko). • Stage I (initial) - latent heart failure, manifested only during physical activity (shortness of breath, tachycardia, fatigue). • Stage II (severe) - prolonged circulatory failure, hemodynamic disturbances (stagnation in the systemic and pulmonary circulation), dysfunction of organs and metabolism are also expressed at rest •• Period A - the beginning of a long stage, characterized by mild hemodynamic disturbances, dysfunction hearts or only parts of them •• Period B - the end of a long stage, characterized by profound hemodynamic disturbances, the entire cardiovascular system is involved in the process. • Stage III (final, dystrophic) - severe hemodynamic disorders, persistent changes in metabolism and functions of all organs, irreversible changes in the structure of tissues and organs.
New York Heart Association classification (1964) • Class I - ordinary physical activity does not cause significant fatigue, shortness of breath or palpitations • Class II - mild limitation of physical activity: satisfactory health at rest, but ordinary physical activity causes fatigue, palpitations, shortness of breath or pain • Class III - severe limitation of physical activity: satisfactory health at rest, but less than usual load leads to the appearance of symptoms • Class IV - inability to perform any physical activity without deteriorating well-being: symptoms of heart failure are present even at rest and intensify with any physical activity .
The classification of the Society of Heart Failure Specialists (OSSN, 2002) was adopted at the All-Russian Congress of Cardiologists in October 2002. The convenience of this classification is that it not only reflects the state of the process, but also its dynamics. The diagnosis must reflect both the stage of chronic heart failure and its functional class. It is necessary to take into account that the correspondence between the stage and the functional class is not entirely clear - the functional class is set in the presence of slightly less pronounced manifestations than is necessary to assign the corresponding stage of heart failure.
• Stages of chronic heart failure (may worsen despite treatment) •• Stage I - the initial stage of heart disease (damage). Hemodynamics are not impaired. Latent heart failure Asymptomatic left ventricular dysfunction •• Stage IIA - clinically pronounced stage of heart disease (damage). Hemodynamic disturbances in one of the blood circulation circles, expressed moderately. Adaptive remodeling of the heart and blood vessels •• Stage IIB - severe stage of heart disease (damage). Pronounced changes in hemodynamics in both circles of blood circulation. Maladaptive remodeling of the heart and blood vessels •• Stage III - the final stage of cardiac damage. Pronounced changes in hemodynamics and severe (irreversible) structural changes in target organs (heart, lungs, blood vessels, brain, kidneys). The final stage of organ remodeling.
• Functional classes of chronic heart failure (can change during treatment in either direction) •• FC I - there are no restrictions on physical activity: habitual physical activity is not accompanied by rapid fatigue, shortness of breath or palpitations. The patient can tolerate increased workload, but it may be accompanied by shortness of breath and/or delayed recovery •• FC II - slight limitation of physical activity: there are no symptoms at rest, habitual physical activity is accompanied by fatigue, shortness of breath or palpitations •• FC III - noticeable limitation of physical activity: at rest there are no symptoms, physical activity of lesser intensity compared to usual exercise is accompanied by the appearance of symptoms •• FC IV - inability to perform any physical activity without discomfort; Symptoms of heart failure are present at rest and worsen with minimal physical activity.
Clinical manifestations • Complaints - shortness of breath, attacks of suffocation, weakness, fatigue • • Shortness of breath in the initial stage of heart failure occurs during physical activity, and in case of severe heart failure - at rest. It appears as a result of increased pressure in the pulmonary capillaries and veins. This reduces the extensibility of the lungs and increases the work of the respiratory muscles. •• Severe heart failure is characterized by orthopnea - a forced sitting position taken by the patient to facilitate breathing with severe shortness of breath. The deterioration of health in the supine position is due to the deposition of fluid in the pulmonary capillaries, leading to an increase in hydrostatic pressure. In addition, in the lying position, the diaphragm rises, which makes breathing somewhat difficult. • Chronic heart failure is characterized by paroxysmal nocturnal shortness of breath (cardiac asthma), caused by the occurrence of interstitial pulmonary edema. At night, during sleep, an attack of severe shortness of breath develops, accompanied by coughing and the appearance of wheezing in the lungs. As heart failure progresses, alveolar pulmonary edema may occur •• Rapid fatigue in patients with heart failure appears due to insufficient oxygen supply to skeletal muscles •• Patients with chronic heart failure may experience nausea, loss of appetite, abdominal pain, abdominal enlargement (ascites) due to blood stagnation in the liver and portal vein system •• From the side of the heart, pathological III and IV heart sounds can be heard. Moist rales are detected in the lungs. Hydrothorax is characteristic, often right-sided, resulting from an increase in pleural capillary pressure and extravasation of fluid into the pleural cavity.
• Clinical manifestations of heart failure significantly depend on its stage •• Stage I - signs (fatigue, shortness of breath and palpitations) appear during normal physical activity, there are no manifestations of heart failure at rest •• Stage IIA - there are unexpressed hemodynamic disturbances. Clinical manifestations depend on which parts of the heart are predominantly affected (right or left) ••• Left ventricular failure is characterized by stagnation in the pulmonary circulation, manifested by typical inspiratory shortness of breath with moderate physical exertion, attacks of paroxysmal nocturnal shortness of breath, and rapid fatigue. Swelling and enlargement of the liver are uncharacteristic. ••• Right ventricular failure is characterized by the formation of congestion in the systemic circulation. Patients are concerned about pain and heaviness in the right hypochondrium, decreased diuresis. The liver is characterized by enlargement (the surface is smooth, the edge is rounded, palpation is painful). A distinctive feature of stage IIA heart failure is considered to be complete compensation of the condition during treatment, i.e. reversibility of manifestations of heart failure as a result of adequate treatment •• Stage IIB - there are profound hemodynamic disturbances, the entire circulatory system is involved in the process. Shortness of breath occurs with the slightest physical exertion. Patients are concerned about a feeling of heaviness in the right hypochondrium, general weakness, and sleep disturbances. Orthopnea, edema, ascites are characteristic (a consequence of increased pressure in the hepatic veins and peritoneal veins - transudation occurs, and fluid accumulates in the abdominal cavity), hydrothorax, hydropericardium •• Stage III - the final dystrophic stage with profound irreversible metabolic disorders. As a rule, the condition of patients at this stage is severe. Shortness of breath is pronounced even at rest. Characterized by massive edema, accumulation of fluid in the cavities (ascites, hydrothorax, hydropericardium, edema of the genital organs). At this stage, cachexia occurs.
