Venous discirculation in childhood and adolescence
Introduction
Vascular lesions of the nervous system are an important problem in modern clinical neurology.
The study of cerebral venous circulation disorders remains one of the urgent tasks of modern medicine. The improvement of ultrasound equipment, as well as its software, has led to the fact that when studying blood flow in the arteries of the brain, it is possible to assess the state of venous blood flow at a fairly good level.
However, the main problem is that the data on the normative values of velocities in the venous system of the brain are extremely scattered, fragmentary and not always unambiguous.
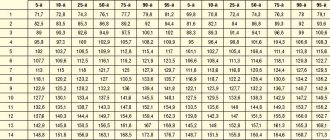
In this regard, you often have to rely on your own experience, taking as a basis data from a number of literary sources (Table 1), which are more consistent with the features of this device, the quality of the resulting image and the age of the patient. The small number of ultrasound studies, which would contain data on the state of venous blood flow at the extra- and even more so at the intracranial levels, is explained primarily by hardware features, and only then by the insufficient amount of information on this issue in the periodical literature, the complexity of the spatial-anatomical three-dimensional perception of the intracranial venous system by diagnosticians, low need for such studies on the part of neurologists. Table 1
. Blood flow indicators (Vmax, cm/s) in the internal jugular veins and in the main intracranial veins/sines of the brain.
| Author | Internal jugular vein | Middle cerebral vein | Vienna Rosenthal | Vienna Galena | Direct sine | Internal cerebral vein | Vertebral veins |
| V.G. Lelyuk, S.E. Lelyuk, 2003 [1] | 7-45 right\ 12-33 left | 9 | 11 | 15 | |||
| J. Valdueza et al., 1996 [2] | 6-18 | 4-17 | |||||
| BG Schoser, 1999 [3] | 5-12 | ||||||
| E. Stolz et al., 1997 [4] | 13,8 ± 8,9 | 13,7 ± 4,7 | 31,7 ±15,6 | ||||
| R. Baumgartner et al., 1997 [5] | 4-15 | 7-19 | 12-39 | 10-18 | |||
| R. Aaslid, 1991 [6] | 23 ± 3 | ||||||
| V.A. Shakhnovich, 1998 [7] | 14-28 | ||||||
| M.L. Dicheskul et al., 2008 [8] | 9,8-20,9 | ||||||
| G.A. Ivanichev, G.B. Dolgikh, 2007 [9] | 22,0 ± 4,6* 20,1 ± 3,2** | 17,7 ± 3,3* 16,2 ± 2,2** | |||||
| G.B. Dolgikh, G.A. Ivanichev, 2008 [10] | 13,6 ± 0,3 | 23,4 ± 0,9 | 18,7 ± 0,9 |
Note. * - in children aged 1-12 months; ** - in children aged 1-3 years.
The purpose of this study was to assess correlation dependencies in patients with signs of venous discirculation at the intra- and extracranial levels, cerebral venous hemodynamics in children and adolescents with a clinical picture of “cranialgia”, with clarification of the cause-and-effect relationships that determine the formation of venous discirculation.
Material and methods
The study included 106 children aged from 2 to 18 years, average age 9.87 ± 3.9 years (from 2 to 6 years - 18 people, average age 3.8 ± 1.43 years; from 7 to 18 years - 88 people, average age 11.1 ± 2.99 years), sent for examination to the diagnostic center of Kaliningrad with a headache clinic or symptoms of vertebrobasilar insufficiency. During the examination, signs of dysgemia at the intra- and extracranial levels were identified in all of them. Doppler ultrasound studies of arterial and venous blood flow at the level of the neck and base of the brain were performed on a Medison Accuvix V10 device (South Korea), in B-, C-, PW-modes, linear (L5-12 MHz) and sector phased (P2- 4 MHz) sensors. Correlation dependencies were assessed between 94 clinical and instrumental indicators.
results
As a result of the study, it was found that discirculation in the vertebral vein (PV) system, as a rule, is a consequence of pronounced extravasal influences (vascular compression) on blood flow in the internal jugular vein (IJV) on the side of registration of dyshemia (r = + 0.67; p 0.05).
