Testicular varicose veins, or varicoceles, are a problem that many men face. Often the disease occurs in adolescence and is detected during a urological examination. According to statistics, 5-7% of young people aged 18-20 years and 15-17% of men under 40 suffer from varicocele. In 80-98% of cases, left-sided varicose veins are observed.
Varicocele is characterized by a hidden course and does not manifest itself for a long time. It is possible to detect the disease in its early stages only with the help of special tests. The Valsalva maneuver for varicocele helps to visualize pathologically dilated veins. What is this research and what are its benefits?
Presentation. Text version.
Duplex ultrasonography today is the most commonly used method for studying the venous system in chronic venous diseases (CVD) of the lower extremities.
Using duplex ultrasound, indications are determined and the results of various types of treatment are assessed. However, there is still no consensus on how best to perform this test in this patient population. Based on our own many years of experience (from 1989 to the present) in the use of various types of ultrasound examinations in the examination of many thousands of our patients, data from domestic and foreign colleagues, and analysis of world literature, we tried to generalize and optimize the existing recommendations for conducting ultrasound examinations of patients with various forms of chronic venous disease
The purpose of duplex ultrasound examination in patients with chronic venous disease:
- Obtain the most complete anatomical and physiological characteristics of the studied segment of the venous system;
- Comprehensively examine existing anomalies of venous blood flow.
The following must be installed:
- which connections of the main saphenous veins are insolvent, determine their location and diameter;
- degree of reflux in the saphenous veins of the thigh and leg;
- number, location, diameter and functioning of incompetent perforating veins;
- other relevant veins with reflux;
- source of filling superficial varicose veins;
- veins that are hypoplastic, atretic, absent or removed;
- the condition of the deep vein system, including the consistency of the valves and the presence of previous venous thrombosis.
Most patients who undergo duplex scanning to examine superficial veins, deep veins, and perforators are considered potential patients. The information obtained allows you to decide whether treatment is necessary and to what extent. Patients with incompetent sapheno-femoral (SPS) or sapheno-popliteal (SPS) junctions may require surgery, duplex ultrasound-guided sclerotherapy, or an endovenous procedure (radiofrequency obliteration, endovenous laser coagulation). Patients with isolated saphenous vein tributary incompetence can undergo phlebectomy and sclerotherapy. Inaccurate identification of all sources of hypertension and areas of hypervolemia leads to inadequate treatment with subsequent early relapses of varicose veins.
Causes of varicocele.
There are congenital and acquired causes that contribute to varicocele.
Congenital diseases include: duplication of the testicular vein, ring-shaped structure of the left renal vein, congenital pathologies of the valvular apparatus of the testicular vein, congenital stenosis of the renal vein, high growth.
Acquired: increased intra-abdominal pressure (jogging, weightlifting, chronic constipation), compression of the testicular vein by large vessels. These conditions lead to increased pressure in the renal vein and, secondarily, in the testicular vein, since venous pressure is hydrostatic pressure, that is, the pressure of a column of fluid.
Duplex scanning.
Since venous reflux usually occurs in both lower extremities, it is recommended to examine them both, even if clinical signs of the disease are present in one.
Whether all patients require scanning is a controversial issue. However, with the isolated use of a small-sized Doppler device (continuous wave) or without it, up to 30% of incompetent sapheno-femoral or sapheno-popliteal junctions can be missed and complete and adequate information about the transformed veins may not be obtained. Today, there is no doubt about the extremely low information content of an independent Doppler study in assessing the viability of the communicating veins.
Of course, duplex scanning is very important to perform before treatment to determine whether there is insufficiency of the SPS or SPS, register its level and determine the anatomical features, for example, the common entry of the SPV with the gastrocnemius veins into the popliteal vein.
Veins filled with reflux from the pelvic/perineal veins should be visualized; varicose veins not connected to the large or small saphenous vein. Isolated lateral varicose veins of the thigh should be assessed, ensuring that there are no indications for intervention on the main veins.
Duplex scanning is of fundamental importance for determining the characteristics of the anatomical bed and hemodynamics of recurrent varicose veins. A comprehensive assessment of the adequacy of the surgical or endovenous intervention performed on the patient allows us to develop subsequent treatment tactics that meet the pathophysiological requirements. Duplex scanning also makes it possible to determine the degree of involvement of the deep vein system in the disease, predict the likely outcome after isolated treatment of pathologically altered areas of the superficial veins, and select patients in need of reconstructive interventions on the deep veins.
