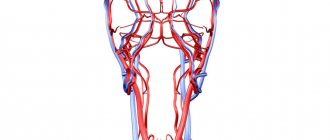
Angioplasty and stenting of the internal carotid artery (ICA) is an intervention that restores blood supply to the brain. Performed to treat, prevent and prevent stroke.
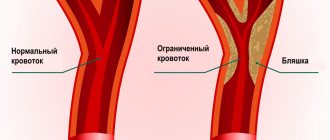
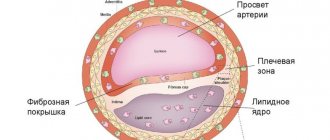
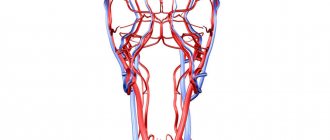
The carotid arteries are the main arteries that supply blood to your brain. They can become clogged with fatty deposits (plaques) that slow or block blood flow to the brain, a condition known as atherosclerotic carotid artery disease, which can lead to stroke.
Endovascular intervention to restore full blood flow through the carotid artery is performed minimally invasively under local anesthesia through a small puncture in the common femoral artery (in the groin) or in the radial artery (in the wrist) and includes insertion, positioning and implantation of a stent at the site of narrowing of the internal carotid artery.
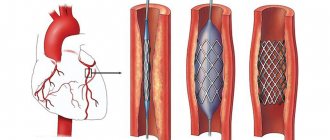
For such interventions, a trap filter (a modern device for protecting the brain from thromboembolism) is required. Then a stent is placed, which expands the artery from the inside and keeps it open (this is a self-expanding metal frame with a specially designed closed cell or double-layer stents that incorporate all the advantages of previous generations).
Angioplasty and stenting of the internal carotid artery are analogous to open surgery and can also be used when traditional carotid surgery (carotid endarterectomy) is impossible or too risky.
Indications for angioplasty and stenting of the internal carotid artery
Angioplasty and internal carotid artery (ICA) stenting may be necessary for the treatment or prevention of acute ischemic stroke if:
- Your internal carotid artery is narrowed by 70% or more, especially if you have had a stroke (then more than 50% narrowed) or stroke symptoms and are not in good enough health to have open surgery - for example, if you have severe heart disease or lungs or after radiation therapy;
- You have already had a carotid endarterectomy and are experiencing new narrowing after surgery (restenosis)
- Places of narrowing (stenosis) are difficult to reach during endarterectomy
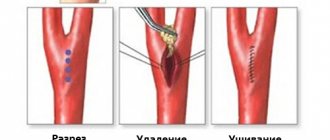
In some cases, carotid endarterectomy may be a better choice than angioplasty and stenting to remove accumulations of fatty deposits blocking an artery. You and your doctor will discuss which procedure is safest for you.
Risks of Angioplasty and Stenting
Complications can occur with any medical procedure. Here are some of the possible complications of carotid angioplasty and stenting:
- Stroke or mini-stroke (transient ischemic attack or TIA) . During angioplasty, blood clots that may form on the catheters can break free and travel to your brain. You will receive blood thinners during the procedure to reduce this risk. A special trap filter is used for these procedures, but the risk is associated with placing it after the catheter has passed the narrowing site.
- New narrowing of the carotid artery (restenosis) . The main disadvantage of carotid angioplasty is the likelihood that your artery will narrow again within a few months of the procedure. Special drug-eluting stents have been developed to reduce the risk of restenosis.
- Blood clots . Blood clots can form in stents even weeks or months after angioplasty. These clots can cause stroke or death. It is important to take aspirin, clopidogrel (Plavix), and other medications exactly as prescribed to reduce the chance of clots forming in your stent.
- Bleeding . You may have bleeding at the injection site. Usually this simply results in a hematoma, but sometimes serious bleeding occurs and blood transfusions or surgical procedures may be required.
