Occlusion of the subclavian artery is an atherosclerotic lesion of one of the most important arteries of the body.
The process of development of occlusion (literally “closing”) of the subclavian artery is accompanied by the deposition of cholesterol and fat cells in its walls, the proliferation of connective tissue (sclerosis), and the deposition of calcium salts (calcification). This leads to the formation of the so-called. plaques - pieces of tissue that seem to stand across the path of blood flow.
This process leads to a narrowing of the subclavian artery, which in turn contributes to the development of cerebrovascular insufficiency and ischemia (that is, insufficient blood supply) of the upper extremities. The development of atherosclerosis also threatens with more serious consequences, since the detachment of plaques from the walls of the artery can cause blockage of blood vessels, which can also lead to death.
Occlusion of the subclavian artery is not an independent disease, but is a consequence of atherosclerotic changes in the arteries (overgrowth of connective tissue and plaque formation) and stenosis (narrowing of the walls of blood vessels).
In 15% of patients, symptomatic cerebral ischemia is caused by damage to the subclavian arteries (SCA) or brachiocephalic trunk (BCS) with the development of vertebral-subclavian steal syndrome (VSS) [1].
The steal phenomenon occurs when there are two vascular beds with different peripheral resistances. To the development of vertebral-subclavian steal syndrome ( eng.:
“steal” - steal, steal, rob) are caused by occlusive-stenotic lesions of the first segment of the RCA or BCS, as a result of which blood flows retrogradely through the ipsilateral vertebral artery into the arm, robbing the brain - the vertebrobasilar system (VBS). In this case, the brain can lose up to 20% of the required blood flow [2].
According to the WHO expert group (1970), vertebrobasilar insufficiency (VBI) is “a reversible disorder of brain function caused by a decrease in the blood supply to the area supplied by the vertebral and basilar arteries.” In accordance with ICD-10, VBI is classified under G45.0 - “vertebrobasilar arterial system syndrome.”
Ischemia in the VBS can manifest itself not only in the form of reversible transient ischemic attacks or chronic cerebrovascular insufficiency, but also the development of strokes. Within 5 years, 30% of patients with symptoms of VBI develop a stroke [3]. Strokes in the VBS against the background of SSPO are hemodynamic in nature.
The formation of SPPO is also possible with damage to the BCS, simultaneous damage to the first segment of the RCA and anomalous origin of the vertebral artery from the aortic arch [4, 5], occlusion of the proximal part of the vertebral artery and the first segment of the RCA [6]. Stealing in such cases develops through the subclavian-vertebral collateral network (branches of the thyrocervical and costocervical trunks). Occlusion of the BCS carries an additional risk of stealing the right carotid system with the development of vertebral-subclavian-carotid steal syndrome [7-9]. In patients who have undergone mammary coronary bypass surgery, with stenosis or occlusion of the first segment of the RCA, coronary-subclavian steal syndrome through the internal mammary artery may develop [2, 10, 11].
SPPO was first described by L. Contorni in 1960 [12]. In 1961, C. Fisher [13] proposed the established term SPSS. In the literature, SPPO can also be found under the name “reverse Robin Hood syndrome.” In 1965, J. Vollmar et al. [14] identified four variants of stealing in case of occlusion of the first segment of the RCA: vertebral-vertebral, carotid-basilar, external-vertebral, carotid-subclavian. The most common cause of the development of occlusion or critical stenosis of the proximal segment of the RCA and other brachiocephalic arteries is atherosclerosis, less often nonspecific aortoarteritis [15-20], as well as deformation of the proximal segments of the RCA with the formation of septal stenosis [21]. Atherosclerotic occlusions and stenoses of the BCJ and RCA occur more often at the age of 50-60 years. The left RCA suffers 2-3 times more often than the right [22, 23].
In 70% of cases, the left vertebral artery is 1.5-2 times wider than the right [24], being the main source of blood supply to the posterior parts of the brain, so even the slightest change in blood flow through it can lead to a disorder in the entire VBS.