Duplex ultrasonography provides comprehensive information about anatomical variations and the causes of development of various vascular malformations. The possibility of its unlimited implementation provides dynamic control over the quality of surgical correction or staged sclerotherapy.
For good image quality of superficial veins, in most cases, a high-frequency transducer with a linear sensor of 7.5-13 MHz is optimal. For very large or swollen limbs, you can use a transducer with a 3.5-5 MHz convex sensor.
Superficial veins usually lie at a depth of 2-3 cm from the skin. It is important to set the optimal settings for the focal zone of the sensor in order to obtain the best image of the vein being examined in B-mode. The dynamic gain control should be set to optimize the image:
- the lumen of the vein should be dark in the absence of acute thrombosis or postthrombotic obstruction;
- the spontaneous echogenicity of the blood flow should be visualized with the ability to register the echo signal from a thrombus in the lumen of the vessel.
To optimize the system for assessing low flow rates observed in veins, it is recommended to use “low flow”.
Recommended settings:
- Doppler sensitivity range is within 5-10cm/s;
- Doppler filter – at the lowest level.
It is best to increase the "doppler gain" so that there is little "noise" in the color or pulse Doppler scale to ensure maximum system sensitivity. In patients with strong venous flow, Doppler range should be increased and color gain reduced to avoid color artifacts. We typically use blue to represent orthograde venous flow to the heart in color mode, and red to represent retrograde flow (venous reflux).
To standardize measurements of vein diameter and reflux, it is recommended to conduct the study with the patient standing. The horizontal position is not for determining reflux and measuring vein diameters is not informative. The examination of the calf veins is carried out while the limb being examined is supported on a low stand (often the edge of the researcher’s chair can also serve as this).
When duplex ultrasound scanning of the veins of the lower extremities, it is necessary to use a combination of transverse and longitudinal visualization. Transverse scanning provides more accurate general information about the morphology and possible presence of an endolaminar thrombus due to compression, allowing, among other things, a more subtle assessment of the functional usefulness of the valve structures (the form of closure of the leaflets). Longitudinal scanning more fully assesses orthograde blood flow and reflux.
To obtain optimal color or spectral Doppler signal, an insonation angle of 45-60 degrees between the transducer and the vein should be used.
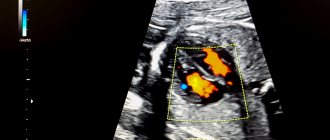
Ultrasound for varicocele.
In the practice of a urologist-andrologist, ultrasound ranks first in the diagnosis of varicocele and has become the “gold standard”.
Modern linear high-frequency sensors are used. To assess the anatomy, a “gray scale” is used (the doctor sees all structures on the screen in black - gray - white). With this technique, tubular structures are identified in the projection of the inguinal canal and scrotum. These are the veins. The diameter of the veins is measured. Normally, the diameter of the vein should not exceed 2 millimeters and the course of the veins should be straight. With varicocele, in the projection of the inguinal canal and scrotum, a conglomerate of intertwined convoluted tubular structures is found, which seem to hang on other elements of the spermatic cord.
When studying the function of veins, additional techniques are used.
The color Doppler mapping (CDC) method helps to evaluate the functioning of the valve apparatus of the veins and speed indicators, as well as the time of blood movement in the vessel. Normally, venous outflow, that is, the work of the veins is synchronized with the act of breathing and the movements of the diaphragm. After inhalation, in the first second, the venous valves close and the movement of blood in the veins slows down and the speed of venous blood flow is zero. As you exhale, the diaphragm muscles contract and intrathoracic pressure increases. Due to these mechanisms, blood is attracted to the heart. The CDC technique clearly illustrates the reflux phase on the screen, making it possible to diagnose varicocele.
Reflux research.
Venous reflux is defined as retrograde blood flow in the opposite direction to physiological blood flow, lasting more than 0.5 seconds, although there is no agreement (in the published literature) regarding its duration for all venous segments.