Stenting as a possibility to restore vascular patency
Arterial stenting is a low-traumatic, minimally invasive endovascular intervention, the essence of which is to install a stent in a narrowed area of the vessel. For the first time, the technique of dilating blood vessels through the introduction of a special frame (stent) was proposed by S.T. Dotter, born in 1969. In 1977, with the participation of A. Gruentzig, R. Myler and E. Nappa, the first intraoperative coronary balloon angioplasty (dilation of the artery using a special balloon) was performed in San Francisco. The first coronary artery stenting in humans was performed by J. Puel et al. in March 1986 in Toulouse (France). In 1993, the FDA approved the use of stents for the treatment of acute and impending coronary artery occlusions complicating coronary balloon angioplasty; in 1994, approval was received for the use of stents for the treatment of native coronary arteries. The stenting method has become actively used to restore the patency of the coronary arteries. The function of the stent is to prevent the artery from narrowing back after the plaque is expanded using special instruments. As a rule, before stenting, predilatation of the artery is performed - expansion of the artery with a special balloon (like preparing the artery before stenting).
Preparing for a non-surgical procedure
Before elective stenting, your endovascular surgeon will review your medical history and perform a physical examination. Can be assigned:
- Ultrasound . To obtain images using sound waves of the narrowed artery and the speed of blood flow to the brain.
- Contrast-enhanced computed tomography (MSCT) or Magnetic resonance angiography (MRA) . This diagnostic produces highly detailed images of blood vessels using radiofrequency waves in a magnetic field or X-rays injected with a radiopaque contrast agent.
Food and medicine
You will receive instructions about what you can eat or drink before your angioplasty and ICA stenting. Preparation may be different if you are already in the hospital before the intervention.
The night before your endovascular surgery:
- Follow your doctor's instructions about adjustments to your current medications. Your doctor may tell you to stop taking certain medications before having angioplasty, especially if you take certain diabetes medications or blood thinners.
- Arrange transportation home in advance. Angioplasty usually requires a hospital stay, and you may not be able to go home the next day due to the lingering effects of the sedation.
Causes
The formation of atherosclerotic plaques in blood vessels is caused by the deposition of cholesterol in the walls of the arteries, and their gradual increase causes a narrowing of the vessel itself (which, in turn, leads to a lack of blood supply to tissues and organs - ischemia), and when the plaque is destroyed, acute ischemia of organs and tissues occurs from -for arterial thrombosis, causing heart attacks and strokes. Most often, plaques are deposited simultaneously in the arteries of different organs, and the disease manifests itself as systemic. The following are most susceptible to atherosclerosis:
- coronary arteries;
- arteries of the lower extremities;
- brachiocephalic arteries (supplying blood to the brain);
- renal arteries.
Differences from surgery
Angioplasty and stenting of the internal carotid artery (ICA) is considered a high-tech, minimally invasive endovascular intervention, performed under local anesthesia.
There are no scars left on your body on your neck, except for a very small cut - about 2-3 mm (puncture site) in a blood vessel in the groin or on the wrist.
There is no need for general anesthesia; everything is done under local anesthesia, so you are awake during the procedure. Fluids and medications are given through an IV.
Before the procedure
- You will be taken on a gurney to the cath lab operating room. You will place your head in a comfortable cup-shaped area on the operating table.
- Your wrists and groin should be shaved on both sides and prepared with an antiseptic solution.
- A local anesthetic is injected into the puncture site for pain relief.
- To monitor the ECG of the heart, electrodes will be connected to the chest.
During the procedure
Once you are calm, your operating x-ray surgeon will puncture an artery, usually the femoral artery in the groin area. The angioplasty and stent procedure are described below.
- A special catheter with a unique bend (tube) is inserted into the artery . Under X-ray control, a catheter with the necessary instruments and a balloon is brought to the narrowing of the carotid artery. You will not feel the catheter going through the arteries because the insides of the arteries do not have nerve endings. The entire instrument is guided through this catheter to the narrowed section of the artery.
- A radiopaque contrast agent (RCS) is injected into the carotid artery through a catheter . RCV may cause a temporary feeling of warmth on one side of your face. The RCV gives a detailed view of the narrowed artery and blood flow to the brain.
- The filter is opened in the artery . A filter, called an embolic protection device, is inserted beyond the narrowing to catch any particles that may break off from the narrowed section of the artery (plaque) during the procedure.