Instrumental data • ECG : you can identify signs of blockade of the left or right branch of the His bundle, ventricular or atrial hypertrophy, pathological Q waves (as a sign of a previous MI), arrhythmias. A normal ECG casts doubt on the diagnosis of chronic heart failure. • EchoCG allows you to clarify the etiology of chronic heart failure and assess the functions of the heart, the degree of their impairment (in particular, determine the ejection fraction of the left ventricle). Typical manifestations of heart failure are expansion of the cavity of the left ventricle (as it progresses, expansion of other chambers of the heart), an increase in the end-systolic and end-diastolic dimensions of the left ventricle, and a decrease in its ejection fraction. • X-ray examination •• It is possible to detect venous hypertension in the form of redistribution of blood flow in favor of the upper parts of the lungs and an increase in the diameter of blood vessels •• With congestion in the lungs, signs of interstitial edema are detected (Kerley lines in the costophrenic sinuses) or signs of pulmonary edema •• Hydrothorax is detected ( most often right-sided) •• Cardiomegaly is diagnosed when the transverse size of the heart increases by more than 15.5 cm in men and more than 14.5 cm in women (or when the cardiothoracic index is more than 50%). • Catheterization of the cardiac cavities reveals an increase in pulmonary capillary wedge pressure of more than 18 mm Hg. Diagnostic criteria - Framingham criteria for the diagnosis of chronic heart failure, divided into major and minor • Major criteria: paroxysmal nocturnal dyspnea (cardiac asthma) or orthopnea, distention of the jugular veins, wheezing in the lungs, cardiomegaly, pulmonary edema, pathological III heart sound, increased central venous pressure ( more than 160 mm water column), blood flow time more than 25 s, positive “hepatojugular reflux” • Minor criteria: swelling in the legs, night cough, shortness of breath on exertion, liver enlargement, hydrothorax, tachycardia more than 120 per minute, decrease in vital capacity by 1 /3 of the maximum • To confirm the diagnosis of chronic heart failure, either 1 major or 2 minor criteria are required. The symptoms detected must be related to heart disease.
Differential diagnosis • Nephrotic syndrome - a history of edema, proteinuria, renal pathology • Liver cirrhosis • Occlusive lesions of the veins with subsequent development of peripheral edema. Treatment • It is necessary to first evaluate the possibility of influencing the cause of the deficiency. In some cases, effective etiological intervention (for example, surgical correction of heart disease, myocardial revascularization in ischemic heart disease) can significantly reduce the severity of manifestations of chronic heart failure • In the treatment of chronic heart failure, non-drug and drug therapy methods are distinguished. It should be noted that both types of treatment should complement each other.
Non-drug treatment • Limiting the consumption of table salt to 5–6 g/day, liquid (up to 1–1.5 l/day) • Optimizing physical activity •• Moderate physical activity is possible and even necessary (walking for at least 20–30 minutes 3 –5 r/week) •• Complete physical rest should be observed if the condition worsens (at rest the heart rate decreases and the work of the heart decreases).
Drug therapy . The ultimate goal of treatment of chronic heart failure is to improve the quality of life and increase its duration.
• Diuretics. When prescribing them, it is necessary to take into account that the occurrence of edema in heart failure is associated with several reasons (constriction of the renal vessels, increased secretion of aldosterone, increased venous pressure. Treatment with diuretics alone is considered insufficient. In chronic heart failure, loop (furosemide) or thiazide (for example, hydrochlorothiazide) diuretics. If the diuretic response is insufficient, loop diuretics and thiazides are combined •• Thiazide diuretics. Hydrochlorothiazide is usually used in a dose of 25 to 100 mg/day. It should be remembered that if the renal GFR is less than 30 ml/min, it is not advisable to use thiazides •• Loop diuretics begin to act faster, their diuretic effect is more pronounced, but less durable than that of thiazide diuretics. Furosemide is used at a dose of 20–200 mg/day IV, depending on the manifestations of edema and diuresis. It can be prescribed orally at a dose of 40– 100 mg/day.
• ACE inhibitors cause hemodynamic unloading of the myocardium due to vasodilation, increased diuresis, and decreased filling pressure of the left and right ventricles. Indications for prescribing ACE inhibitors are clinical signs of heart failure, a decrease in left ventricular ejection fraction of less than 40%. When prescribing ACE inhibitors, certain conditions must be observed according to the recommendations of the European Society of Cardiology (2001) •• It is necessary to stop taking diuretics 24 hours before taking ACE inhibitors •• Blood pressure should be monitored before and after taking ACE inhibitors •• Treatment begins with small doses with gradual their increase •• It is necessary to monitor renal function (diuresis, relative density of urine) and the concentration of blood electrolytes (potassium, sodium ions) while increasing the dose every 3–5 days, then every 3 and 6 months •• Avoid co-administration of potassium-sparing diuretics (their can be prescribed only for hypokalemia) •• Concomitant use of NSAIDs should be avoided.
• The first positive data have been obtained on the beneficial effect of angiotensin II receptor blockers (in particular, losartan) on the course of chronic heart failure as an alternative to ACE inhibitors in cases of intolerance or contraindications to their use.
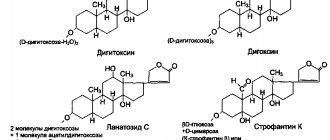
• Cardiac glycosides have a positive inotropic (increase and shorten systole), negative chronotropic (decreasing heart rate), negative dromotropic (slowing AV conduction) effect. The optimal maintenance dose of digoxin is considered to be 0.25–0.375 mg/day (in elderly patients 0.125–0.25 mg/day); The therapeutic concentration of digoxin in blood serum is 0.5–1.5 mg/l. Indications for the use of cardiac glycosides are tachysystolic atrial fibrillation and sinus tachycardia.
• b-blockers •• The mechanism of beneficial action of β-blockers in chronic heart failure is due to the following factors ••• Direct protection of the myocardium from the adverse effects of catecholamines ••• Protection against catecholamine-induced hypokalemia ••• Improvement of blood flow in the coronary arteries due to a decrease in heart rate and improvement diastolic relaxation of the myocardium ••• Reducing the effect of vasoconstrictor systems (for example, due to decreased renin secretion) ••• Potentiation of the vasodilating kallikrein-kinin system ••• Increasing the contribution of the left atrium to the filling of the left ventricle due to improved relaxation of the latter •• Currently from b -adrenergic blockers for the treatment of chronic heart failure, carvedilol is recommended for use - a b1- and a1-blocker with vasodilating properties. The initial dose of carvedilol is 3.125 mg 2 times / day, followed by an increase in the dose to 6.25 mg, 12.5 mg or 25 mg 2 times / day in the absence of side effects in the form of arterial hypotension, bradycardia, decreased left ventricular ejection fraction (according to EchoCG) and other negative manifestations of the action of b-blockers. Metoprolol is also recommended, starting with a dose of 12.5 mg 2 times / day, bisoprolol 1.25 mg 1 time / day under the control of ventricular ejection fractions with a gradual increase in dose after 1-2 weeks.