There are several methods to detect reflux:
- for proximal veins, compression of the calf and cessation of compression;
- for the calf veins – compression of the foot;
- rapid deflation from a pneumatic cuff on the calf;
- active dorsiflexion of the foot and subsequent relaxation;
- Valsalva maneuver - this method is preferable, according to many authors, when it is necessary to demonstrate the failure of the saphenofemoral junction
Venous reflux is identified by obtaining an image of the vein of interest and applying compression to the limb using one of the described methods. The compression is abruptly stopped and the presence and duration of reflux is observed. Cuff deflation is used to quantify reflux. This is the most reproducible method, although some consider it technically more difficult.
Method of performing the Valsalva maneuver
The Valsalva maneuver is widely used in the diagnosis of varicocele in the early stages, when there are no pronounced clinical symptoms yet. The technique is used as an independent method of examination or in combination with ultrasound.
In patients with suspected varicocele, the Valsalva maneuver is performed at the first examination. The man takes a deep breath and holds his breath. At this time, the urologist palpates the scrotum and testicles. In the presence of pathological changes, even slight dilation of the veins becomes noticeable.
To assess blood flow in the affected vessels, the Valsalva maneuver is also performed during ultrasound. The specialist asks the man to take a deep breath and strongly tense his abdominal muscles. Signs of the disease are expansion of the spermatic cords and the appearance of elastic nodules.
Our clinic invites you to undergo diagnostics and surgical treatment of varicocele. The medical facility is equipped with the necessary equipment, and consultations are conducted by experienced urologists-andrologists. Sign up for consultations by phone.
Preparing the patient.
The patient should be examined in a well-lit room. The lower extremities are examined generally for the presence of varicose veins and the presence of postoperative scars to clinically determine the source of reflux and facilitate further examination. The patient must be explained what will be done, especially with regard to the Valsalva maneuver. There is no doubt about the extremely low information content of the so-called functional tests. We fundamentally believe that time should not be wasted on doing the latter, even from an educational point of view.
The room should be at normal room temperature. An excessively warm environment promotes dilatation of the veins, while a cool environment can cause their spasm, which, as a rule, makes visualization difficult, and contributes to the disappearance of borderline venous reflux. The patient needs to relax the limb being examined during the examination to create favorable conditions for good filling of the calf veins.
Scanning of the great saphenous vein (GSV), deep veins above the knee and thigh perforators.
The patient should stand facing the doctor, turn his leg outward, heels pressed to the floor, and shift his weight to the opposite limb. To identify the GSV and the common femoral vein, it is necessary to scan the area of the inguinal fold in the transverse position of the sensor. Both of these veins lie medial to the common femoral artery. A convenient technique with the figurative name “Mickey Mouse”. After removal of the GSV, the integrity of the safenfemoral junction is compromised—Mickey's medial ear is missing in the image.
In the area of the SPS, several veins (tributaries of the GSV) and two valves of the great saphenous vein (terminal and preterminal) are usually visualized. It is very important to evaluate these tributaries and valves, as different hemodynamic options are possible. It is critical to identify suspected sources of reflux, including incompetent SPS, incompetent lower abdominal and pelvic veins, femoral perforators, or the vein of Giacomini.
In the transverse image, you should determine whether the reflux is directional:
- in the GSV within the saphenous vein system;
- into the additional anterior saphenous vein, which lies lateral to the GSV and is usually connected to the deep veins in the lower thigh;
- into the main femoral tributaries, located superficially relative to the subcutaneous fascia.
Scanning should be continued along the entire length of the GSV and along its tributaries to the ankle. The vein lies between two layers of fascia, which is quite easily identified on an ultrasound scan in B-mode (real time). This image is known by its appearance as a “subcutaneous eye.” It is necessary to examine every centimeter of the length of the vein for compressibility and reflux. If there is reflux, then it is necessary to measure the diameters in the area of the SPS and along the entire GSV. Another significant area of examination is the mid-thigh and knee area. It is necessary to scan the trunk of the GSV, and not any other varicose segment with an incompetent valve. Measuring the diameter can help decide which treatment method to use. An indicator such as the depth of the GSV trunk under the skin is also important, especially in patients who are planning to undergo radiofrequency or laser obliteration. These measurements can be used as a baseline for monitoring after endovenous procedures.
Spermogram
Varicocele in an advanced state can cause infertility, so one of the diagnostic methods is semen analysis. A spermogram allows you to determine the degree of varicocele and other abnormalities. During the analysis, the following indicators are recorded:
- Volume, color, consistency, presence of blood cells.
- The period of liquefaction of the material to determine the presence of an inflammatory process.