Combined damage to the vertebral artery and RCA with the development of steal syndrome occurs in 6.1% of cases [25]. Damage to the vertebral artery is most often localized in the initial part of the V1 segment - in the area of the mouth [26]. Concomitant carotid artery stenosis occurs in 82–84% of patients with SPPO [27]. Among the combined hemodynamically significant lesions of the carotid system, the most common is stenosis of the bifurcation of the common carotid artery [23, 28].
The diversity of the structures of the blood-supplied VBD and the functions they perform determine the polymorphism of the clinical manifestations of VBD. Chronic occlusions of the arteries of the upper limb are usually asymptomatic due to good collateral blood flow at the level of the shoulder, and VBI in the initial stages has many clinical masks (cervical osteochondrosis, diseases of the inner ear, etc.) [18-20]. Symptomatic stenosis of the first segment of the RCA is much less common than with damage to the carotid artery. At the same time, symptoms from the upper limb occur in 54% of cases, cerebral symptoms - in 77% [29]. An asymptomatic course is observed in 20% of patients with isolated lesions of the RCA [30]. RCA stenosis can be complicated by distal atheroembolism [31].
Clinically, steal syndrome is manifested by symptoms of VBI. Clinical manifestations of VBN may include signs of dyscirculatory encephalopathy, hemispheric symptoms in the form of the development of sensory and pyramidal disorders (alternating syndrome), vestibular (ataxia, nystagmus, intention tremor) and cochlear (unilateral hearing loss, tinnitus), visual (loss of visual fields, photopsia) symptoms, symptoms of cranial nerve dysfunction (trunk symptoms in the form of oculomotor disorders, peripheral paresis of facial muscles, bulbar and pseudobulbar syndromes); Characterized by drop attacks (Unternharnscheidt syndrome), syncope, systemic and non-systemic dizziness. Possible accompanying vegetative manifestations: nausea, vomiting, changes in blood pressure, heart rate, hyperhidrosis [20]. The severity of these signs depends on the location and size of the ischemic focus, as well as the state of the collateral circulation [32]. A case of transient antegrade amnesia due to SPPO has been described [33].
SPPO and symptoms of cerebral ischemia are more often detected in patients with concomitant lesions of the RCA and other brachiocephalic arteries [30]. VBI can occur as a thromboembolic or hemodynamic type [34]. The severity of clinical manifestations in the thromboembolic type is much higher [35].
A change in blood flow through the vertebral artery does not always lead to VBI due to compensated blood flow through the closed circle of Willis [36]. Functional inferiority or disconnection of the circle of Willis due to the absence of one or two anterior or posterior communicating arteries can lead to the development of intracerebral steal syndrome [37].
Subjective signs of brachial ischemia are chilliness, coldness, numbness of the fingers, “intermittent claudication” of the hand; in the later stages, pain at rest and trophic disorders develop. The presence of steal syndrome can be suspected already at the stage of physical examination - differences in blood pressure (BP) and pulse in both arms (probably their complete absence), systolic murmur over the projection of the stenotic RCA [15, 38-40]. Gradient A.D. on both arms more than 20 mm Hg. speaks in favor of the presence of SPPO [41, 42].
To diagnose VBI, functional tests of de Klein, Khotan, etc. can be used. SPPO is confirmed by triplex ultrasound scanning - a collateral type of blood flow distal to the site of RCA lesion, as well as constant or transient retrograde blood flow in the systole phase through the vertebral artery on the same side.
However, the antegrade type of blood flow through the vertebral artery when the first portion of the RCA is affected does not exclude the presence of steal syndrome due to the well-developed spinal-subclavian collateral network [43]. To identify the so-called latent steal syndrome, a test with reactive hyperemia is performed - at the time of decompression of the brachial artery, an acceleration of blood flow in the subclavian-vertebral branches and a decrease in the distal sections (V4) of the vertebral artery are recorded.