• Spironolactone. It has been established that the administration of the aldosterone antagonist spironolactone at a dose of 25 mg 1–2 times a day (in the absence of contraindications) helps to increase the life expectancy of patients with heart failure. • Peripheral vasodilators are prescribed for chronic heart failure if there are contraindications or if ACE inhibitors are poorly tolerated. Of the peripheral vasodilators, hydralazine is used at a dose of up to 300 mg/day, isosorbide dinitrate at a dose of up to 160 mg/day.
• Other cardiotonic drugs . β-Adrenergic agonists (dobutamine), phosphodiesterase inhibitors are usually prescribed for 1–2 weeks in the final stage of heart failure or in case of a sharp deterioration in the patient’s condition.
• Anticoagulants. Patients with chronic heart failure are at high risk of thromboembolic complications. Both pulmonary embolism due to venous thrombosis and thromboembolism of vessels in the systemic circulation caused by intracardiac thrombi or atrial fibrillation are possible. The administration of indirect anticoagulants to patients with chronic heart failure is recommended in the presence of atrial fibrillation and a history of thrombosis.
• Antiarrhythmic drugs. If there are indications for the prescription of antiarrhythmic drugs (atrial fibrillation, ventricular tachycardia), it is recommended to use amiodarone at a dose of 100–200 mg/day. This drug has minimal negative inotropic effects, whereas most other drugs in this class reduce left ventricular ejection fraction. In addition, antiarrhythmic drugs themselves can provoke arrhythmias (proarrhythmic effect). Surgery
• The choice of the optimal method of surgical treatment depends on the cause leading to heart failure. Thus, in case of ischemic heart disease, in many cases, myocardial revascularization is feasible; in case of idiopathic subaortic hypertrophic stenosis, septal myectomy; in case of valvular defects, prosthetics or reconstructive interventions on the valves; in case of bradyarrhythmias, pacemaker implantation, etc.
• In case of heart failure refractory to adequate therapy, the main surgical treatment is heart transplantation. • Methods of mechanical circulatory support (implantation of assisters, artificial ventricles and biomechanical pumps), previously proposed as temporary options before transplantation, have now acquired the status of independent interventions, the results of which are comparable to the results of transplantation. • To prevent the progression of cardiac dilatation, devices are implanted in the form of a mesh that prevents excessive expansion of the heart. • In case of cor pulmonale that is tolerant to treatment, transplantation of the heart-lung complex seems to be a more appropriate intervention.
Forecast. Overall, the 3-year survival rate of patients with chronic systolic heart failure is 50%. The mortality rate from chronic systolic heart failure is 19% per year.
• Factors, the presence of which correlates with a poor prognosis in patients with heart failure •• Decrease in left ventricular ejection fraction of less than 25% •• Inability to climb one floor and move at a normal pace for more than 3 minutes •• Decrease in the content of sodium ions in blood plasma less than 133 mEq /l •• Decrease in the concentration of potassium ions in the blood plasma less than 3 meq/l •• Increase in the content of norepinephrine in the blood •• Frequent ventricular extrasystole during daily ECG monitoring.
• The risk of sudden cardiac death in patients with heart failure is 5 times higher than in the general population. Most patients with chronic heart failure die suddenly, mainly from ventricular fibrillation. Prophylactic administration of antiarrhythmic drugs does not prevent this complication.
ICD-10 • I50 Heart failure
Reduced vascular resistance of a blood vessel
Arteries also have muscles. The more they contract, the smaller the channel through which blood flows, and the greater the tension on the heart muscle. Angiotensin, a naturally occurring hormone, is a very powerful blood vessel constrictor. Drugs that inhibit the formation of angiotensin or block its ability to bind to a blood vessel help relax the vascular muscles and are the basis of the Heart Failure Society of America Guidelines. Examples include captopril (Capoten), enalapril (Vasotec), valsartan (Diovan), and losartan (Cozaar). Because of this relaxation, the heart can pump out more blood per beat, improving EF. The drug combination hydralazine and isosorbide (Bidil) may be effective in patients who are resistant to—or intolerant to—angiotensin inhibitors.
Relaxation of the heart muscle
In response to decreased EF, the body releases substances such as adrenaline, which increase the speed and force of ventricular contraction. While temporary effective, chronic elevations of these compounds cause the heart muscle to strengthen and reduce its movement. Beta blockers are drugs that counteract these actions, reducing tension in the heart wall and improving the ability to contract. Three of these are recommended: carvedilol (Coreg), metoprolol succinate (Toprol XL), and bisoprolol (Zebeta). Beta blockers are most often used in combination with angiotensin inhibitors.
Artificial heart valves
Recommendations for patients with a prosthetic heart valve 1.6 MB
Artificial heart valve: 2 main types
If any of the 4 heart valves malfunction - they are narrowed (stenosis) or excessively dilated (insufficiency) - it is possible to replace them or reconstruct them using artificial analogues. An artificial heart valve is a prosthesis that provides the required direction of blood flow by intermittently closing the mouths of venous and arterial vessels. The main indication for prosthetics is gross changes in the valve leaflets, leading to severe circulatory disorders.
There are two main types of artificial heart valves: mechanical and biological models, each of which has its own characteristics, advantages and disadvantages.
1. Butchart EG et al. Recommendations for the management of patients after heart valve surgery. European Heart Journal. 2005: 26(22); 2465-2471.
Figure 1. Two main types of artificial valves
Mechanical heart valve or biological prosthesis?
The mechanical heart valve is reliable, lasts a long time and does not need to be replaced, but requires constant use of special medications that reduce blood clotting.
2. Bonow RO, Carabello BA, Kanu C. et al.; American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease) : developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation 2006; 114(5):e84-231; J Am Coll Cardiol 2006; 48(3):e1-148.
Biological valves may gradually deteriorate. Their service life largely depends on the age of the patient and concomitant diseases. With age, the process of destruction of biological valves slows down significantly.
The decision about which valve is most optimal should be made before surgery during a mandatory conversation between the surgeon and the patient.
Life with an artificial heart valve
People with prosthetic heart valves are at very high risk of thromboembolic complications. The fight against thrombosis is the basis of the management strategy for such patients, and it is its success that largely determines the prognosis for the patient.
The risk of thromboembolic complications is reduced with the use of biological valve prostheses, but they have their disadvantages. They are implanted infrequently and mainly in older people.