- The number of active sperm (in a healthy man there is at least half of them).
- The presence of pathological forms or glued spermatozoa (indicates problems of the immune system).
Before taking the test, it is important:
- Observe sexual rest for 3 - 7 days.
- Avoid drinking alcohol.
- For 10 days, avoid visiting saunas and baths.
The material is collected in a special container in the clinic, and not at home, because transportation to the laboratory should not exceed 60 minutes. We must not forget about the rules of hygiene - it is important to wash your hands thoroughly before masturbation.
Deep veins of the thigh.
After identification during transverse scanning, the common femoral vein (CFV) should subsequently be examined longitudinally to determine the phasicity of the flow during normal breathing.
Tests to be performed:
- with deep breathing - normally the blood flow stops;
- Valsalva maneuver or manual compression of the thigh (calf) to check for reflux.
It is best to perform these tests with the patient in a standing position. Some authors prefer the position of the patient lying on his back.
When continuous blood flow is determined in the PVB, we always mean the presence of proximal obstruction or post-thrombotic changes in the vein. In this case, it is recommended to extend duplex scanning to the iliac veins and the inferior vena cava. The VV should be examined above and below the saphenofemoral junction, because as soon as retrograde flow distal to this level represents true deep vein reflux. In any case, it is necessary to trace the entire length of the femoral vein to the popliteal vein.
Antonio Maria Valsalva was a distinguished anatomist, physiologist and professor of surgery at the University of Bologna. In 1704, he published his most famous work, De Aure Humana Tractatus, which served as a reference for the treatment of middle ear diseases for more than a century. In several paragraphs of his book, A. M. Valsalva described in detail a therapeutic technique “for pushing foreign bodies and fluids out of the middle ear,” in which the patient attempted to exhale for several seconds with his mouth and nose closed. Many years later (1851) in Germany, the physiologist Edward Weber detailed the changes in the cardiovascular system associated with this technique, allowing it to be used to determine the autonomic (autonomic) regulation of the heart. Historically, giving due credit to both authors, in world literature sources this technique is often called the Valsalva-Weber maneuver (VW) [1].
The test makes it possible to quantitatively and comprehensively assess the contribution of the sympathetic and parasympathetic parts of the autonomic nervous system (ANS) to the regulation of the functions of the heart and blood vessels [2].
The role of autonomic disorders in the origin of vasovagal syncope (VVO) is widely discussed. The possibilities of using PVV in patients with VZV have not been studied, which determined the relevance of this study.
Materials and methods
The study included 12 healthy individuals (all men, mean age 31±7 years) and 30 patients with VZV (12 (40%) men, mean age 32±14 years). The patients had significantly lower height and body weight compared to the group of healthy individuals, probably due to the predominance of men in the latter group. The vasovagal genesis of fainting in patients in all cases was confirmed by clinical survey data using a specially developed questionnaire [3]. At the same time, other (metabolic, neurological, cardiac and orthostatic) causes of attacks of loss of consciousness are excluded by the results of a preliminary instrumental examination.
The patients also did not have clinically significant diseases of a somatic, endocrine, neuropsychic nature or were taking medications.
All individuals included in the study underwent PVV. The test was carried out using a specialized complex Task Force Monitor (“CNSystem”, Austria), which made it possible to synchronously monitor the electrocardiogram (ECG) and heart rate (HR) - RR
non-invasively, in a “beat-to-beat” mode, monitor blood pressure (BP) on the fingers of the right hand using the photocompensation method (based on changes in pulse blood supply) in combination with periodic calibration of the signal taking into account blood pressure measured by the oscillometric method on the left shoulder.
Initially, the patient was at rest, lying on his back, for 20 minutes, the initial parameters were recorded.
At this time, the test procedure was explained to the subject and the Valsalva maneuver was taught, including a short trial of performing it. Then PVV was performed in accordance with the recommendations of P. Novak [2].
When performing the test, the subject took a mouthpiece into his mouth (a disposable plastic syringe with a capacity of 10 ml, to the connector for the needle of which the inlet hose of the pressure gauge was connected; at a distance of 10 mm from this place, 4 holes were made in the body of the syringe with a needle No. 0740 to ensure a small leak of air during forced exhalation , which prevented “incorrect” performance of the test by a patient with a closed glottis). The patient took a deep breath and then exhaled forcefully into the mouthpiece. Based on the readings of a pressure gauge connected to the mouthpiece, he maintained a pressure of 40 mm Hg. within 15 s. Then the subject released the mouthpiece and took a normal breath. To facilitate the test, a special nose clip was used.
