A stroke is a complex disorder of cerebral circulation that can occur to a person at any age. Even children are not immune from strokes. This condition occurs when normal blood flow to the brain is stopped due to blocked or ruptured blood vessels, causing loss of some brain functions.
1. Causes of stroke in children
1.1 Causes of hemorrhagic stroke
1.2 Causes of ischemic stroke
2. Treatment and rehabilitation after stroke
There are three different ages when a child may experience a stroke:
- in the womb;
- in the newborn phase;
- under the age of 18.
It is important to remember that the identification of the disorder, as well as the method of further treatment, directly depends on the age of the child. Experts note that most often strokes in children occur in the first two age phases. The severity of this disorder is determined by its location in the brain.
Pediatric stroke can be of two types:
- ischemic (caused by blockage of blood vessels);
- hemorrhagic (caused by rupture of blood vessels).
Introduction
The study of cerebral circulatory disorders (CVA) of the hemorrhagic type in childhood is an urgent task due to the tendency to increase the frequency of pathology, as well as the high level of mortality and disability associated with CCD.
Thus, the incidence of hemorrhagic stroke (HS) in children aged 1 month to 18 years is 2.9 cases per 100 thousand children per year [1]. In the 1st month of life, there are 28.6 cases of HI per 100 thousand newborns among those born before the 31st week of gestational age and 24.7 cases among those born after the 31st week [2, 3]. About 40% of all cases of HI develop in the 1st year of life [4].
Mortality rates from HI in children reach 29–41% [5–7]. Disability, according to L. Beslow and L. Jordan. [8], is registered in 50% of children who survived a stroke.
In 1995, the World Health Organization proposed a definition of stroke as “the rapid development of clinical signs of focal or global impairment of cerebral function that persists for 24 hours or more, leading to death in the absence of causes other than stroke.”
However, the clinical manifestations of the initial period of HI in children differ from those in adults and have their own characteristics depending on age. According to the literature [9–11], in children of the older age group at the onset of HI, neurological manifestations are similar to those of adult patients. The main symptoms are headache, difficulty speaking, hemiparesis and visual deficits. S. Gupta et al. [12] described the development of monoplegia, as well as hemi- and tetraplegia, which was accompanied by loss of consciousness, as a cardinal symptom of HI in older children. S.K. Evtushenko et al. [13] observed hemiplegia in combination with visual field impairment and speech disorder in the acute period of HI. K. Ibraim da Freiria et al. [14] in the initial phase of the disease revealed a combination of hemiplegia, speech difficulties and behavioral disturbances. A number of authors [15-17], reviewing the clinical features of the onset of HI in children of the older age group, noted the sudden onset of headache, vomiting, changes in the level of consciousness and focal neurological deficit. S. Fox et al. [15] emphasized that intracranial hypertension and cerebral edema rapidly progress after HI, leading to secondary brain damage.
The younger the child, the more nonspecific the initial clinical features of HI may be [16]. Thus, seizures are among the common initial manifestations of HI in young children [18]. K.G. Kremets [19] observed focal seizures in 10% of cases of neonatal HI, which most often occurred in one limb. According to the results of the study by A.Yu. Ratner [20], in children of the younger age group, HI initially manifested itself with general cerebral symptoms: vomiting, convulsions and coma. According to G. De Veber et al. [21], perinatal HI began with lethargy and convulsions. A. Meyer-Heim et al. [22] pointed to more diverse manifestations of the acute period of HI, when, along with irritability or drowsiness, problems associated with feeding the baby, vomiting and symptoms of peripheral hemodynamic disorders arose. According to K. Calder et al. [23], one of the signs of HI in infants is a bulging large fontanel.