Living with an artificial heart valve requires a number of restrictions. The majority of patients with prosthetic valves are those with mechanical prostheses, who belong to a group at high risk of developing thrombotic complications. The patient is forced to constantly take antithrombotic drugs, in the vast majority of cases - indirect anticoagulants (warfarin). Almost all patients with mechanical heart valves should take them. The choice of a bioprosthesis also does not exclude the need to take warfarin, especially in patients with atrial fibrillation. To avoid dangerous bleeding, patients chronically taking warfarin should avoid daily activities and entertainment associated with an increased risk of injury (contact sports, working with cutting objects, or a high risk of falls, even from height).
The most important aspects of medical monitoring of a patient with an artificial heart valve today include:
- blood clotting control;
- active prevention of thromboembolic complications using anticoagulants (most often warfarin).
3. Bonow RO, Carabello BA, Chatterjee K. et al.; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2008;118(15):e523-661; J Am Coll Cardiol 2008; 52(13):e1-142.
It is important to note that European and American experts now consider the levels of antithrombotic therapy previously recommended for most patients to be too intense. Modern approaches to risk assessment make it possible to identify subgroups of people with the highest risk of thromboembolic complications and active antithrombotic therapy. For other patients with prosthetic heart valves, less aggressive antithrombotic therapy may be more effective.
Prevention of thrombosis in patients with mechanical heart valves
Prevention of thrombosis in patients with a mechanical heart valve requires lifelong antithrombotic therapy.
The intensity of warfarin therapy depends on the location of the prosthesis and its type. For example, in accordance with the ACC/AHA (2008) recommendations, a mechanical aortic valve prosthesis requires maintaining an INR in the range of 2.0-3.0 when using double-leaf (bicuspid) prostheses, as well as the Medtronic Hall valve (one of the most popular single-leaf artificial valves in the world). valves), or in the range of 2.5-3.5 for all other disc valves, as well as for the Starr-Edwards ball valve.
4. Salem DN, O'Gara PT, Madias C., Pauker SG; American College of Chest Physicians. Valvular and structural heart disease: American College of Chest Physicians Evidence
Mechanical mitral valve prosthesis requires maintaining the INR within 2.5-3.5 for all types of valves.
Table 1. Recommended INR value for mechanical heart valves
| Heart valve position | Risk factors for TE complications | |
| none | present | |
| Aortic | 2,0-3,0 | 2,5-3,5 |
| Mitral | 2,5-3,5 | 3,0-4,0 |
5. Methodological recommendations were reviewed and recommended by the scientific council of the Federal State Budgetary Institution “Research Institute for Complex Problems of Cardiovascular Diseases” of the Siberian Branch of the Russian Academy of Medical Sciences on July 1, 2011, updated on January 14, 2014.
However, even with recommended antithrombotic therapy, the risk of thromboembolic complications in patients undergoing heart valve replacement remains at 1-2%. The results of most clinical studies indicate that the risk of thrombosis is higher in patients with mitral valve prostheses (compared to aortic valve prostheses). If for patients with artificial aortic valves a less intensive anticoagulant regimen is possible (with a target INR of 2.0-3.0), then in the case of a mechanical mitral valve prosthesis, the anticoagulant regimen should be quite intensive (with a target INR of 2.5-3 ,5).
6. Vahanian A., Baumgartner H., Bax J. et al.; Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology; ESC Committee for Practice Guidelines. Guidelines on the management of valvular heart disease: The Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology. Eur Heart J 2007; 28 (2): 230-68.
Regardless of the type of artificial valve used, the risk of thrombosis is highest in the first few months after surgery - until the completion of epithelization processes at the site of implantation of the prosthesis. American experts consider it advisable to keep the INR within 2.5-3.5 in the first 3 months. after surgery, even for patients with an artificial aortic valve.
In addition, keeping the INR within a more stringent range (2.5-3.5) is recommended by the ACC/AHA in the presence of high-risk factors for thromboembolism, regardless of the type of prosthesis and its location. Such factors include atrial fibrillation, a history of thromboembolism, left ventricular (LV) dysfunction, and a hypercoagulable state.
Currently, there are portable devices for self-determination of INR (similar to systems for monitoring sugar levels in patients with diabetes), which help maintain INR levels in the required range. Among them, Coagucheck XS has proven itself for independent testing and immediate receipt of PTT/INR results. The device allows you to get accurate results in less than a minute, using only 8 µl (one drop of blood).
However, regardless of the chosen antithrombotic treatment strategy after heart valve replacement, regular patient monitoring, education, and close collaboration with the treating physician remain essential.
7. Butchart EG Antithrombotic management in patients with prosthetic valves: a comparison of American and European guidelines. Heart 2009;95: 430 436.
This allows for timely adjustment of drug doses, as well as changes in their thrombolytic activity, depending on the nutritional characteristics, state of the patient’s liver and kidney function.
Prevention of thrombosis in patients with bioprosthetic valves
In patients with bioprosthetic valves, less aggressive anticoagulant therapy is indicated, since in most studies the risk of thromboembolic complications in such patients, even in the absence of anticoagulant therapy, averaged only 0.7%.
According to American experts, the addition of warfarin may be useful in cases of increased risk of thromboembolism, but is not routinely recommended for all patients. When using warfarin, the INR should be kept within 2.0-3.0 if the aortic valve is replaced, and 2.5-3.5 if the mitral valve is replaced.
The use of warfarin with a target INR of 2.0-3.0 may also be appropriate in the first 3 months. after surgery and in patients with a mitral or aortic valve prosthesis without risk factors, given the increased tendency to thrombus formation in the early stages after valve replacement. Patients with a mitral valve prosthesis benefit particularly from this strategy.
Table 2. Recommended INR value for biological heart valves
| Heart valve position | Risk factors for TE complications | |
| none | present | |
| Aortic | 2,0-2,5 | 2,5-3,0 |
| Mitral | 2,5-3,0 | 3,0-3,5 |
| Tricuspid | 2,5-3,0 | 3,0-3,5 |
However, European ESC experts believe that there is currently insufficient evidence to support the need for long-term antithrombotic therapy in patients with bioprosthetic heart valves, unless these patients have any additional risk factors.
European guidelines recommend the use of warfarin in such patients only for the first 3 months. after surgery (target INR - 2.5).
Long-term (lifelong) anticoagulation therapy in patients with bioprosthetic valves may only be appropriate in the presence of high-risk factors (eg, atrial fibrillation; to a lesser extent, heart failure with LVEF <30% may be a risk factor), according to ESC guidelines6.