The test was repeated three times with a 3-minute interval between tests. For subsequent calculations, one of the tests with the minimum number of artifacts in blood pressure and heart rate trends was selected. For in-depth processing of the study results and calculation of additional indicators, data from trends in blood pressure and heart rate were exported into Excel spreadsheets, followed by calculation using the capabilities of the Excel program.
Analysis of the results of PPV to identify ANS disorders and determine the degree of their severity included a visual assessment of the curves of changes in blood pressure and heart rate, as well as the calculation of parameters that are currently used by leading laboratories involved in the diagnosis and treatment of ANS pathology [2, 4-6]. A complete list of such indicators is given in table. 1
, and a schematic representation of the sample phases is in
Fig.
1 .
Figure 1. Dynamics of mean blood pressure and RR
during PPV in a healthy volunteer. Explanations in the text.
Statistical processing and analysis of the obtained data was carried out using nonparametric methods. To assess intergroup comparisons of indicators, the Mann-Whitney test was used, and to study the reliability of changes in indicators in each of the study groups during the tests, the Wilcoxon method was used. To estimate the frequencies of qualitative characteristics, Fisher's nonparametric method was used. All differences were considered significant at p
<0,05.
Results and discussion
When analyzing changes in indicators of the cardiovascular system function during PVV, 4 phases are distinguished (see Fig. 1; Fig. 2)
[1, 2, 4-7].
Figure 2. Dynamics of mean blood pressure and RR
during PPV in a patient with VZV.
MAP in late phase II does not reach the initial level (for the normal version of the reaction for comparison, see Fig. 1). In phase I, when the subject takes an intense breath and begins expiratory effort, an increase in blood pressure is observed due to the increased ejection of blood from the heart, while a slight decrease in heart rate may be observed (an increase in the duration of the R-R
).
Phase II corresponds in time to expiratory tension and is characterized by a rapid initial decrease in blood pressure (early period). This is caused by a decrease in venous blood return and cardiac output against the background of high intrathoracic pressure, and then a gradual increase in blood pressure, often exceeding its initial level (late period), under the influence of compensatory baroreflex mechanisms. The result is excitation of the sympathetic part of the ANS and vasoconstriction, as well as a weakening of vagal influences and sinus tachycardia (decreased duration of R-R
). However, if immediately before the test the subject made deep breathing movements, then in phase II bradycardia may be observed, associated with the increased action of the vagus nerve [7]. A sudden cessation of expiratory effort 15 s from the start of the test leads to a drop in intrathoracic pressure and blood pressure (phase III). Subsequently, with the resumption of respiratory movements, the return of venous blood to the heart increases and, against the background of a persisting increased level of vasoconstriction (as a result of sympathetic activation in phase II), a rise in blood pressure is observed, exceeding its initial level (“overshoot”), and heart rate slows down.
If the compensatory physiological mechanisms for regulating blood pressure and heart rate are insufficient, the described phasing when performing PVV may be disrupted, and the reactions of hemodynamic parameters may be distorted, which is observed in various pathologies of the ANS.
Analysis of parameters characterizing various phases of PWV (see Table 1)
, did not reveal significant differences between healthy individuals and patients with VZV for most of them, with the exception of the “2” pressure index on the test
(see Table 1; Table 2)
.
In patients with VZV, the value of index “2” (i.e., the increase in blood pressure in the “late period” of phase II) on average for the group turned out to be less than in healthy individuals (see Fig. 1, 2)
.
During visual analysis, a significant change in the shape of the mean blood pressure curve, consisting in the fact that by the end of phase II of the test, blood pressure did not reach the initial level, was recorded in 10 out of 30 patients with VZV (i.e., 33%) (see Fig. 2)
, and not a single healthy person.
The differences in the frequency of detection of this phenomenon between the two groups are significant (see Table 2)
.