Dysgemia in the vein of Galen on the right is often accompanied by an increase in the tone of the VA, ICA and MCA on the ipsilateral side (as a consequence of reflex changes), just as the former is associated with kinks and S-shaped tortuosity of the ICA on the right. The effect of ICA tortuosity on venous outflow may be due to extravasal compression of venous vessels by tortuous arterial trunks with significantly higher intravascular pressure in the places of their closest abutment.
The relationship between “headache syndrome” and accelerated venous blood flow through the veins of Galen turned out to be extremely low (r = +0.22; p
In addition, a fairly clear picture of pronounced unilateral disturbances of both arterial blood flow and venous outflow was noted, which is probably due to the unity of the autonomic innervation of the arteriovenous system “head-neck”, the presence of complex compensatory mechanisms (reflex), as well as the indirect influence of the tone of the striated muscles neck and cervical spine, which is confirmed in a number of studies.
Discussion
From our own experience of working with devices from leading manufacturers of ultrasound equipment, it should be admitted that the best quality images of the cerebral venous network were often obtained using Medison Acuvix devices. At the same time, the images were of high quality in both C and PW modes, with a minimum of artifacts and interference.
Assessment of venous blood flow at the extracranial level (jugular veins, vertebral veins) causes fewer difficulties and is available on almost any device, except, perhaps, assessment of blood flow through the vertebral veins in persons with excess body weight, widespread osteochondrosis and a short neck, when even visualization vertebral arteries is carried out with great difficulty.
The structure of the cerebral venous system is presented in Figure 1.
Rice. 1.
Arteries and veins/venous plexuses at the base of the brain [11]. 1 - sphenoid-parietal venous sinus, 2 - middle cerebral artery (MCA), 3 - middle cerebral vein (deep), 4 - posterior cerebral artery (segment P1) (PCA), 5 - basilar venous plexus, 6 - basilar (main ) artery, 7 - vein of Rosenthal (right) and branch of the posterior cerebral artery (right), 8 - vertebral artery (segment V1), 9 - marginal venous sinus, 10 - vein of Galen (great cerebral vein), 11 - straight sinus, 12 - branch of the posterior cerebral artery (left), 13 - vein of Rosenthal (left), 14 - inferior ventricular vein.
Variants of normal and pathological venous blood flow are shown in Table 2 and Figures 2-18.
table 2
. Variants of normal and impaired venous blood flow in C- and PW-regimes. Causes of venous discirculation in the main venous pools. *
| Blood Flow Options | Causes of venous discirculation |
| Rosenthal's Vienna Fig. 2, 3, 4 |
|
| Inferior ventricular vein (tributary vein of Rosenthal) Fig. 5 | |
| Middle cerebral vein Fig. 6, 7, 8 |
|
| Vienna Galena Fig. 9, 10, 11 |
|
| Vertebral vein Fig. 12, 13 |
|
| Internal jugular vein Fig. 14, 15 |
|
| External jugular vein Fig. 16 | |
| Sphenoparietal venous sinus Fig. 17, 18 |
Note
*
The following should also be considered as possible causes of venous discirculation:
- violation of the central regulatory mechanisms of vascular tone;
- hereditary constitutional predisposition, manifested by undifferentiated connective tissue dysplasia (including in the form of bone deformities and hypermobility of the joints of the cervical spine);
- consequences of perinatal pathology (cervical spine injuries [12]; perinatal hypoxic-ischemic processes [13]);
- extravasal causes of venous stagnation: tumors of the mediastinum and neck; osteochondrosis of the cervical spine; traumatic compression of the chest and abdomen, leading to compression of the superior vena cava, jugular and vertebral veins; early osteochondrosis; deforming arthrosis; spondylosis; craniovertebral anomalies (basilar compression; defects of the odontoid process of the second cervical vertebra, Kimmerle anomalies; Arnold-Chiari anomalies);
- disorders of exclusively myogenic nature; compression of the vertebral artery by the inferior oblique muscle of the capitis during tonic tension with subsequent contracture or compression by the anterior scalene muscle;
- vasculitis of cerebral vessels, rheumovasculitis, bacterial meningitis, thrombosis of intracranial venous sinuses [10].