Thus, for patients with bioprosthetic heart valves, European experts recommend a more cautious tactic of antithrombotic therapy, while American experts consider a more aggressive approach justified. At the same time, in the United States, there is a more widespread tendency to minimize the patient’s time in hospital and the cost of his treatment, so American doctors prefer to prescribe acetylsalicylic acid to patients with bioprostheses. In Europe, they are still inclined to keep the patient in the hospital longer, if necessary, and to use warfarin in this category of patients, which is more demanding in monitoring blood coagulation parameters.
One of the most significant problems in the management of such patients in domestic healthcare settings is the inability to adequately control blood coagulation parameters against the background of constant use of anticoagulants.
It is the INR indicator that is recommended by all international guidelines as necessary to ensure the safety and effectiveness of therapy.
Recommendations for patients with a prosthetic heart valve 1.6 MB
Muscle pump
The movement of blood through the veins is ensured by a number of factors: the work of the heart, the valve apparatus of the veins, the “muscle pump”, etc. The veins of the upper and lower extremities are equipped with valves, and the deep veins are surrounded by muscles. With physical
When under load, the muscles act like pumps, putting pressure on the veins from the outside. The more frequent and active the movements, for example when walking, the more effective the “pumping action” of the muscles. True, muscle contraction, pinching blood vessels, impedes blood flow. But if the contractions are intermittent, then the decrease in blood flow during the contraction phase is effectively compensated by oxygen bound to myoglobin. Therefore, during rhythmic exercise that occurs when running, skiing, or cycling, the blood supply to the muscles of the limbs increases significantly. Contraction of the abdominal muscles forces a significant amount of blood out of the vessels of the liver, intestines and spleen, increasing blood flow to the heart and thereby affecting cardiac output.
When muscles contract, the veins in them are compressed, which immediately leads to an increase in blood flow to the right ventricle (muscle pump). An increase in the outflow of venous blood from the muscles of the lower extremities promotes rapid filling of the heart and, in addition, increases the perfusion pressure in the lower extremities by reducing the pressure in the veins of the leg and foot.
Activation of the muscle pump is accompanied by changes in the post-capillary vessels (mainly veins) of the systemic circulation.
Physical exercise causes a reflex increase in the tension of the walls of the venous vessels in both working and non-working limbs. This tension is maintained throughout the load and is proportional to its severity.
Treatment of chronic coronary heart disease
Ischemic (coronary) heart disease (CHD), which develops as a result of atherosclerosis of the coronary arteries, is the leading cause of disability and mortality in the working population throughout the world. In Russia, the prevalence of cardiovascular diseases and coronary artery disease is growing, and in terms of mortality from them, our country is one of the first places in the world, which necessitates the use of modern and effective methods of their treatment and prevention by doctors. Among the population of Russia, the prevalence of the main risk factors for the development of coronary artery disease remains high, of which smoking, arterial hypertension, and hypercholesterolemia are the most important.
Atherosclerosis is the main cause of the development of coronary artery disease. It proceeds covertly for a long time until it leads to complications such as myocardial infarction, cerebral stroke, sudden death, or to the appearance of angina pectoris, chronic cerebrovascular insufficiency, and intermittent claudication. Atherosclerosis leads to gradual local stenosis of the coronary, cerebral and other arteries due to the formation and growth of atherosclerotic plaques in them. In addition, such factors as endothelial dysfunction, regional spasms, impaired microcirculation, as well as the presence of a primary inflammatory process in the vascular wall as a possible factor in the formation of thrombosis take part in its development [1]. An imbalance of vasodilating and vasoconstrictor stimuli can also significantly change the state of the tone of the coronary arteries, creating additional dynamic stenosis to the already existing fixed one.
The development of stable angina can be predictable, for example, in the presence of factors that cause an increase in myocardial oxygen demand, such as physical or emotional stress (stress).
Patients with angina pectoris, including those who have already suffered a myocardial infarction, constitute the largest group of patients with coronary artery disease. This explains the interest of practicing physicians in the issues of proper management of patients with angina pectoris and the choice of optimal treatment methods.
Clinical forms of IHD . IHD manifests itself in many clinical forms: chronic stable angina, unstable (progressive) angina, asymptomatic IHD, vasospastic angina, myocardial infarction, heart failure, sudden death. Transient myocardial ischemia, usually resulting from narrowing of the coronary arteries and increased oxygen demand, is the main mechanism for the development of stable angina.
Chronic stable angina is usually divided into 4 functional classes according to the severity of symptoms (Canadian classification).
The main goals of treatment are to improve the patient's quality of life by reducing the frequency of angina attacks, preventing acute myocardial infarction, and improving survival. Antianginal treatment is considered successful in the case of complete or almost complete elimination of angina attacks and the patient’s return to normal activity (angina pectoris not higher than functional class I, when painful attacks occur only under significant loads) and with minimal side effects of therapy [2, 3].
In the treatment of chronic ischemic heart disease, 3 main groups of drugs are used: β-blockers, calcium antagonists, organic nitrates, which significantly reduce the number of angina attacks, reduce the need for nitroglycerin, increase exercise tolerance and improve the quality of life of patients.
However, medical practitioners are still reluctant to prescribe new effective drugs in sufficient doses. In addition, if there is a large selection of modern antianginal and anti-ischemic drugs, outdated and insufficiently effective ones should be excluded. A frank conversation with the patient, an explanation of the cause of the disease and its complications, and the need for additional non-invasive and invasive research methods helps to choose the right treatment method.
According to the results of the ATP-survey (Angina Treatment Patterns), in Russia, when choosing antianginal drugs with a hemodynamic mechanism of action in monotherapy, preference is given to nitrates (11.9%), then b-blockers (7.8%) and calcium antagonists (2 .7%) [4].
β-blockers are the first choice drugs for the treatment of patients with angina pectoris, especially in patients who have had a myocardial infarction, as they lead to a reduction in mortality and the incidence of recurrent infarction. Drugs of this group have been used in the treatment of patients with coronary artery disease for more than 40 years.
β-blockers cause an antianginal effect by reducing the myocardial oxygen demand (due to a decrease in heart rate, lowering blood pressure and myocardial contractility), increasing oxygen delivery to the myocardium (due to increased collateral blood flow, its redistribution in favor of the ischemic layers of the myocardium - subendocardium ), antiarrhythmic and antiaggregation effects, reducing calcium accumulation in ischemic cardiomyocytes.
Indications for the use of β-blockers are the presence of angina, angina with concomitant arterial hypertension, concomitant heart failure, “silent” myocardial ischemia, myocardial ischemia with concomitant rhythm disturbances. In the absence of direct contraindications, β-blockers are prescribed to all patients with coronary artery disease, especially after myocardial infarction. The goal of therapy is to improve the long-term prognosis of a patient with coronary artery disease.