The indices we analyzed are used to identify damage to the sympathetic part of the ANS and the degree of its severity [4]. The magnitude of the decrease in average blood pressure (index “1”), the possibility of restoring this indicator by the end of phase II of PPV (index “2”), the residual value necessary to achieve its initial level (index “3”) are accepted as quantitative and qualitative criteria "sympathetic deficiency" assessments. According to the results of the study by P. Novak [4], the index “3” of all the studied indicators in the analysis of PVV was optimal for assessing the sympathetic link of blood pressure regulation, since it made it possible to clearly distinguish healthy individuals from patients with “sympathetic insufficiency” and was associated with orthostatic hypotension , as well as the degree of its severity.
In our work on index “3”, no significant differences were found between patients with VZV and healthy individuals. This may be due to the fact that, unlike the study by P. Novak, in our study the patients had no signs of classical orthostatic hypotension (decrease in systolic blood pressure >20 mm Hg) during an active orthostatic test.
There are differences of opinion regarding the presence of autonomic pathology in patients with VZV. It is believed that people susceptible to VZV do not have true damage to the ANS when using traditional criteria for assessing its function, and the existing symptoms are explained in terms of a hyperbolically expressed reflex response, leading to bradycardia and arterial hypotension [8]. At the same time, a number of clinical and experimental works [9-15] show that using other methods for assessing the regulatory capabilities of the ANS (analysis of heart rate variability indicators, microneurographic study of the sympathetic activity of the peroneal muscles, impedance cardiography, myocardial scintigraphy with metaiodobenzylguanidine labeled with radioactive iodine ) signs may be revealed that indicate an insufficient contribution of the sympathetic component to the regulation of the activity of the heart and blood vessels.
To truly judge the severity of damage to the ANS, a comprehensive analysis of the functioning of its two parts is necessary - sympathetic and parasympathetic. According to the results of our work, between patients with VZV and healthy individuals in parameters characterizing the “vagal” regulation of the heart (sensitivity of the arterial baroreflex, Valsalva ratio - see Table 1
), no significant intergroup differences were obtained.
At the same time, in 9 (30%) of 30 patients, an individual analysis of the Valsalva ratio adjusted for gender and age [2] revealed its decrease (see Table 2)
. The results obtained in this work differ from the literature data [13, 15], which indicate the preservation of “vagal” influences on the sinus node in patients with VZV and even their intensification both in the resting position, lying down, and especially with the development of syncope. The reason for such differences may be both the methodological features of assessing the function of the ANS (analysis of heart rate variability) used in these studies, and the factors involved in the formation of different samples of patients.
To identify autonomic disorders, an integrated approach is usually used - several tests are performed (deep breathing test, Valsalva maneuver, test with active or passive orthostasis and sudomotor test), and when determining the severity of the detected pathology, it is customary to use special scales. PVV is the only one of those listed, the evaluation of the results of which allows us to draw a conclusion about possible disorders in both the sympathetic and parasympathetic parts of the ANS.
In general, in 16 (53%) of 30 patients with VZV, signs of autonomic disorders were identified either in the sympathetic (altered shape of the BP mean curve) or in the parasympathetic (individually altered Valsalva ratio) part of the ANS. The coincidence in the involvement of both parts in the process was stated in 3 cases. Using scales for assessing the degree of autonomic failure [2], the identified disorders in the patients included in this study can be assessed as mild.
Conclusion
When performing dosed PVV, signs of sympathetic insufficiency (impaired adrenergic regulation of blood pressure) are detected in 33% of patients with VZV, and parasympathetic insufficiency (impaired “vagal” regulation of cardiochronotropic function) - in 30%.
Femoral perforators.
It is recommended to consider perforators in the medial thigh during examination of the GSV and deep veins. Not all femoral perforators, successful or incompetent, will be identified. They are usually visible in the middle and lower third of the scanned area, but they can also be verified in the proximal part of the thigh near the saphenofemoral junction. If clinical examination reveals the presence of varicose veins in these areas, it is necessary to look for lateral and posterior femoral perforators.
Spectral and/or color Doppler should be used to examine internal and external flow (inward flow and inward flow) in perforators through contraction of the calf or thigh muscles. Perforators providing blood flow in two directions are probably abnormal (pathological), although the same findings occur in some patients without clinical manifestations of varicose veins. If an incompetent femoral perforator is identified, it is advisable to record its diameter, which is measured at the muscular fascia, and its location relative to the knee joint, in order to then decide on the best method of treatment.
Ultrasound of the scrotum, genitourinary system
An ultrasound examination is performed first in a lying position, then standing. A change in posture is necessary to determine the speed of blood flow. Thanks to ultrasound, the doctor can obtain complete information about the disorder and determine the extent of the spread of the varicocele and examine the consistency of the tissues.