**
The literature covers various methods for invasive and non-invasive assessment of intracranial pressure (ICP) [7, 14]. In the specialized literature, the possibility of assessing ICP by displacement of the tympanic membrane is discussed [15]. However, this technique is described only for patients with hydrocephalus. The development of non-invasive methods for measuring ICP is still relevant, with various ultrasound and telemetric measurement methods taking the leading place. However, the question of the accuracy of the data obtained with non-invasive methods remains open and requires further clarification. None of the non-invasive techniques allows you to measure the absolute value of ICP, but only extrapolates its dynamics.
The only possible method for identifying ICH in patients with chronic venous insufficiency remains a comprehensive clinical and instrumental diagnosis, including assessment of the neurological status, condition of the fundus, Echo-encephalography (EchoEG), Dopplerography of the vessels of the neck (USDG BCS) and brain (TG USDG). Only the combination of these methods can bring the researcher closer to the expected conclusion. According to H. Bode [16], it is almost impossible to detect an increase in ICP in a child with hydrocephalus, based only on Doppler data.
In the studies of Yu.A. Rosin [17] proved the presence of a pressure gradient between the vein of Galen and the straight sinus. During transoccipital examination in the oral part of the straight sinus, in the area where the vein of Galen flows into the straight sinus, high venous outflow (more than 50 cm/s) is detected in children, which significantly exceeds the blood flow in the veins of Rosenthal, internal cerebral veins and the inferior sagittal sinus.
At the same time, a number of authors note that an increase in the tone of the main cerebral arteries should be considered as a compensatory mechanism for facilitating venous outflow [18].
The main hemodynamic signs of benign intracranial hypertension with transcranial Dopplerography (TCD) are considered to be an increase in maximum velocity and increased pseudopulsation of blood flow in the cerebral veins and sinuses (veins of Rosenthal > 15 cm/s, vein of Galen > 20 cm/s and straight sinus > 30 cm/s )
[1]. It is assumed that during chronically ongoing processes in the cranial cavity, venous circulation suffers more significantly.
It has been noted that a sharp increase in the venous signal and a change in the physiological direction of blood flow along the internal ophthalmic vein to retrograde are detected on the side of the “focus” of brain damage in cases of cerebrovascular accidents and traumatic brain injury, accompanied by an increase in intracranial pressure [13].
Rice. 2.
Middle cerebral artery (MCA). Transtemporal access. Color Doppler mapping mode at the level of the anterior cerebral artery (ACA) (3), MCA (5), first (7) and second (8) segments of the PCA, vein of Rosenthal (9), vein of Galen (10), middle cerebral vein (4), inferior ventricular vein (tributary vein of Rosenthal) (6). Brain peduncles (pedunculi cerebri) (1; 2).
Rice. 3.
Middle cerebral vein (deep). Right there. Color flow control, PW mode. Flow scanning in the vein of Rosenthal. Vmax 15.88 cm/s.
Rice. 4.
Posterior cerebral artery (segment P1) (PCA). Transtemporal access. Color flow control, PW mode. Scanning of pathological accelerated flow in the vein of Rosenthal. Vmax 28.59 cm/s.
Rice. 5.
Basilar venous plexus. Transtemporal access. Color flow control, PW mode. MCA (1), PCA segment P1 (4), cerebral peduncles (6; 7), middle cerebral vein (2), vein of Rosenthal (5). Flow scanning in the inferior ventricular vein (inflow of the vein of Rosenthal) (3).
Rice. 6.
Basilar (main) artery. Transtemporal access. Color flow mode at the level of the ACA (1), MCA (2), first segment of the PCA (4), middle cerebral vein (3). Brain peduncles (pedunculi cerebri) (5; 6).
Rice. 7.
Vein of Rosenthal (right) and branch of the posterior cerebral artery (right). Right there. Color flow control, PW mode. Flow scanning in the middle cerebral vein (proximal segment).
Rice. 8.
Vertebral artery (segment V1). Transtemporal access. Color flow control, PW mode. Scanning of pathological accelerated flow in the middle cerebral vein (proximal segment). Vmax 24.62 cm/s
Rice. 9.