- A balloon catheter on the delivery system is positioned at the site of narrowing and inflated to dilate the vessel.
- A small metal mesh tube (stent) may be placed in the newly opened vessel . A self-expanding metal frame with a specially designed closed cell or double-layer stents that incorporate all the advantages of previous generations. The expanded stent provides support that helps prevent the artery from narrowing again.
- The filter, balloon and stent delivery system, and the catheter itself are removed.
When the procedure is complete, you lie still in one position and the bleeding stops at the site where the tube was inserted. You will usually not have stitches, but a bandage will be placed over the small incision. You are then transferred to a recovery room.
After the procedure
To avoid bleeding from the catheter site, you will need to lie relatively still for several hours. You will either be in the recovery area or in your hospital room. After the procedure, you may be given an ultrasound of the carotid artery. Most people are discharged from the hospital within 24 hours of the procedure.
The catheter site may be sore and swollen for several days. There may be a small hematoma in the puncture area. You can take medications in the recommended dose needed to relieve discomfort as prescribed by your doctor.
You may need to avoid vigorous activity and heavy lifting for a week after the procedure.
Description of a clinical case
Patient K., 69 years old, was admitted to Clinical Hospital No. 1 of the UDP with a diagnosis of “Atherosclerotic occlusion of the carotid arteries. Arterial hypertension. Chronic bronchitis in remission. Chronic prostatitis.” Upon admission, the patient had no active complaints. In the anamnesis, since 2002, the patient noted episodes of loss of consciousness with a frequency of occurrence 2-3 times a year. The last episode was observed in May 2011. Suffering from arterial hypertension for a long time with a maximum rise in blood pressure up to 180/90 mmHg, adapted to a pressure of 140/80 mmHg.
On examination: general condition is relatively satisfactory, the skin is clean, normal color, no swelling. Breathing is harsh, no wheezing. Respiratory rate 18/min. Heart sounds are muffled, the rhythm is correct. Blood pressure 140/80 mmHg. Pulse 78 per minute. The pulsation over the carotid arteries is distinct, there is a weak systolic murmur in the projection of the subclavian artery on both sides. Neurological status without features.
According to color duplex scanning of the extracranial sections of the brachiocephalic arteries, occlusions of the ICA on both sides were identified with a compensatory increase in the speed parameters of blood flow in the system of the external carotid arteries. Hemodynamically significant stenosis of the ostia of the vertebral arteries on both sides (stenosis of the ostium of the left vertebral artery 90%, stenosis of the ostium of the right VA 75%). Also noted were stenoses of the ECA at the mouth on both sides, 35% each, and stenoses of the proximal segments of the subclavian arteries on both sides, 40%. Signs of hypertensive macroangiopathy of the extracranial segments of the brachiocephalic arteries, represented by C-shaped tortuosity of the CCA on both sides, S-shaped tortuosity of the extravertebral sections of the vertebral arteries on both sides and ectasia of the internal jugular veins on both sides. Multislice computed tomography revealed signs of dyscirculatory encephalopathy, mixed atrophic hydrocephalus and cerebral atherosclerosis. No data regarding stroke were received.
When performing angiography of the brachiocephalic arteries, the following data were obtained. The right subclavian artery is calcified, narrowed in the proximal third from the mouth by 50%. The right vertebral artery is narrowed at the mouth by 80%, in the distal third by 60%. The right CCA and ECA are passable, the contours are uneven. The right ICA is occluded from the mouth, the right anterior and middle cerebral arteries are well filled with collaterals from the vertebral arteries through the circle of Willis, uneven contours. The left subclavian artery is calcified, narrowed in the proximal third from the mouth by 40%, in the area of origin of the vertebral artery - by 30%. The left vertebral artery is markedly calcified in the proximal third from the mouth, narrowed at the mouth by 90%, and then has irregular contours. The left CCA and ECA are passable, the contours are uneven. The left ICA is occluded in the proximal third, the left anterior and middle cerebral arteries are well filled with collaterals from the vertebral arteries through the circle of Willis, uneven contours (see Fig. 1).