Among β-blockers, propranolol (80–320 mg/day), atenolol (25–100 mg/day), metoprolol (50–200 mg/day), carvedilol (25–50 mg/day), bisoprolol (5 - 20 mg/day), nebivolol (5 mg/day). Cardioselective drugs (atenolol, metoprolol, betaxolol) have a predominantly blocking effect on β1-adrenergic receptors.
One of the most widely used cardioselective drugs is atenolol (tenormin). The initial dose is 50 mg/day. In the future, it can be increased to 200 mg/day. The drug is prescribed once in the morning. In case of severe renal impairment, the daily dose should be reduced.
Another cardioselective β-blocker is metoprolol (Betaloc). Its daily dose is on average 100–300 mg, the drug is prescribed in 2 doses, since the β-blocking effect can be observed for up to 12 hours. At present, long-acting metoprolol preparations have become widespread - betaloc ZOK, metocard, the duration of the effect of which reaches 24 hours.
Bisoprolol (Concor), in comparison with atenolol and metoprolol, has more pronounced cardioselectivity (in therapeutic doses it blocks only β1-adrenergic receptors) and a longer duration of action. It is used once a day at a dose of 2.5–20 mg.
Carvedilol (Dilatrend) has a combined non-selective β-, α1-blocking and antioxidant effect. The drug blocks both β1- and β2-adrenergic receptors, without having its own sympathomimetic activity. Due to the blockade of α1-adrenergic receptors located in the smooth muscle cells of the vascular wall, carvedilol causes pronounced vasodilation. Thus, it combines β-adrenergic blocking and vasodilating activity, which is mainly responsible for its antianginal and anti-ischemic effect, which persists with long-term use. Carvedilol also has a hypotensive effect and inhibits the proliferation of smooth muscle cells, which plays a proatherogenic role. The drug is able to reduce the viscosity of blood plasma, aggregation of erythrocytes and platelets. In patients with impaired left ventricular (LV) function or circulatory failure, carvedilol has a beneficial effect on hemodynamic parameters (reduces pre- and afterload), increases ejection fraction and reduces LV size. Thus, the administration of carvedilol is indicated primarily for patients with coronary artery disease who have suffered a myocardial infarction, with heart failure, since in this group of patients its ability to significantly improve the prognosis of the disease and increase life expectancy has been proven. When comparing carvedilol (average daily dose 20.5 mg) and atenolol (average daily dose 25.9 mg), it was shown that both drugs, prescribed 2 times a day, are equally effective in the treatment of patients with stable angina pectoris [5]. One of the guidelines for the adequacy of the dose of beta-blockers used is a decrease in heart rate at rest to 55–60 beats/min. In some cases, in patients with severe angina, resting heart rate may be reduced to less than 50 beats/min.
Nebivolol (nebilet) is a new selective β1-blocker that also stimulates the synthesis of nitric oxide (NO). The drug causes hemodynamic unloading of the heart: it reduces blood pressure, pre- and afterload, increases cardiac output, and increases peripheral blood flow. Nebivolol is a b-blocker with unique properties, which lie in the ability of the drug to participate in the process of synthesis of relaxing factor (NO) by endothelial cells. This property gives the drug an additional vasodilating effect. The drug is used primarily in patients with arterial hypertension with attacks of angina pectoris.
Celiprolol (200–600 mg/day) - a third-generation β-blocker - differs from other β-blockers in its high selectivity, moderate stimulation of β2-adrenergic receptors, direct vasodilating effect on blood vessels, modulation of the release of nitric oxide from endothelial cells, and the absence of adverse metabolic effects. The drug is recommended for patients with coronary artery disease with chronic obstructive pulmonary diseases, dyslipidemia, diabetes mellitus, and peripheral vascular diseases caused by tobacco smoking [6]. Celiprolol (200–600 mg/day), atenolol (50–100 mg/day), propranolol (80–320 mg/day) have comparable antianginal efficacy and equally increase exercise tolerance in patients with stable angina pectoris.
β-blockers should be given preference when prescribed to patients with coronary artery disease if there is a clear connection between physical activity and the development of an angina attack, with concomitant arterial hypertension; the presence of rhythm disturbances (supraventricular or ventricular arrhythmia), previous myocardial infarction, severe anxiety. Most of the adverse effects of β-blockers are due to blockade of β2 receptors. The need to monitor the prescription of β-blockers and the side effects encountered (bradycardia, hypotension, bronchospasm, increased signs of heart failure, heart block, sick sinus syndrome, fatigue, insomnia) lead to the fact that the doctor does not always use these drugs. The main medical errors when prescribing β-blockers are the use of small doses of drugs, their administration less frequently than necessary, and the discontinuation of drugs when a heart rate at rest is less than 60 beats/min. One should also keep in mind the possibility of developing withdrawal syndrome, and therefore β-blockers must be discontinued gradually.
Calcium channel blockers (calcium antagonists). The main point of application of drugs of this group at the cellular level are slow calcium channels, through which calcium ions pass into the smooth muscle cells of blood vessels and the heart. In the presence of calcium ions, actin and myosin interact, ensuring contractility of the myocardium and smooth muscle cells. In addition, calcium channels are involved in the generation of pacemaker activity of sinus node cells and conduction of impulses through the atrioventricular node.
It has been established that the vasodilating effect caused by calcium antagonists occurs not only through a direct effect on the smooth muscles of the vascular wall, but also indirectly, through potentiation of the release of nitric oxide from the vascular endothelium. This phenomenon has been described for most dihydropyridines and isradipine, and to a lesser extent for nifedipine and non-hydropyridine drugs. For long-term treatment of angina from dihydropyridine derivatives, it is recommended to use only prolonged dosage forms or long-acting generations of calcium antagonists. Calcium channel blockers are powerful vasodilators; they reduce myocardial oxygen demand and dilate coronary arteries. The drugs can be used for vasospastic angina and concomitant obstructive pulmonary diseases. Additional indications for the prescription of calcium antagonists are Raynaud's syndrome, as well as (for phenylalkylamines - verapamil and benzodiazepines - diltiazem) atrial fibrillation, supraventricular tachycardia, hypertrophic cardiomyopathy. The following calcium antagonists are used in the treatment of coronary heart disease: nifedipine, immediate action 30–60 mg/day (10–20 mg 3 times) or prolonged action (30–180 mg once); immediate-release verapamil (80–160 mg 3 times daily); or prolonged action (120–480 mg once); immediate-release diltiazem (30–60 mg 4 times a day) or long-acting (120–300 mg/day once); long-acting drugs amlodipine (5–10 mg/day once), lacidipine (2–4 mg/day).