Depending on the results of a triplex scan with a reactive hyperemia test, three types of SPPO are distinguished [44]: 1) permanent (with occlusion or critical stenosis of the RCA or BCS orifice of more than 90%) - blood flow through the vertebral artery has the opposite direction, and the reactive hyperemia test registers persistent increased retrograde blood flow that persists for several seconds; 2) transient (with stenosis of more than 50%) - blood flow in the vertebral artery has the opposite direction only in the systole phase, the reactive hyperemia test shows a slow restoration of the original picture; 3) latent (with stenosis less than 50%) - blood flow in the vertebral artery is antegrade, but changed. The reactive hyperemia test in such cases shows a rapid return of the original Dopplerogram.
Another confirmatory research method is traditional selective X-ray contrast angiography - filling the affected RCA through the vertebral artery system. The number of severe complications during this study reaches 3.5%, mortality - 2.4% [45], and the use of single-plane angiography in some cases does not allow reliably determining the degree of stenosis. To diagnose the nature and detail of the lesion, determine the morphology of the plaque, and the state of the circle of Willis, MSCT angiography has recently been increasingly used, and the use of TCD helps to determine the disorder and reserve of cerebral hemodynamics [46, 47].
The morphology of atheromas plays a significant role in the development of cerebrovascular events due to microembolization or acute occlusion.
The combination of MSCT and magnetic resonance angiography has great potential for determining the morphology of atherosclerotic plaques [1].
For functional assessment of cerebral circulation, dynamic angioscintigraphy and Dopplerography are used in combination with a stress test, which makes it possible to identify functional disorders of cerebral circulation already in the early stages of atherosclerosis of the brachiocephalic arteries and evaluate the effectiveness of surgical treatment [48].
A functional test with dosed physical activity has been described [23], which shows the dependence of the increase in steal syndrome on the amount of physical activity and proves the uncontrollability of SPO.
To assess the oxygen status of the brain, it is possible to use cerebral oximetry with the calculation of the oxygen extraction coefficient and a breath-hold test [49].
In cases of combined lesions of the brachiocephalic arteries, determination of the most hypoperfused area of the brain is possible thanks to MRI or CT perfusion [50]. The ideal diagnostic method for detecting cerebral blood flow insufficiency is the study of the oxygen extraction fraction using positron emission tomography. The use of MSCT and MRI is leading in the diagnosis of acute cerebrovascular accidents [50].
The presence of even asymptomatic SPO due to its unpredictable course is an absolute indication for surgery [23, 30, 51]. Since 1980, endovascular methods of recanalization of the affected segment have been used in the world to treat patients with SPPO. Their undeniable advantage is their low invasiveness and traumatic nature [52–57]. The likelihood of successful endovascular recanalization is reduced in the presence of gross atherocalcinosis or occlusion. The technical success potential for recanalization of RCA occlusions is much lower than for stenotic lesions [58]. Technical and angiographic success of recanalization of occlusions of the BCS and RCA is possible in 57–96% of cases [54, 59–64]. An additional negative factor is the variability of the anatomy of the vertebral-subclavian arterial zone, affecting the results of not only endovascular interventions, but also open reconstructive operations. In the presence of tortuosity or variations in the origin of the RCA and BCS, which do not allow the catheter to approach the site of stenosis/occlusion, open interventions should be considered as the operations of choice [59].
In the case of BCS pathology, prosthetics or bypassing of the BCS directly from the aortic arch is usually performed as an open operation. Access to the stenotic BCS is possible through a median sternotomy. Mortality in case of BCS bypass is in the range of 5.8-8% [65], and the number of complications is 16.7% [56]. At the same time, the 5-year patency of shunts is 94%.
RCA reconstructions can be performed from either the thoracic or cervical approach. The cervical approach is considered safer not only in terms of mortality, but also ischemic complications [17, 59, 66, 67]. Mortality after operations on the BCJ or RCA performed through the thoracic approach ranges from 3 to 19% [59, 66, 68, 69].