Certain types of stroke are characterized by different clinical manifestations. Thus, subarachnoid hemorrhage (SAH) can manifest itself with sudden onset, headache, irritability, photophobia and meningeal syndrome. With ventricular hemorrhage, depression of consciousness, respiratory rhythm disturbances with hypoventilation, apnea, generalized tonic convulsions or decerebrate rigidity, bradycardia, arterial hypotension, bulging fontanel and tetraparesis are more common. With intracerebellar hemorrhages, symptoms of compression of the brain stem are detected: bradycardia, apnea, increased intracranial pressure with bulging of the fontanelle, dehiscence of the skull sutures, moderate dilatation of the ventricles, as well as paresis of facial muscles, tetraparesis. With subdural hemorrhage, signs of compression of the brain stem also appear: anisocoria with the absence of photoreaction of the pupils, stupor or coma, as well as stiff neck, opisthotonus and bradycardia [24, 25]. Bulbar dysfunction indicates involvement of the brainstem, while aphasia suggests involvement of the basal ganglia, thalamus, or cerebral hemispheres [26].
Information on the clinical manifestations of HI in infants is still more limited. In the literature there are only indications of the heterogeneity of the clinical course of the disease in children of this age group. At the same time, the spectrum of nosological pathology can include both somatic and surgical conditions (traumatic brain injury), as well as infections of the nervous system, encephalopathy, etc. In this regard, HI in infants is often diagnosed late or not diagnosed at all [ 24, 27, 28]. Accordingly, in many cases, treatment and preventive care is provided with a delay, which leads to the development of irreversible consequences (increased morbidity and mortality) and determines the importance of studying HI in infants
The purpose of the study was to study the neurological manifestations of HI in infants.
What diagnoses are often confused with a stroke in a child?
Pediatricians have such a concept as alertness to a specific pathology. Due to the fact that strokes in children are much less common than in adults, when a young specialist starts working, he loses this element of alertness.
When a patient develops neurological symptoms, this is often assessed from the perspective of other diagnoses, for example, meningoencephalitis or neuroinfections, which are more common in children and which also require emergency hospitalization. Therefore, even if it is a stroke, the child does not remain without the attention of doctors.
Material and methods
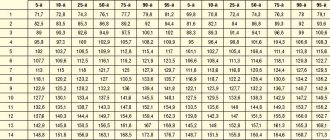
A retrospective analysis of the medical records of 140 infants hospitalized with HI in the pediatric and emergency care clinic was carried out: 95 (67.86%) boys and 45 (32.14%) girls.
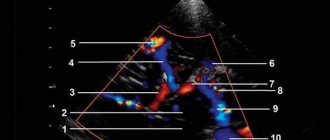
We paid attention to the initial manifestations of the disease (based on the results of a survey of parents). The neurological examination data available in the medical history were analyzed both upon admission of patients to the hospital and at subsequent stages of disease development. The functions of cranial nerves, muscle strength and tone, tendon and skin reflexes, pain sensitivity, and the presence or absence of symptoms of meningeal irritation were assessed. The level of disturbance of consciousness was detected using the pediatric Glasgow Coma Scale (GCS). The patients' medical histories reflected the results of brain neuroimaging performed using computed tomography, which made it possible to clarify the location of the hemorrhage.
Important for achieving the goal of the study was also the availability of materials concerning the general somatic condition of patients (data on the examination of internal organs, results of constant monitoring of respiratory rate, heart rate, heart rhythm, etc.).
At what age can a child start showing symptoms of a stroke?
The problem of early stroke is interesting due to age. As a rule, it occurs in children under 3-5 years of age. Not among teenagers, as it would seem. Moreover, more than half of the cases are perinatal strokes. That is, strokes that occur in utero, starting from 22 weeks of gestation, or immediately after birth - up to one month of age.
But such a stroke is always clearly monitored and verified quite well, because these children undergo an ultrasound of the brain and, if necessary, a decision is made on additional research, for example, an MRI.
results
During the perinatal period (from the moment of birth to the 28th day of life), 16 (11.43%) children with G.I. Over 28 days of life, 124 (88.57%) children were hospitalized. Children of the 2nd and 3rd months of life predominated - 117 (83.57%): 2nd month - 101 (72.14%) children, 3rd month - 16 (11.43%). At the age of 4 months to 1 year, 7 (5.0%) patients with HI were hospitalized.