Activation of the sympathoadrenal system by dihydropyridines (nifedipine, amlodipine) is currently considered as an undesirable phenomenon and is considered the main reason for a slight increase in mortality in patients with coronary artery disease when taking short-acting dihydropyridines for unstable angina, acute myocardial infarction and, apparently, with long-term use in patients with stable angina pectoris . In this regard, it is currently recommended to use retard and prolonged forms of dihydropyridines. They have no fundamental differences in the nature of pharmacodynamic action with short-acting drugs. Due to gradual absorption, they are devoid of a number of side effects associated with sympathetic activation, so characteristic of short-acting dihydropyridines.
In recent years, evidence has emerged indicating the possibility of slowing down damage to the vascular wall with the help of calcium antagonists, especially in the early stages of the development of atherosclerosis.
Amlodipine (Norvasc, Amlovas, Nordipine) is a third generation calcium antagonist from the group of dihydropyridines. Amlodipine dilates peripheral blood vessels and reduces cardiac afterload. Due to the fact that the drug does not cause reflex tachycardia (since the sympathoadrenal system is not activated), energy consumption and myocardial oxygen demand are reduced. The drug dilates the coronary arteries and increases the supply of oxygen to the myocardium. Antianginal effect (reducing the frequency and duration of angina attacks, daily requirement for nitroglycerin), increasing tolerance to physical activity, improving systolic and diastolic heart function in the absence of a depressing effect on the sinus and atrioventricular node and other elements of the conduction system of the heart put the drug in one of the first places in the treatment of angina pectoris.
Lacidipine, a third-generation drug from the class of calcium antagonists, has high lipophilicity, interaction with the cell membrane, and independence of tissue effects from its concentration. These factors are leading in the mechanism of antiatherosclerotic action. Lacidipine has a positive effect on the endothelium, inhibits the formation of adhesion molecules, proliferation of smooth muscle cells and platelet aggregation. In addition, the drug is able to inhibit the peroxidation of low-density lipoproteins, i.e., it can affect one of the early stages of plaque formation.
The European Lacidipine Study on Atherosclerosis (ELSA) compared the intima-media thickness of the carotid artery in 2334 patients with arterial hypertension during 4 years of therapy with lacidipine or atenolol. In the patients included in the study, the carotid arteries were initially normal and/or altered. Treatment with lacidipine was accompanied by a significantly more pronounced decrease in intima-media thickness, both at the level of the bifurcation and the common carotid artery, compared to atenolol. During treatment with lacidipine compared with atenolol, the increase in the number of atherosclerotic plaques in patients was 18% less, and the number of patients in whom the number of plaques decreased was 31% more [7].
Thus, calcium antagonists, along with pronounced antianginal (anti-ischemic) properties, can have an additional anti-atherogenic effect (stabilization of the plasma membrane, preventing the penetration of free cholesterol into the vessel wall), which allows them to be prescribed more often to patients with stable angina pectoris with damage to arteries of different localizations. Currently, calcium antagonists are considered second-line drugs in patients with angina pectoris, following β-blockers. As monotherapy, they can achieve the same pronounced antianginal effect as β-blockers. The undoubted advantage of β-blockers over calcium antagonists is their ability to reduce mortality in patients who have had myocardial infarction. Studies of the use of calcium antagonists after myocardial infarction have shown that the greatest effect is achieved in individuals without severe left ventricular dysfunction, suffering from arterial hypertension, and having had a myocardial infarction without a Q wave.
Thus, the undoubted advantage of calcium antagonists is a wide range of pharmacological effects aimed at eliminating the manifestations of coronary insufficiency: antianginal, hypotensive, antiarrhythmic. Therapy with these drugs also has a beneficial effect on the course of atherosclerosis.
Organic nitrates . The anti-ischemic effect of nitrates is based on a significant change in hemodynamic parameters: a decrease in pre- and afterload of the left ventricle, a decrease in vascular resistance, including coronary arteries, a decrease in blood pressure, etc. The main indications for taking nitrates are angina pectoris and rest in patients with coronary artery disease (also in in order to prevent them), attacks of vasospastic angina, attacks of angina, accompanied by manifestations of left ventricular failure.
Sublingual nitroglycerin (0.3–0.6 mg) or nitroglycerin aerosol (Nitromint 0.4 mg) is intended for the relief of acute attacks of angina due to the rapid onset of action. If nitroglycerin is poorly tolerated, nitrosorbide, molsidomine or the calcium antagonist nifedipine can be used to relieve an attack of angina, chewing or dissolving the tablets when taking them under the tongue.
Organic nitrates (preparations of isosorbide dinitrate or isosorbide-5-mononitrate) are used to prevent angina attacks. These drugs provide long-term hemodynamic unloading of the heart, improve blood supply to ischemic areas and increase physical performance. They try to prescribe them before physical activity that causes angina. Of the drugs with proven effectiveness, the most studied are cardiquet (20, 40, 60 and 120 mg/day), nitrosorbide (40–80 mg/day), olicard retard (40 mg/day), mono poppy (20–80 mg/day ), mono mac depot (50 and 100 mg/day), efox long (50 mg/day), mono cinque retard (50 mg/day). For patients with stable angina pectoris class I-II, intermittent administration of nitrates is possible before situations that can cause an attack of angina. For patients with more severe angina pectoris class III-IV, nitrates should be prescribed regularly; In such patients, one should strive to maintain the effect throughout the day. In case of class IV angina (when angina attacks can also occur at night), nitrates should be prescribed in such a way as to ensure an effect throughout the day [8].
Nitrate-like drugs include molsidomine (Corvaton, Sidnopharm, Dilasidom), a drug that differs from nitrates in chemical structure, but is no different from them in its mechanism of action. The drug reduces vascular wall tension, improves collateral circulation in the myocardium, and has anti-aggregation properties. Comparable doses of isosorbide dinitrate and corvatone are 10 mg and 2 mg, respectively. The effect of Corvaton appears after 15–20 minutes, the duration of action is from 1 to 6 hours (on average 4 hours). Corvaton retard 8 mg is taken 1-2 times a day, since the effect of the drug lasts more than 12 hours.
The weakness of nitrates is the development of tolerance to them, especially with long-term use, and side effects that complicate their use (headache, palpitations, dizziness), caused by reflex sinus tachycardia. Transdermal forms of nitrates in the form of ointments, patches and discs, due to the difficulty of dosing them and the development of tolerance to them, have not found widespread use. It is also unknown whether nitrates improve the prognosis of a patient with stable angina with long-term use, which makes the advisability of their use in the absence of angina pectoris (myocardial ischemia) questionable.