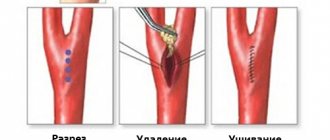
In case of RCA occlusion, preference is given to reconstructive operations, and in case of stenosis, endovascular operations are preferred [70, 71]. In cases where open surgical tactics are chosen for RCA pathology, the method of choice is carotid-subclavian bypass or carotid-subclavian anastomosis [23].
Vascular grafts used for carotid-subclavian bypass are characterized by excellent patency [72]. Postoperative mortality is less than 1%, with a 95% primary 10-year graft patency rate [73]. Prostheses made of polytetrafluoroethylene, dacron, and less commonly autovein are used as plastic materials. During cross-clamping of the carotid artery, it is recommended to stop stealing the VVS by clamping the vertebral artery or the 2nd segment of the RCA [74].
Subclavian-carotid anastomosis, first performed in 1964 by J. Parrot, is an excellent treatment method, but requires wider access in the neck and is impossible without the use of additional explants for prolonged lesions with transition to the second segment of the RCA. Postoperative mortality is less than 1%, and the patency of the anastomosis in the long-term period reaches 96-100% [75-77]. Some authors [30, 59, 78—80] believe that transposition of the RCA into the common carotid artery has a number of advantages over carotid-subclavian bypass.
Various options for extra-anatomical cross-bypass are rarely used due to the greater length of the bypass, the opposite direction of blood flow in the donor artery, physical discomfort and the possible upcoming coronary artery bypass surgery in the future.
Some supporters of bypass operations, along with carotid-subclavian bypass, talk about the good effect of carotid-axillary bypass [81].
A rare option for reconstructive surgery for pathology of the first segment of the RCA and a sufficient diameter of the vertebral artery is the carotid-vertebral anastomosis “side to side” [82].
The incidence of restenosis and reocclusion of the RCA and BCJ after endovascular intervention ranges from 7.3 to 29.8% [59, 60]. The immediate and long-term results of open and endovascular interventions on the BCS are not statistically different [83]. Primary and 5-year patency of the RCA after stenting reaches 80-100%, and after balloon angioplasty - only 54%, and with stenoses it is higher [60, 84-87]. For the prevertebral segment of the RCA, it is better to use balloon-expandable stents, and for the postvertebral segment, self-expanding ones [2, 54, 88, 89]. When stenting the RCA orifice, the stent should protrude 2 mm into the aortic lumen and not overlap the orifices of the vertebral and internal mammary arteries.
Interventions are the operation of choice for proximal lesions of the branches of the aortic arch [17, 84, 89, 90]. Some authors have noted [91–93] that the long-term results of carotid-subclavian bypass surgery are better than those of RCA stenting.
Currently, in order to reduce the frequency of reocclusions and restenoses after stenting, two-component antiplatelet therapy is recommended. During endointerventions on the BCS, it is necessary to use distal devices to protect the brain from microembolism. The likelihood of cerebral embolic complications when performing endovascular operations on the left RCA in the presence of reverse blood flow through the vertebral artery is minimal [88].
In most cases, transfemoral access is used for stenting of brachiocephalic arteries. In cases of severe damage to the aortoiliac femoral segments, their deformation or tortuosity, as well as occlusion of the RCA from the orifice, retrograde (radial, ulnar, brachial, axillary) or combined approaches are used. The most preferred approach is through the brachial artery. The axillary artery is more difficult to puncture and more difficult to achieve effective post-puncture compression. The likelihood of iatrogenic occlusion of the arteries of the forearm is higher than that of the brachial artery. However, in the event of occlusion of one of the arteries of the forearm, with a positive Allen test, the second will compensate for blood circulation in the hand [88]. To perform the Allen test, the radial and ulnar arteries are simultaneously clamped, while the patient is asked to clench his hand into a fist, then one of the arteries is released. If reactive hyperemia appears within 5-10 seconds, the test is considered normal. Performing stenting from a radial approach is a safe technique [94].