Among the complaints (parents) indicated lethargy in 101 (72.14%) patients, which in 16 (11.42%) children turned into drowsiness, and in 1 child into loss of consciousness. In 39 (27.86%) children, the disease began with anxiety, in 19 (13.57%) monotonous crying appeared, 89 (63.57%) children at the onset of HI refused breastfeeding, in 20 (14.28%) regurgitation occurred, and 66 (47.14%) had vomiting. 21 (15.0%) children had seizures. In 7 (5%) patients, tilting of the head was detected. 101 (72.14%) patients had pale skin, 2 (1.42%) had icteric skin discoloration. 10 (7.14%) children had skin rashes, 1 had mucous membranes, 1 had bruises on the face, and 1 patient had nosebleeds. In 4 (2.85%) children, the absence of movements in the right or left upper limb, as well as the right or left lower limb, was recorded. 29 (20.71%) children had a cough, 11 (7.85%) had groaning breathing, and 3 (0.80%) had respiratory arrest. Diarrhea and loose stools were noted in 7 (5.0%) children, and 3 (2.14%) had blood in the stool. In 3 (2.14%) patients, parents noted purulent discharge from the eyes. Parents recorded an increase in body temperature up to 37-37.9 °C in 29 (20.71%) children, within 38-38.9 °C - in 49 (35.0%), above 39 °C - in 8 ( 5.71%) patients.
Neuroimaging examination at the time of admission to the hospital revealed a high frequency of SAH - in 32 (22.85%) children, as well as such clinical and anatomical forms of SAH as combined subarachnoid-parenchymal hemorrhage - in 24 (17.14%) patients, SAH in combination with non-traumatic subdural hematoma - in 15 (10.71%) cases, SAH and ventricular hemorrhage - in 6 (4.28%) children. Mixed subarachnoid-parenchymal and non-traumatic subdural hemorrhage was observed in 18 (12.85%) patients, subarachnoid-parenchymal and ventricular hemorrhage - in 13 (9.28%) patients, subarachnoid-parenchymal, ventricular, subdural hemorrhage - in 2 (1, 42%). Much less frequently, 1 child had mixed subarachnoid-ventricular and subdural hemorrhage. In 8 (5.71%) children, the reason for hospitalization was non-traumatic subdural hematoma, in 8 (5.71%) - non-traumatic subdural hematoma and parenchymal hemorrhage, in 7 (5.0%) - isolated parenchymal hemorrhage. In 2 (1.42%) patients, HI was represented by parenchymal and ventricular hemorrhage, in 4 (2.85%) - isolated ventricular hemorrhage.
A neurological examination of children upon admission to the hospital revealed the presence of both meningeal and focal neurological symptoms, as well as signs of increasing intracranial hypertension and the formation of cerebral edema.
The GCS score in 3 (2.14%) cases was 15 points, in 29 (20.71%) - 12 points, in 39 (27.86%) - 9 points, in 29 (20.71%) - 7 points, in 37 (26.43%) - 5 points, in 3 (2.14%) cases - 4 points.
102 (72.85%) patients had a meningeal symptom complex, represented by stiffness of the neck muscles. 38 (27.14%) children had convulsions, 7 (5.0%) had hyperesthesia. Impaired thermoregulation manifested itself in the form of hyperthermia, which was detected in 91 (65.0%) patients on the day of hospitalization. An increase in body temperature up to 37-37.9 °C was recorded in 31 (22.14%) children, within 38-38.9 °C - in 56 (40.0%) children, above 39 °C - in 4 ( 2.85%) of patients, which was probably due to concomitant infectious pathology [29].
Common clinical manifestations of HI in infants were: increase in intracranial pressure, formation of cerebral edema. At the same time, 125 (89.28%) children had bulging and tension of the large fontanel. In 3 (2.14%) cases, the large fontanelle, on the contrary, sunk. Only 12 (8.57%) children had a satisfactory condition of the large fontanel.
The diffuse nature of brain damage due to progressive intracranial hypertension and cerebral edema was accompanied by floating movements of the eyeballs in 29 (20.71%) children.
