The carotid artery is a paired large blood vessel that rises to the head along the anterolateral surface of the neck on the right and left. It originates in the chest cavity, branching from the aorta, the main artery of the human body that supplies blood to all internal organs. The division of the carotid artery into external and internal trunks (bifurcation) occurs in the area of the thyroid cartilage of the larynx, hyoid bone or under the lower jaw. The outer part provides blood supply to the face, neck and scalp, while the inner part supplies blood to the brain.
Classification and causes of diseases
In some cases, pathologies of the brachiocephalic arteries are provoked by anomalies of the anatomical structure - excessive tortuosity of the vessels or fibromuscular dysplasia. Somewhat more often this occurs against the background of extravasal compression. However, in total, the listed reasons account for no more than 10% of all cases. The remaining 90% of catalysts occur in atherosclerotic lesions.
The causes of disturbances in the activity of the brachiocephalic arteries include:
- Atherosclerosis of the carotid, subclavian or vertebral artery;
- Primary and secondary vasculitis (arteritis);
- Persistent low or high blood pressure (hypo- and hypertension);
- Osteochondrosis of the cervical spine (and associated vascular compression);
- Severe heart pathologies;
- Developmental abnormalities or chronic diseases of the aorta;
- Aneurysms;
- Diabetic angiopathy;
- Vascular malformations;
- Dyscirculatory disorders (including vegetative-vascular dystonia);
- Mechanical injuries to the neck and head.
Atherosclerosis, which is the most common provocateur of diseases, is often caused by third-party endogenous and exogenous factors. These include long-term smoking, mature and old age, hypercholesterolemia, diabetes mellitus, unhealthy lifestyle and poor health in general.
With atherosclerosis of the brachiocephalic arteries, a persistent circulatory disorder in the brain occurs. It varies in intensity and severity, but almost always leads to tragic outcomes. In 80% of cases, such pathologies lead to a major stroke. The importance of timely contact with a cardiologist and vascular surgeon when symptoms are detected cannot be overestimated - sometimes early adequate treatment saves the patient from disability and death.
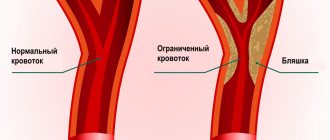
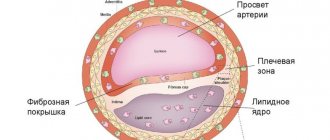
The formation of atherosclerotic plaque in the brachiocephalic arteries is a long process; traditionally it begins at a young age. A neoplasm gradually grows in the wall of a certain vessel, leading to a narrowing of the lumen of the artery, or its complete blockage.
Sometimes specialists diagnose non-stenotic atherosclerosis. This means that the lumen of the vessel is blocked by an atherosclerotic plaque by less than 50%, i.e. the disease does not entail potential critical risks. Without observation and treatment, non-stenotic atherosclerosis transforms into stenotic atherosclerosis, provoking vascular occlusion and serious disruption of the blood supply to the brain.
Tortuosity of the internal carotid artery
It was previously believed that vascular diseases were diseases of older people! But young people, and especially children, are the healthiest people, and they cannot suffer from vascular diseases... But this is not so. Why do children get headaches so often? Why, despite all our efforts, sometimes the assimilation of school material by a “healthy” child suddenly becomes low? Why does a child with normal tests suddenly cease to tolerate physical activity well and avoid physical activity? culture? Leaving the sports section? After all, where do cerebrovascular accidents occur in children? Oddly enough, in first place due to cerebrovascular insufficiency, and even apoplexy (cerebral strokes), are vascular diseases of the neck. And in children - pathological deformations, tortuosity of the internal carotid artery, due to which the blood flows unevenly, twisting into rapid “whirlpools”, which can cause thrombosis of both the cervical vessel and any brain vessel. And the frequency of detection of pathological tortuosity, irregular bends and kinks of the arteries of the neck in children is second in prevalence only to atherosclerosis in adults. Narrowing of the cervical vessels can lead to headaches, dizziness, poor academic performance, poor tolerance to physical activity, as there is insufficient cerebral blood flow
WHERE DOES THIS ATTACK COME FROM?
In adults, blood vessels become sick and deteriorate from a number of known reasons: high blood pressure, smoking, atherosclerosis, diabetes and inflammatory diseases. More often, from an incorrect lifestyle. And in children, vascular diseases of the neck are caused mainly by congenital causes. The vessels of the neck do not straighten enough in their innate movement towards the heart and remain tortuous. Blood does not flow correctly in such kinks. For these reasons, the wall of the vessel thickens, the lumen becomes narrow, or is even completely closed by a blood clot. Many children suffer from such pathological deformations of the neck vessels. But such diseases remain unrecognized, and the child with his complaints is regarded as a malingerer. And so often a pediatrician treats a child for asthenia or vegetative-vascular dystonia without success. This is due to the fact that the mandatory examination program for children does not include such high-tech studies of the vascular system of the head and neck as Doppler Doppler Doppler and Ultrasound Angioscanning. This equipment is simply not available in clinics. But our children often need identification and timely treatment of these conditions.