Marginal venous sinus. Transtemporal access. Color circulation mode at the level of the first segment of the PCA (3), vein of Rosenthal (4), vein of Galen (5). Brain peduncles (pedunculi cerebri) (1; 2).
Rice. 10.
Vein of Galena (great vein of the brain). Right there. Color flow control, PW mode. Flow scanning in the vein of Gallen. Vmax 21.18 cm/s
Rice. eleven.
Direct sine. Transtemporal access. Color flow control, PW mode. Scanning of pathological accelerated flow in the vein of Galen. Vmax 50 cm/s
Rice. 12.
Branch of the posterior cerebral artery (left). Longitudinal scanning in the projection of the V2 segment of the vertebral artery (1) and vertebral vein (2). Color flow control and PW mode. Vmax in the vertebral vein is 34.69 cm/s.
Rice. 13.
Vienna of Rosenthal (left). Longitudinal scanning in the projection of the V1 segment of the vertebral artery (1). Color flow control and PW mode. Pathological accelerated flow in the vertebral vein (2). Vmax 83.73 cm/s.
Rice. 14.
Inferior ventricular vein. Transverse scanning in the projection of the internal carotid artery (3), external carotid artery (2) and internal jugular vein (1). Color flow control and PW mode. Vmax in the internal jugular vein is 41.49 cm/s.
Rice. 15.
Transverse scanning in the projection of the internal carotid artery (1) and the tortuous internal jugular vein (2). Color flow control and PW mode. Pathologically accelerated turbulent flow in the internal jugular vein up to 80 cm/s.
Rice. 16.
Transverse scanning in the projection of the internal (1) and external (2) carotid arteries, external jugular vein (3). Color flow control and PW mode. Vmax in the external jugular vein is 22.88 cm/s.
Rice. 17.
Transtemporal access. Mode of color circulation at the level of the MCA (2), and the sphenoparietal venous sinus (1). Brain peduncles (pedunculi cerebri) (3).
Rice. 18.
Ibid (Fig. 17). Color flow control, PW mode. Flow scanning in the sphenoparietal venous sinus (1). Vmax 19.19 cm/s.
Another problem facing the researcher, even in the case when it is possible to assess the nature of venous blood flow at the intra- and extracranial level, is the correct interpretation of the results obtained. Since the available literature data does not provide a holistic picture of the causes of venous discirculation, and in some cases, increased ICP or connective tissue dysplasia is indicated as the main reason for its occurrence, without indicating the possible mechanisms of the formation of venous discirculation, the benefit of such conclusions is extremely small. It is also impossible to influence the tactics of further treatment, since the points of possible application of efforts by doctors of different specialties are unknown or not indicated.
An increase in ICP as a probable cause of venous discirculation should not be forgotten that due to its low prevalence in the population (0.025-0.05% among children and adolescents), this pathology cannot be considered as the leading etiological cause of dysgemia and is most likely a diagnosis of exclusion.
Functional disorders of the musculoskeletal system with the formation of blocks in small joints of the spine with the appearance of reflex musculoskeletal pain syndromes are unreasonably rarely diagnosed, and the role of myofascial pain syndromes, in which the muscle suffers primarily, is underestimated. An important role in this in children is played by certain injuries to the cervical spine in the anamnesis (mainly during childbirth). The literature describes the mosaic nature of emerging pathogenetic factors in the obstruction of the outflow of venous blood from the skull. At the same time, the leading place in the genesis of dynamic disorders of venous circulation belongs to myofascial pain syndrome of cervical localization. When myofascial pain syndrome is localized in the muscles of the craniovertebral junction, congestive venous disorders are caused by general algic processes in this zone, including functional blockades of the junction, while tunnel-compression mechanisms in this zone do not play a decisive role in venous discirculation. Tunnel-compression mechanisms of obstruction of venous blood flow are most relevant in the middle and lower cervical localization of myofascial pain.