The syndrome of motor disorders was manifested by hemiparesis in 17 (12.14%) and tetraparesis in 1 child. Impaired motor reactions in the form of limited movements in the limbs on the right were observed in 6 (4.29%) patients, on the left - in 11 (7.85%), which indicated a predominant lesion of the right hemisphere of the brain. Extrapyramidal movement disorders were manifested by changes in muscle tone in the form of hypertension in 98 (70.0%) patients, and in the form of hypotension in 35 (25.0%) children. Muscle atony was observed in 4 (2.86%) children. Only 3 (2.14%) patients had satisfactory muscle tone. In 103 (73.57%) cases, high tendon reflexes with expansion of reflexogenic zones were noted. Decreased tendon reflexes were observed in 29 (20.74%) patients, areflexia - in 3 (2.14%). Tongue deviation to the right was detected in 3 (2.14%) patients.
The results of the study of the pupils showed the same size in 73 (52.14%) children, right-sided pupil dilation was observed in 36 (25.72%), left-side dilation - in 31 (22.14%) patients. Optic nerve palsy was manifested by a decrease in the reaction of the pupils to light in 54 (38.57%) children, and the absence of a reaction of the pupils to light in 12 (8.57%). The photoreaction of the pupils was determined in 74 (52.85%) cases.
41 (29.28%) children had horizontal, 3 (2.14%) children had vertical nystagmus. 101 (72.14%) patients had a positive Babinski reflex.
Paralysis of the facial nerve was manifested by flattening of the nasolabial fold on the left in 23 (16.42%) children, on the right - in 2 (1.42%). Lagophthalmos was observed in 2 (1.42%) cases.
Damage to the upper parts of the brainstem and oculomotor nerve palsy manifested as strobism in 26 (18.57%) patients. Oculomotor disorders were also accompanied by ptosis on the right in 9 (6.42%) cases, on the left - in 3 (2.14%) cases. A negative corneal reflex was found in 16 (11.42%) children.
Paresis of upward gaze was detected in 1 child, paresis of gaze to the left - in 6 (4.28%), paresis of gaze to the right - in 2 (1.42%).
One child was diagnosed with aphonia. Bulbar disorders with dysfunction of swallowing, sucking and a negative pharyngeal reflex were registered in 44 (31.42%) children. Assessment of vital functions revealed bradycardia (less than 70 beats/min) in 42 (30.0%) patients, moderate and severe tachycardia with a heart rate over 120 beats/min in 95 (67.85%) children. Age-appropriate heart rhythm was observed in 3 (2.14%) patients. In most cases, 102 (72.85%) children had hyperventilation disorders in the form of tachypnea (40 respiratory movements in 1 minute or more) with the participation of auxiliary muscles. Bradypnea with a respiratory rate of less than 30 respiratory movements per minute or apnea (breathing cessation for more than 15 seconds) was recorded in 38 (27.15%) children. Vegetative signs were pale skin in 31 (22.14%) patients. However, 59 (42.14%) patients had icteric discoloration of the skin. Petechial rashes on the skin were detected in 1 (0.71%) child, petechial hemorrhage on the palate - in 10 (7.14%) children. An increase in liver size was found in 61 (43.57%) children. Gastrointestinal bleeding was observed in 3 (2.14%) cases, frequent bowel movements - in 5 (3.57%) children, decreased urination - in 5 (3.57%) patients, purulent discharge from the eyes - in 4 (2 .85%) patients.
Causes and signs: what can cause a stroke in children?
According to European registries, about 70% of childhood strokes are ischemic. The rest are hemorrhagic.
Ischemic stroke itself can be different. Most often, it occurs when the flow through the arterial bed directly to the part of the brain that this vessel supplies with blood is disrupted. There are a huge number of diseases that can cause it.
The first fairly large group is cardiovascular pathology. These are usually heart defects, heart rhythm disturbances. Even the surgery performed does not reduce the risk of stroke.
This also includes inflammatory heart diseases - carditis. If there are bacterial plaques on the heart valve leaflets, they come off when the heart contracts. Any embolus blocks the passage of the vessel, as a result, a section of brain tissue does not receive blood supply and ischemia occurs in it.
The second group includes neuroinfections. A number of studies have shown that the presence of herpes can cause complications such as stroke.