Normal ultrasound readings:
- The diameter of the testicular vein is no more than 2 mm.
- The speed of venous blood in the testicular vein is up to 10 cm/s.
- There is no venous reflux.
If the diameter of the vein is increased, a varicocele is diagnosed. Ultrasound is considered one of the most informative and accurate methods for diagnosing pathology. The procedure can be performed in conjunction with Doppler ultrasound, which examines the volume of blood flow in the vessels of the scrotum and its speed. Dopplerography can detect valve disorders in the veins.
To determine varicocele and the degree of venous dilation of the veins, there are various diagnostic methods that are safe for the patient’s health. After passing the examination, the doctor can accurately determine the presence of pathology and choose the most appropriate treatment method.
Popliteal vein scan.
The popliteal fossa is a difficult place to study, both from an anatomical point of view and from the point of view of assessing venous hemodynamics. A lot of longitudinal and cross-sectional studies are always required in this area. Typically, the veins of this zone are scanned by placing the patient face down, when it is necessary to determine the synchronicity (phase) of blood flow with breathing, although in some patients, again, phasing is not observed even in the absence of pathology. Typically, increased blood flow is determined by squeezing the calf, because The Valsalva maneuver has limited value at this level. The popliteal vein should be examined above and below the saphenopopliteal junction, as at other levels, due to the fact that only retrograde blood flow detected distal to this site represents true deep vein reflux. It is necessary to establish the anatomical and hemodynamic relationship of the popliteal vein, sapheno-popliteal junction and musculovenous sinuses of the gastrocnemius and soleus muscles.
Historical reference
Today, the Valsalva maneuver for varicocele is used to assess the increase in the venous network of the spermatic cord when holding the breath and straining. A similar technique with minor modifications was used more than 100 years ago, but for a different purpose.
Back in the 20th century, a method named after the surgeon Antonio Maria Valsalva was actively practiced. An Italian specialist studied the anatomy of the ear and concluded that the main function of the auditory tube is to ventilate the middle ear to maintain optimal pressure on both sides of the eardrum. In normal condition the pipe is closed. When diving under water, the pressure increases greatly. To normalize it, you need to exhale.
Initially, a technique based on this discovery was practiced to cleanse the middle ear and diagnose brain and heart diseases. Later, the scope of application became wider: a modified Valsalva maneuver began to be actively used in urology for the diagnosis of varicocele.
Scanning of the small saphenous vein and vein of Giacomini.
The patient should stand facing away from the operator, knee slightly bent, heel on the floor, weight on the opposite limb. Start scanning from the back of the knee. Use a transverse view to identify the major veins of the popliteal fossa. Determine whether there is a sapheno-popliteal junction. If there is, visualize it carefully in a longitudinal view.
Examine the PV proximally and distally to the junction, the entry of the calf veins, and the SPS for reflux or thrombosis. Determine whether there is failure of the SPS with reflux along the SVC. Reflux may occur during contraction of the gastrocnemius muscle or manual compression (systolic phase), indicating possible obstruction of the popliteal and/or femoral vein. Typically, reflux is more obvious during relaxation of the calf muscle (diastolic phase). If there is reflux, measure the diameter of the SVC 3 cm distal to the saphenoplasty joint (at the popliteal crease and mid-calf). The level of the SPS relative to the popliteal skin fold should be determined. The small saphenous vein may connect to the popliteal vein medially, posteriorly, or laterally, so it is advisable to record its position relative to the popliteal vein. Be sure to check the presence or absence of an artery accompanying the small saphenous vein or calf veins. This is important when planning sclerotherapy under duplex scanning control. Look for alternative sources of reflux, including the connection of the SVC with perforators in the popliteal fossa, branches of the great saphenous vein, pelvic veins to the buttocks or perineum, the extension of the SVC on the thigh, and variations of the vein of Giacomini. The Giacomini vein lies quite deep for most of its length. It is advisable to determine its distal connection with the small saphenous vein and its proximal connection with the great one.
Scanning veins below the knee.
The patient is in a standing position (this is preferable for superficial veins) or in a sitting position, with the feet down and resting on the operator's knee or on a step.