Conclusion
Taking into account our data on the strong correlation between accelerated venous blood flow and tortuosity of the ICA, VA (as indirect manifestations of disorders in the cervical spine, including manifestations of natal trauma to the cervical spine), we believe that in children and adolescents a key role in The appearance of dysgemia (impaired venous outflow) is played by the “pathology/structural features” of the cervical spine and the congenital structural features of the ICA at the extracranial level. The main causes of dysgemia in childhood should be considered “congenital connective tissue dysplasia” [19], manifested in the form of pathology of the cervical spine, with curvature and tortuosity of the bone canal, or “birth injuries with subluxation of 1-2 cervical vertebrae” (presence of a history of in the majority of examined individuals), with impaired venous outflow at the extracranial level.
Taking into account all of the above, it should also be concluded that if a picture of venous discirculation is identified, especially in young people, treatment should be aimed primarily at restoring the functional integrity of the musculoskeletal system of the cervical spine, correcting posture, manual practices, as well as compliance with regime-restrictive measures [20].
Literature
- Lelyuk V.G., Lelyuk S.E. Ultrasound angiology. M.: Real Time, 2003. 322 p.
- Valdueza JM, Schmierer K., Mehraein S., Einhäupl KM Assessment of normal flow velocity in basal cerebral veins. A transcranial Doppler ultrasound study. 1996. Stroke 27. pp. 1221-1225.
- Schoser BG, Riemenschneider N., Hansen HC The impact of raised intracranial pressure on cerebral venous hemodynamics: a prospective venous transcranial Doppler ultrasonography study // J. Neurosurg. 1999. V. 91, N 5. P. 744-749.
- Stolz E., Jauss M., Horning C. Cerebral venous anatomy in color-coded duplex sonography. What is possible in non-contrast enhanced TCCD? // New trends in cerebral haemodynamics and neurosonology / Eds. Kligelhofer J., Bartels E., Riglenshtein B. 1997. P. 312-319.
- Baumgartner RW, Gonner F., Muri R. Normal haemodynamics in cerebral veins and sinuses: a transcranial color-coded duplex sonography study // New trends in cerebral haemodynamics and neurosonology / Eds. Kligelhofer J., Bartels E., Riglenshtein B. 1997. P. 312-319.
- Aaslid R. Cerebral hemodynamics // Transcranial Doppler / Eds. Newell DW, Aaslid R.: - NY: Raven, 1992. R. 500.
- Shakhnovich V.A. Violation of the venous circulation of the brain according to transcranial Dopplerography // Ultrasound Doppler diagnostics of vascular diseases / Ed. ed. Nikitina Yu.M., Trukhanova A.I. M.: Vidar, 1998. pp. 355-400.
- Dicheskul M.L., Kulikov V.P., Maslova I.V. Ultrasound characteristics of venous outflow through the vertebral veins / Ultrasound and functional diagnostics, 2008, N 4. P. 33-40.
- Ivanichev G.A., Dolgikh G.B. Disturbances of arterial and venous blood flow in children with vertebrobasilar insufficiency // Journal of Neurology and Psychiatry, 2007, N 3.
- Dolgikh G.B., Ivanichev G.A. Cerebral vascular disorders in children with cerebral palsy and convulsive syndrome // Kazan Medical Journal, 2008, N 3.
- Pucillo M.V., Vinokurov A.G., Belov A.I. Atlas “Neurosurgical Anatomy” / Ed. Konovalova A.N. M.: Antidor, 2002.
- Burtsev E.M., Andreev A.V., Dyakonova E.N., Kutin V.A. Functional Dopplerography in pediatric angioneurology // Abstracts of the report at the VIII International Conference: Current state of non-invasive diagnostic methods in medicine. Sochi, 2001. pp. 151-160.
- Nikitin Yu.M., Trukhanov A.I. Ultrasound Doppler diagnostics in the clinic. MIC, 2004. 496 p.
- Adelson PD, Bratton SL, Carney NA et al. Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents. Pediatr. Crit. Care Med. 2003; (4) 3.
- Samuel M., Burge DM, Marchbanks RJ Tympanic membrane displacement testing in regular assessment of intracranial pressure in eight children with shunted hydrocephalus // J. Neurosurg. 1998. V. 88. R. 983-995.
- Bode H. Pediatric application of transcranial Doppler sonography / Wien; Ny: Springer Verlag, 1988. P. 108.
- Rosin Yu.A. Dopplerography of cerebral vessels in children / SPbMAPO, 2006. 114 p.