Another group is hematological diseases with blood clotting disorders. There is such a thing as a hemodynamic stroke. It occurs when a child has a large loss of blood, the pressure decreases and disturbances occur that do not compensate the brain with blood flow.
And this is not the entire list of causes of stroke.
Is it possible for a child to have a recurrence of stroke?
It all depends on the reason. Let's say a child has chronic leukemia as a certain form of blood cancer. It would seem that he was cured, he was given chemotherapy. It may be stable for a certain time. Could his cancer recur? Maybe. So, with relapses, a second stroke is possible.
There are children with hematological diseases who have mutations and a hereditary predisposition to them. This may be thrombophilia or Leiden factor. In this category of children, the likelihood of stroke recurrence is present, but small - up to 1-5%.
Who is more likely to have a stroke, boys or girls? There is no clear difference in hemorrhagic strokes. On ischemic data vary. Some studies say that such a stroke occurs more often in girls, others - in boys, the specialist says.
How to protect your child from stroke?
If a child goes to a sport where there is heavy load, it is recommended that parents take a certificate from a pediatrician. The doctor usually asks if there are any complaints. It makes sense to do an ultrasound of the heart, an electrocardiogram and consult a cardiologist. Further, this child will be observed in one way or another in a sports dispensary. In this case, parents follow the path of prevention.
If there are unusual conditions that the child has not had before, you should consult a doctor in a timely manner. Moreover, in Belarus it is possible not only to call an ambulance, but also to come to the emergency room yourself. There the child is examined, and the diagnosis is verified fairly quickly.
The fight for knowledge
It’s still not easy for Ilya to study. At nine years old, he is in first grade, mastering the eighth grade program. True, from home.
“The correctional school is located fifteen kilometers from home. There are fifteen people in the class. When we started studying, Ilya could sit quietly for about twenty minutes. Now, according to the teacher, he can endure a lesson for forty minutes. But there are three lessons at school. That's why I haven't decided to send him to class yet. The teacher comes to our house,” Anna clarifies.
“Teacher Anastasia Alexandrovna,” Ilya adds busily. – We read and write with her. Have you seen the series “Dog”?”
Ilya masters the educational material unevenly. Mathematics goes back and forth, writing and reading are worse, but he can’t even see a textbook on the world around him, he doesn’t like this subject so much. The seasons are difficult for him, he doesn’t recognize animals well – maybe that’s why he doesn’t like this subject.
The family's plans for Ilya's future are modest.
“I certainly don’t hope that he will graduate from college. I would be able to read, count and look after myself. But you can’t imagine how responsive and grateful he is.”
What do the statistics say: how younger is stroke?
On average, childhood strokes occur in 1.5-13 cases per 100 thousand children worldwide. In many countries, since 2007, patient registries have been created, which indicate the number of children admitted to hospitals with stroke, their age, the nature of the disease and its consequences.
The register has been operating in Moscow since 2021. In Belarus, there are no general data yet, but only in, where the Department of Child Neurology is located, on average up to 20 children are admitted per year. “This is not a lot, so we cannot talk about the widespread occurrence, or the fact that stroke is becoming younger globally,” the specialist notes.
Photos from open sources
Read ndsmi.by on social networks: VKontakte, Odnoklassniki, Facebook, instagram, twitter, Telegram
What are the risk factors for stroke in a child?
Sometimes strokes occur during physical activity. And these are not only active forms of physical activity, such as running or jumping, but even such provocations as straining during bowel movements are possible. In this case, the embolus breaks off if there were any thrombotic masses, which completely shuts down the vessel. This leads to loss of consciousness and convulsions.
Therefore, it is a priori impossible to say that parents may miss that the child is having a stroke. Neurological symptoms will always be present; they arise acutely and unexpectedly. But at the stage of the first and second days, even pediatricians may have doubts if an MRI is not performed. Because, unlike adults, children experience a slight rise in temperature and in the presence of inflammatory reactions, if the child is punctured, there may even be changes in the cerebrospinal fluid. Therefore, sometimes even pediatricians take time, but this child will definitely not be at home - he will go to the hospital.