Thus, the blood supply to all parts of the brain was carried out exclusively through the vertebral arteries, each of which was significantly narrowed at the mouth. Taking into account the clinical picture, data from non-invasive research methods and the high surgical risk of open vascular surgery, it was decided to perform staged stenting of the mouths of both vertebral arteries.
How the treatment method works
The patient is connected to equipment with which his vital parameters will be monitored. A drug that reduces blood clotting is injected intravenously. If installed, a balloon-expandable stent is inserted through an introducer (an accessory device, a plastic tube with a sleeve). The introduction takes place under angiographic control. When the stent reaches the desired location, it is inflated with a balloon. When installing a self-expanding stent, a catheter is inserted through the introducer and the stent is delivered to the desired location. The catheter is then removed and the stent is deployed. After some time, the stent takes the required shape. The operation lasts on average 1-2 hours.
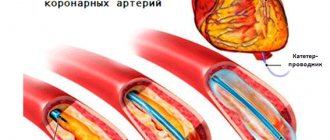
Balloon angioplasty
Through a puncture of the peripheral artery, a special guiding catheter is installed at the mouth of the coronary artery. A metal coronary conductor (0.36 mm thick) is passed through it. All stages of its progress are controlled by fluoroscopy. A balloon catheter is brought through a guidewire to the narrowing zone and predilatation of the narrowing is performed (preparing the artery for direct stenting), the diameter and length of the balloon depends on the nature of the vessel lesion. After preliminary balloon angioplasty, a stent is inserted into the artery. It is a balloon catheter with a compressed stent mounted on it. Such a stent is elastic and flexible enough to adapt to the condition of the vessel, and is also compatible with all tissues and organs of the human body. Under X-ray control, the inserted stent is inflated with a pressure of 9-20 atm and is securely implanted into the narrowed area. After this, the balloon is deflated and removed. Control angiography is performed to monitor the positioning of the stent, its full expansion and the absence of residual narrowing. If necessary, repeat angioplasty (inflation) of the stent area is performed using a balloon catheter of greater pressure and size. The stent remains in the lumen of the artery, but cannot move into the artery (since it is implanted with high pressure), and it cannot be removed from the artery. To restore blood flow in the artery, it is periodically necessary to use 2 or more stents (this depends on the extent and severity of the lesion).
Stenting is always preceded by a preparatory period. The patient undergoes a standard examination on an outpatient basis, including gastroscopy (to exclude erosions in the gastrointestinal tract). After the operation, the patient spends 1-2 days in a specialized department. If necessary (for medical reasons), the patient may spend the first day in the intensive care unit. Hospitalization usually takes 1-3 days. After discharge, the patient should be observed by a cardiologist at the clinic or a cardiologist (general practitioner) at his place of residence. When stenting, the patient should receive dual antiplatelet therapy (acetylsalicylic acid drugs + platelet ADP P2Y12 receptor blockers) for 3-6-12 months (depending on the type of stent and the plan of surgical treatment). This is necessary to ensure that blood clots do not form in the installed stents. Within the recommended period of time, the stent cells are completely covered with the body’s own cells, after which the risk of thrombosis is very low.
Benefits of stenting surgery
- Less traumatic (minimally invasive). The patient can very quickly return to his usual lifestyle. The rehabilitation period usually does not take more than a week.
- High-tech. During the operation, exclusively modern equipment and innovative expensive materials are used.
- High efficiency of treatment.
- Only stenting surgery is currently the only effective and safe treatment for current myocardial infarction, which makes it possible to reduce the area of the affected myocardium or even prevent the development of a heart attack and prevent the death of the patient.
Features of coronary artery stenting surgery
Coronary stenting is the placement of a stent into a narrowed section of a coronary artery. Access to the vessel can be made through the femoral or radial artery. The operation itself is performed under hypocoagulation conditions, that is, special drugs are introduced into the patient’s blood that prevent blood clotting, making the blood “liquid.” That is why it is very important that at the time of the operation the patient does not have obvious or hidden sources of bleeding, there are no erosions or ulcers in the gastrointestinal tract.