- Belkin A.A., Alasheev A.M., Inyushkin S.N. Transcranial Dopplerography in intensive care. Methodological manual for doctors. Ekaterinburg: Publication of the Clinical Institute of the Brain of the Scientific Research Center of the Russian Academy of Medical Sciences; 2004.
- Andreev A.V., Lobanova L.V., Ermolin I.E. Transcranial Dopplerography and variational pulsometry in the diagnosis of cerebral angiodystonia in children // Journal of Neuropathology and Psychiatry. 1994. N 3. S. 22-23.
- Tsokolov AV, Tsokolova VA, Tsokolova MA, Senchilo VG, Egorov AU Venous discirculation // Journal of the Neurological Sciences. 333 (2013). e518. Abstract - WCN 2013, No102, Topic:8 - Headache. Vienne, Austria. 2013. Neurology in the age of globalization. XXI World Congress of Neurology.
Ultrasound scanner HS70
Accurate and confident diagnosis.
Multifunctional ultrasound system for conducting studies with expert diagnostic accuracy.
Three stages of pathology
Venous discirculation develops in 3 stages:
- The first is that symptoms do not appear.
- Secondly, the signs are present, but although they worsen the quality of life, they do not exclude the ability to work and the ability to self-care.
- Third, the symptoms are so strong that they provoke severe complications in the brain and throughout the body. The patient can no longer work. Over time, he cannot take care of himself; he requires constant care from other people.
The disease is insidious in that it does not manifest itself at the first stage, and when the symptoms begin to make themselves felt, the changes are sometimes irreversible. And at the second stage, you can only prevent the disease from moving into the third – the most severe phase. You can also completely alleviate the disturbing symptoms, but it is unlikely that you will be able to get rid of the pathological changes that have occurred in the brain 100 percent.
Exercises to help improve venous drainage
During circulatory problems, physical exercise often helps. They must be performed three times a day, for 10 minutes.
Exercise 1 - head tilt, execution steps:
- You need to sit down on a chair.
- Relax your muscles.
- Throw your head back.
- Maintain deep and even breathing.
Duration of execution – up to 2 minutes.
Exercise 2 - long neck, performed as follows:
- You need to take a sitting position.
- The muscles need to be relaxed and the head tilted towards the chest.
- The head rises as high as possible during inhalation.
- As you exhale, it lowers again.
Performed up to 10-15 times.
Exercise 3. Drawing eights. You need to make movements with your head, similar to the image of the number 8, while breathing moderately and relaxing your body. Perform the exercise several times, and your eyes must be closed.
Exercise 4 - power tilt, performed as follows:
- A sitting position is assumed.
- Fingers should be crossed near the base of the chin.
- As you exhale, you need to tilt your head and apply pressure with your hands.
- When inhaling, you need to tilt your head back.
Do it 3 times.
Treatment methods
- First of all, doctors will try to rid you of the underlying disease. For this, various drugs may be prescribed (ACE inhibitors for hypertension, glycosides for heart failure, etc.) or surgery may be performed (for example, to remove a tumor compressing a vein).
- To improve the outflow of venous blood, you will be prescribed a venotonic. Examples of drugs in this group: Venoplant, Detralex, Aescusan, Anavenol.
- To thin the blood and prevent thrombosis, one of the medications based on acetylsalicylic acid will be prescribed: Aspirin, Aspirin Cardio, ThromboASS, Cardiomagnyl.
- To strengthen the vascular walls, doctors prescribe a course of treatment with Pyridoxine to their patients.
- To relieve cognitive symptoms, such as poor memory, emotional instability, difficulties in thinking, nootropics are used: Glycine, Phenibut, Phenotropil.
Phytotherapy
When a child has venous dysgemia in the area of the spinal plexuses, the doctor prescribes healing baths. Viburnum berries, sage herbs, chamomile or elderberry are added to the water.
Other recommendations
The baby, when he realizes what is happening to him, needs to be taught to lead an active lifestyle. The harm of certain habits must be explained to him so that he understands that they are dangerous to his life. The child should be taught to play sports.