HOW IS IT TREATED?
Pathological deformations of blood vessels began to be discovered not so long ago. This is due to the development of diagnostic equipment capabilities. Therefore, in our age of advanced surgery, almost all identified children were previously sent for surgery. Surprisingly, surgical treatment is still the most common type of treatment today! pathological deformations of neck vessels. But today, medical experts, including surgeons themselves, no longer have an unambiguous attitude towards such operations. It turned out that under certain conditions, pathological tortuosity of the arteries can be safe for the child and disappear during his growth. It turned out that there was no need to operate on everyone. And pathological tortuosities can go away on their own. But it is important to ensure that while monitoring the dynamics of tortuosity, the child does not suffer from cerebral ischemia or lack of blood supply. And this can be achieved with special exercises aimed at improving blood flow through the vessels of the neck and brain! Often the most modern pills do not benefit the child, but correctly performed exercises will allow him to get rid of headaches, improve academic performance and feel healthy. Exercises to improve cerebral blood flow in case of pathological tortuosity of a particular vessel will be taught to the child and his parent by a trained specialist. These exercises will be the main treatment. If a child still needs consultation with a vascular surgeon or observation by a pediatric neurologist, this will be recommended.
Typical signs and symptoms
The symptoms of diseases of the brachiocephalic arteries are specific. If you feel alarming symptoms, but your doctor, after listening to the complaints, limited himself to pointless diagnoses (CFS, VSD, etc.), be sure to insist on an expanded diagnosis.
Symptoms of diseases of the brachiocephalic arteries include:
- General fatigue, weakness, decreased performance and concentration;
- Sharp headaches that occur when moving the head;
- Dizziness and syncope (short-term loss of consciousness);
- Fainting with low blood pressure;
- Noise or ringing in the ears;
- Transient paresis of the head and limbs;
- Visual disturbances (appearance of spots and flies in the field of vision, decrease in visual acuity with sudden recovery);
- Angina pectoris;
- Ischemia (sometimes asymptomatic);
- Itching, numbness, tingling in the left extremities;
- Swaying when walking;
- Nausea;
- Rare or frequent disorders of motor or speech functions (numbness, inability to communicate clearly).
The insidiousness of atherosclerosis of the brachiocephalic arteries lies in its “blurred” early course. The listed signs sometimes do not make themselves felt at all, or are expressed so weakly that the patient does not attach due importance to them. Ignoring diagnosis and treatment leads to death or a vegetative state.
Diagnostics
Depending on the preliminary diagnosis, the specialist prescribes a proper diagnostic regimen.
The process of diagnosing pathologies takes place in several stages:
- Face-to-face consultation with a survey of the patient regarding current complaints, duration and severity of symptoms, the presence of direct provoking factors;
- Study of anamnesis (personal and family);
- Laboratory tests for the presence of atherosclerosis (lipid profile with calculation of the atherogenic coefficient, biochemical blood test, determination of proteins in blood serum, etc., at the discretion of the specialist);
- Magnetic resonance or classical angiography;
- Ultrasound Dopplerography (Doppler ultrasound).
The latest study is considered the most informative. It allows you to determine:
- The speed and intensity of blood flow in the vessels;
- Places that prevent the movement of arterial blood to the brain;
- The presence of atherosclerotic lesions;
- The presence of detachments, dilations, occlusions, stenosis of the vessel;
- The presence of blood clots and atherosclerotic plaques, their size and shape;
- Deformations of the vessel (tortuosity, loops, protrusions, bends);
- Dimensions of the lumen of the affected vessel;
- Condition of the vascular walls (elasticity, mobility, firmness);
- Modifications of the arterial wall.
When a pathology is detected, the specialist prescribes comprehensive treatment to the patient.
Dear patients!
Carotid artery stenosis is a condition in which there is narrowing (stenosis) or complete closure (occlusion) of the carotid artery. A person has two carotid arteries located in the neck (right and left). These blood vessels carry blood to the brain and face. Most often, the patency of arteries suffers as a result of the development of atherosclerotic plaques in their walls, narrowing the lumen.
Symptoms of carotid artery stenosis
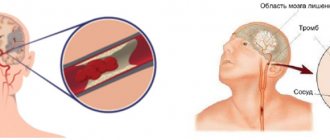
Most people with carotid artery lesions have no symptoms. If symptoms are present, the risk of ischemic stroke increases several times. The most common symptoms are transient (i.e., temporary) ischemic attacks, which are sometimes called minor strokes.