Resolving the issue of the volume and priority of surgical treatment in the combined treatment of brachiocephalic arteries is one of the most important tasks in the surgery of ischemic cerebral disease. With combined lesions of the first segment of the vertebral artery and the RCA, simultaneous endovascular intervention leads to a better clinical outcome [95]. In case of concomitant lesion of the contralateral carotid artery, the first stage is to reconstruct it; in case of homolateral localization, one-stage correction of blood flow is recommended, since revascularization of only the VBS leads to stealing of the carotid territory [30, 51, 96, 97]. It is safer to perform simultaneous reconstruction if a single surgical approach is possible and there is a high tolerance of the brain to cross-clamping of the carotid artery [98].
Causes and risk factors
The area where this compression occurs is called the superior thoracic outlet or thoracic outlet. The arm and neck are in constant motion, therefore, with the congenital narrowness of the gap between the collarbone and the first rib, constant trauma to the nerves of the cervical brachial plexus, subclavian arteries and veins occurs. Additional cervical ribs and shortening of the scalene muscles can lead to the development of compression of the vessels and nerves of the shoulder girdle. Common causes of superior outlet syndrome can be work-related or sports injuries.
The cause of compression of the neurovascular bundle of the arm is most often a congenital narrowing of the space between the first rib and the collarbone. However, thoracic outlet syndrome develops only under certain conditions:
- Anatomical defects
Congenital accessory cervical ribs located above the first rib or a shortened anterior scalene muscle can compress the neurovascular bundle. Sometimes the subclavian bundle can be compressed by the tendon of the pectoralis major muscle due to the anatomical features of the shoulder girdle.
- Poor posture
The habit of sitting and standing with drooping shoulders can cause compression of the vascular bundle at the exit from the chest.
- Injury
A traumatic event, such as a car accident with a fracture of the clavicle or sternum, can cause changes in anatomical relationships and lead to compression of blood vessels and nerves.
- Same type of movements in the shoulder girdle
Sports activities, work on a conveyor belt and other activities associated with constant raising of arms above the shoulders can contribute to the development of clinical signs of compression of the neurovascular bundle.
- Pressure on the shoulder joints
Carrying heavy bags on the shoulder or backpacks can be a provoking factor for the onset of the syndrome.
Prevention
Measures to prevent the development of occlusion of the subclavian artery are aimed at preventing diseases that cause this pathology. They consist of giving up smoking and other bad habits, eating right (especially excluding fried and fatty foods), regularly monitoring blood pressure and preventing stress and traumatic situations.
Occlusion of the subclavian artery is accompanied by complete blockage of the lumen of this blood vessel and insufficient blood supply to the brain and upper extremities. This pathology can lead to a significant deterioration in performance, stroke and disability. If there are pronounced signs of occlusion of this artery, the patient is indicated for surgical treatment aimed at restoring its patency.
Complications
For a long time, some patients reflexively react to pain with muscle fixation. They have to hold a rigid certain position in order to reduce pain. But, unfortunately, this reflex muscle defense aggravates the course of the disease and, ultimately, leads to increased pain. Muscle defence, in turn, then requires separate treatment. It is important to begin treatment for SLM in its early stages. If left untreated, SLM can cause significant nerve or vascular damage, including limb loss.
Variants of Thoracic Outlet Syndrome
Neurological This form of thoracic outlet syndrome is characterized by compression of the brachial plexus. The brachial plexus is a network of nerves that arise from the spinal cord and pass through the space between the first rib and the collarbone to the arm. These nerves stimulate muscle movement and conduct sensation in the shoulder, forearm, and hand. Most often, it is the neurological variant of thoracic outlet syndrome that is observed, when patients complain of pain in the arm, weakness, numbness, and tingling. Vascular This type of disease occurs when the subclavian vein or artery becomes compressed between the collarbone and the first rib or pectoral muscle. Such patients may develop thrombosis of the subclavian vein or artery with the development of vascular insufficiency in the arm. Mixed When there are signs of compression of the nerves and vessels at the exit from the chest. This is the most painful form, but much easier to diagnose.