Running and long walks help overcome venous dysgemia. It is useful to introduce a teenager to yoga. But as the disease progresses, medical consultation is required to help optimize the expected physical activity. It is better not to visit the sauna, since a sharp change in temperature, despite the stimulation of blood flow, negatively affects blood vessels that are weakened by the disease.
Diagnostics
It is impossible to prescribe the correct treatment for a patient without conducting a full examination to identify the main causes that provoked the appearance of the pathology. Nowadays, many methods have been developed, there is modern equipment that allows you to almost accurately determine that a child has venous dysgemia. The most effective method is Doppler ultrasound (USD).
It is usually quite difficult to immediately make an accurate diagnosis. Parents should first visit a neurologist, especially when the baby is constantly crying or has nervous behavior.
Even after clarifying the nature of the disease, it is still not easy to develop precise treatment tactics that would eliminate not the pathology itself, but at least its main symptoms. Because of this, doctors hesitate to make a diagnosis, because the problem that has arisen is a consequence of a certain disease that must be eliminated first of all.
Forecast
If the symptoms of venous discirculation pathology are already pronounced, the prognosis is not very favorable. There is a high probability that the disease will progress further. The risk of stroke is also increased.
However, if you follow all the doctor’s recommendations regarding the treatment of the underlying disease and symptomatic treatment of cerebral venous circulation, you can almost completely get rid of unpleasant manifestations and delay the progression of the disease until old age.
If you identify the disease at an early stage, when it is still hidden (this is why preventive annual visits to a neurologist are needed), then you can prevent even the appearance of the first symptoms.
Classification
There are 3 stages of the disease:
| Stage | Characteristic |
| Latent | The pathology has a latent form, and there are almost no symptoms |
| Cerebral | The stage has non-dangerous symptoms |
| Venous | Accompanied by organic microsymptoms. The condition requires the help of doctors because it threatens the patient’s life |
It is also customary to classify pathology according to Berdichevsky:
- Primary stage. Vascular tone is altered, which leads to impaired blood flow in the brain.
- Stagnant stage. Mechanical obstructions to cerebral circulation are noted.
Prevention
To prevent circulatory problems in the brain:
- Get rid of bad habits.
- Avoid stress, overexertion, and overtime.
- Eat right.
- Do not subject your body to excessive physical activity, but also do not lead a sedentary lifestyle.
- Treat chronic diseases in a timely manner, especially for cervical osteochondrosis, which people often do not give due importance. If your neck hurts, immediately go to a neurologist.
- Monitor your blood pressure, especially if you are over 40. Buy an automatic electronic blood pressure monitor and measure your blood pressure 2 times a day. This will take at most 5 minutes a day, but in this way you will eliminate hypertension and hypotension. If you notice that your blood pressure changes, immediately go to a therapist, and then to a cardiologist.
- Once every six months to a year, undergo a preventive examination with a therapist, cardiologist, or neurologist.
Characteristic symptoms
Signs of venous discirculation begin to appear at stage 2.
| Pathology can be recognized by the following symptoms | When the headache gets worse |
| Headache (dull, bursting) | In the morning, especially if you haven't gotten enough sleep |
| Weakness, fatigue, difficulty getting up in the morning | When you take a horizontal position or tilt your head down |
| Swelling of the lower eyelid, bags under the eyes | When you turn your head many times |
| Noise, ringing in the ears | When performing complex movements that require good coordination |
| Dizziness, fainting | When you exercise |
| Periodic numbness of the limbs | When there is a sudden change in weather |
| Blue tint to the tip of the nose, lips, cheeks | When you're nervous |
Closer to the third stage, the following signs are added to the listed characteristics:
- Disorders of coordination, memory, speech, thinking, psyche.
- The patient's gait is disturbed and he cannot perform precise movements, for example, touching his nose with his eyes closed.
- He becomes forgetful, whiny, irritable.
- May begin to speak less clearly.
- Intellectual abilities decrease.
- The frequency of numbness in the extremities also increases. This can eventually lead to paralysis.
- Epileptic seizures may also develop.
Ultimately, all this leads to a condition similar to the consequences of a stroke. At a very late and advanced stage of venous discirculation, the patient becomes disabled. Also, the disease at the third stage can lead to a stroke, which will further aggravate the severity of the patient’s condition.