When prescribing drugs with a hemodynamic mechanism of action in elderly patients, the following rules should be observed: start treatment with lower doses, carefully monitor unwanted effects, and always consider changing the drug if it is poorly tolerated and insufficiently effective.
Combination therapy . Combination therapy with antianginal drugs in patients with stable angina of class III-IV is carried out for the following indications: impossibility of selecting effective monotherapy; the need to enhance the effect of monotherapy (for example, during periods of increased physical activity of the patient); correction of unfavorable hemodynamic changes (for example, tachycardia caused by nitrates or calcium antagonists from the dihydropyridine group); when angina is combined with arterial hypertension or heart rhythm disturbances that are not compensated for in cases of monotherapy; in case of patient intolerance to generally accepted doses of drugs during monotherapy, small doses of drugs can be combined to achieve the desired effect.
The synergism of the mechanisms of action of various classes of antianginal drugs is the basis for assessing the prospects of their combinations. When treating a patient with stable angina, doctors often use various combinations of antianginal drugs (β-blockers, nitrates, calcium antagonists). In the absence of effect from monotherapy, combination therapy is often prescribed (nitrates and β-blockers; β-blockers and calcium antagonists, etc.).
The results of the ATP-survey study (review of the treatment of stable angina) showed that in Russia 76% of patients receive combination therapy with hemodynamic drugs, while in more than 40% of cases - a combination of nitrates and b-blockers [4]. However, their additive effects have not been confirmed in all studies. The guidelines of the European Society of Cardiology (1997) indicate that if one antianginal drug is ineffective, it is better to first evaluate the effect of another, and only then use the combination [9]. The results of pharmacological controlled studies do not confirm that combination therapy with a beta-blocker and a calcium antagonist is accompanied by a positive additive and synergistic effect in the majority of patients with coronary artery disease. Prescribing 2 or 3 drugs in combination is not always more effective than therapy with one drug at an optimal dose [10]. We must not forget that the use of multiple drugs significantly increases the risk of adverse events associated with effects on hemodynamics.
The modern approach to combination therapy of patients with stable angina pectoris implies the advantage of combining antianginal drugs with multidirectional effects: hemodynamic and cytoprotective.
The main disadvantages of domestic pharmacotherapy for stable angina include the often erroneous, according to modern concepts, choice of a group of antianginal drugs (as a rule, nitrates are prescribed (80%)), the frequent use of clinically insignificant dosages and the unreasonable prescription of combination therapy with a large number of antianginal drugs [4] .
Metabolic agents. Trimetazidine (preductal) causes inhibition of fatty acid oxidation (by blocking the enzyme 3-ketoacyl-coenzyme A-thiolase) and stimulates the oxidation of pyruvate, i.e., it switches myocardial energy metabolism to glucose utilization. The drug protects myocardial cells from the adverse effects of ischemia, while reducing intracellular acidosis, metabolic disorders and damage to cell membranes. A single dose of trimetazidine is not able to relieve or prevent an attack of angina. Its effects are observed mainly during combination therapy with other antianginal drugs or during a course of treatment. Preductal is effective and well tolerated, especially in groups at high risk of developing coronary complications, such as patients with diabetes mellitus, the elderly and those with left ventricular dysfunction.
The combination of preductal with propranolol was significantly more effective than the combination of this β-blocker with nitrate. Trimetazidine (preductal 60 mg/day), preductal MB (70 mg/day) have an anti-ischemic effect, but more often they are used in combination with basic hemodynamic antianginal drugs.
In Russia, a multicenter, single-blind, randomized, placebo-controlled, parallel-group study, TAST (Trimetazidin in patients with Angina in Combination Therapy), was conducted, which included 177 patients suffering from class II-III angina, partially relieved by nitrates and β-blockers, to evaluate the effectiveness of the preductal in combination therapy with nitrates or β-blockers. Evaluation of the effectiveness of treatment was carried out according to the following criteria: time until the onset of ST segment depression by 1 mm during stress tests, time of onset of angina pectoris, increase in the duration of the stress test. It was found that the preductal significantly increased these indicators. There are a number of clinical situations in which trimetazidine, apparently, can be the drug of choice in elderly patients, with circulatory failure of ischemic origin, sick sinus syndrome, with intolerance to antianginal drugs of the main classes, as well as with restrictions or contraindications to their use [eleven].
Drugs with antianginal properties include amiodarone and other “metabolic” drugs (ranolazine, L-arginine), as well as ACE inhibitors, selective heart rate inhibitors (ivabradine, procolaran). They are used mainly as an adjuvant therapy, prescribed in addition to the main antianginal drugs [12, 17].
The problem of drug treatment of patients with coronary artery disease is the patients’ insufficient adherence to the chosen therapy and their insufficient willingness to consistently change their lifestyle. During drug treatment, proper regular contact between the doctor and the patient is necessary, informing the patient about the nature of the disease and the benefits of prescribed drugs to improve the prognosis. When trying to influence the prognosis of a patient’s life with the help of drug therapy, the doctor must be sure that the medications he prescribes are actually taken by the patient, and in appropriate doses and according to the recommended treatment regimen.
Surgery . If drug therapy is ineffective, surgical treatment methods are used (myocardial revascularization procedures), which include: percutaneous transluminal coronary angioplasty, implantation of coronary stents, coronary artery bypass surgery. In patients with coronary artery disease, it is important to determine individual risk based on clinical and instrumental indicators, which depends on the corresponding clinical stage of the disease and the treatment provided. Thus, the maximum effectiveness of coronary bypass surgery was observed in patients with the highest preoperative risk of developing cardiovascular complications (with severe angina and ischemia, extensive lesions of the coronary arteries, impaired LV function). If the risk of complications of coronary artery disease is low (single artery disease, absence or mild ischemia, normal LV function), surgical revascularization is usually not indicated until the ineffectiveness of drug therapy or coronary angioplasty has been established. When deciding whether to use coronary angioplasty or coronary bypass surgery to treat patients with damage to multiple coronary arteries, the choice of method depends on the anatomical features of the coronary bed, LV function, the need to achieve complete myocardial revascularization and patient preferences [13].
Thus, with the methods of combating cardiovascular diseases that exist today (Table), it is important for the doctor to be aware of the latest advances in medicine and make the right choice of treatment method.
For questions regarding literature, please contact the editor.
D. M. Aronov , Doctor of Medical Sciences, Professor V. P. Lupanov , Doctor of Medical Sciences, State Research Center for Preventive Medicine of the Ministry of Health of the Russian Federation, Institute of Clinical Cardiology named after. A. L. Myasnikov Russian Cardiological Research and Production Complex of the Ministry of Health of the Russian Federation, Moscow