With experience, almost all deep veins of the leg can be identified. Reflux in the posterior tibial veins most informatively reflects clinical features. Unfortunately, as a rule, little attention is paid to the study and assessment of the condition of the so-called sural veins. Meanwhile, the musculovenous sinuses of the soleus and gastrocnemius muscles play a very important role in the outflow of blood from the lower extremities. We devoted a lot of time to studying the anatomical and physiological features of their structure and conducted a large series of studies and experiments. Ultrasound aspects of a comprehensive examination of the sinuses of the leg under normal conditions and in various pathological conditions will be presented in a separate work with corresponding recommendations. Superficial veins of the calf.
Examine the GSV for reflux in the calf area. In 97% of cases with incompetence along the entire length of the thigh, this vein is consistent from the middle to the lower third of the leg. In the upper third of the leg below the knee, it may be insolvent for a limited period up to the point where varicose veins flow into it. After surgical interventions for VD, varixes can be located in the ankle and foot area. Be sure to examine the posterior arch vein (vein of Leonardo), which is the main tributary of the great saphenous vein in the lower leg. Look for perforators that can lead to the development of varix in this area.
Calf perforators.
The perforators pass through the deep fascia, which appears as a distinct stripe on the B-mode image. You should look for perforators around the circumference of the calf. Of course, not all of them can be identified. If “from” blood flow is detected, then measure their diameter at the site of the deep fascia and the level from the lateral and medial ankles. However, measuring diameter alone will not differentiate successful from unsuccessful perforators. Check for the presence or absence of bidirectional flow using color Doppler or spectral analysis after distal muscle compression or isometric contraction of the gastrocnemius muscle. There is no consensus yet regarding the pathological significance of bidirectional blood flow. Based on extensive everyday experience of comparing clinical data and the results of duplex angioscanning, we believe that true pathological incompetence of the communicating veins exists only if reflux is detected in the diastolic phase of muscle relaxation or when compression is removed. Some authors have suggested that testing in- and out-flow separately during gastrocnemius contraction or compression and release of the gastrocnemius muscle will help differentiate pathological perforators from re-entrants. It should be emphasized that the study of morphology and hemodynamic changes in patients with chronic venous disease of the lower extremities at all stages differs from testing (checking) for the presence of deep vein thrombosis.
Organization of research and registration.
Different countries have different practices regarding who conducts the ultrasound examination. In the USA and Australia, this procedure is performed by certified vascular specialists - technicians, in the UK - by scientists - vascular researchers, in many other countries - by radiologists (radiologists). Of course, the optimal situation is when the doctor conducting a clinical examination of the patient also performs ultrasound scans of the venous system. Unfortunately, this is quite rare in everyday clinical practice. Therefore, any specialist examining a patient with chronic venous disease must know the basic indications for conducting an ultrasound examination:
- primary varicose veins;
- recurrent varicose veins;
- skin changes or ulcers of the leg;
- other manifestations (swelling, pain);
- venous malformations;
- suspicion of deep vein thrombosis.
In reports on the results of duplex ultrasound scanning of the veins of the lower extremities, the reason for the examination must be indicated. An ultrasound image can be presented to demonstrate the findings. However, the dynamic nature of the study limits the value of these images. Diagrams and text are more effective. Video data is suitable for monitoring the quality of treatment. The report requires detailed information about reflux, the development of varixes, or other features of the disease. This includes the development of incompetence at each junction of the GSV and SSV, the degree of reflux in each trunk, and a description of the GSV separately in the thigh and lower leg. The morphological and hemodynamic pathology associated with varicose veins, as well as the location of the affected veins, should be indicated on the diagram. For recurrent varicose veins, it is desirable to know whether a relapse has occurred at the site of a previously ligated junction or whether the trunk of the main superficial vein, which was previously subjected to some kind of influence, has been recanalized. The diameters of the affected veins should be indicated, including saphenous vein trunks and perforators, because this may affect your treatment. It is imperative to focus on the morphology of the veins: hypoplastic, atretic or previously removed.
It is especially necessary to dwell on the description of deep and superficial veins that have suffered from thrombophlebitis. It is necessary to carefully describe the patency of the vein today, whether there is occlusion, recanalization, whether the recanalized vein has become incompetent and to what extent.
The report must contain complete information obtained by the ultrasound investigator for the clinician treating the patient. It is desirable that all specialists undergo systematic retraining, which should include not only theory, but also practical training with extensive clinical practice.