During an ischemic attack, blood supply to certain areas of the brain is reduced. This may cause temporary dizziness, blurred vision, numbness and tingling of the skin of the extremities, and weakness in an arm or leg, which usually lasts no more than 30 minutes. The risk of stroke is very high in people who have had a transient ischemic attack.
A stroke occurs when there is a sharp decrease in blood supply to a vessel supplying the brain or when it is occluded. Depending on the area of the brain affected, a stroke manifests itself as paralysis of an arm and/or leg, visual and speech disturbances, and behavioral changes. The larger the area of the brain affected, the greater the risk to life. Cerebrovascular accidents are one of the main causes of death in Russia. Ischemic stroke confidently ranks first among diseases leading to permanent disability. Only 10 - 20% of patients who have suffered a stroke recover their ability to work. The rest become disabled and have persistent neurological defects. Along with this, the risk of developing a recurrent stroke remains, since the root cause (atherosclerotic narrowing of the carotid artery) has not been eliminated.
Risk factors for stroke:
- Atherosclerosis
- Diabetes
- High blood pressure
- Smoking
- Eating fatty foods
- Excess weight
- Increased thrombus formation
Diagnosis of carotid artery stenosis
To determine whether you have stenotic lesions of the carotid arteries or not, your doctor will examine you. Even if you have no symptoms, your doctor may hear a murmur over your carotid arteries caused by blood flowing through the stenotic area. If necessary, Doppler ultrasound of the main arteries of the head (USDG MAG) will be prescribed first. It allows you to determine the localization of the narrowing, its degree and significance.
For a more detailed assessment of the condition of the carotid arteries, your doctor may recommend angiography (x-ray examination of blood vessels). This study is performed by catheterization, usually of the femoral or wrist artery, under local anesthesia in a special operating room equipped with an angiography unit.
Angiography of the carotid arteries
During this test, a very thin catheter is inserted into an artery in the leg or wrist and advanced toward the neck. A contrast agent is then injected through the catheter, making the carotid arteries and other arteries in the neck visible under X-rays.
On the eve of the examination, you should shave the skin in the groin area. You should also refrain from eating and drinking in the evening (except for medications). In the operating room, you will be covered with sterile sheets, which you cannot touch so as not to compromise sterility. During the test, your doctor will monitor your electrocardiogram (ECG) and blood pressure (BP). The catheter insertion site will be treated with an antiseptic and numbed. After this, the doctor will puncture your artery, through which he will pass a catheter to your neck. You won't feel it, but you will be able to see the catheter on the monitor.
You must follow all doctor's instructions. Sometimes you will need to hold your breath and not move. From time to time, from the administration of a contrast agent, you may feel warmth or a rush of heat in your head. The doctor will take pictures of the artery. If you have stenosis or occlusion of the carotid arteries, they will be detected.
Depending on the results obtained, you may be recommended a treatment procedure or scheduled for re-examination at a later date.
Treatment of carotid artery stenosis
There are two methods of surgical treatment. The first is an open endarterectomy performed by vascular surgeons. The second is a modern, minimally invasive, x-ray surgery - stenting. Both methods have their indications and contraindications. Therefore, the question of choosing one of them is always decided individually.
Carotid endarterectomy is a surgical operation aimed at removing the inner wall of the carotid artery affected by atherosclerotic plaque. The surgical technique is as follows: under anesthesia, an incision is made in the neck in the projection of the carotid artery. The artery is isolated and opened at the site of narrowing. The inner part of the artery wall is removed, along with the atherosclerotic plaque. Then plastic surgery of the artery is performed and the wound is sutured layer by layer.
Stenting is the installation of a stent, which is a metal tube consisting of cells, into a narrowed part of an artery. Expanding, the stent pushes the narrowed walls of the artery apart from the inside and constantly maintains them in a straightened state. Thanks to this, the internal lumen of the artery is restored and thereby the blood supply to the brain is improved. The following goals are pursued with stenting: elimination of chronic cerebral ischemia and prevention of ischemic stroke (or prevention of its recurrence).
The first stages of carotid artery stenting are carried out in the same way as an angiographic study: preparation, local anesthesia, puncture of the artery, insertion of a catheter and administration of a contrast agent. Before the operation, the patient is connected to special monitoring equipment that monitors parameters such as blood pressure and heart rate. The entire operation takes no more than an hour. From time to time you may feel hot flashes in your head.
Stenting of the carotid arteries is performed with protection against microembolism of cerebral vessels during surgery. Today, many of the world's leading experts prefer so-called filters. The filter is a metal frame on which a membrane is located (vaguely reminiscent of an umbrella). The filter retains microemboli without interfering with blood flow through the vessel: blood flows through micropores in the membrane that do not allow emboli to pass through. In some situations, according to indications, other microembolic protection devices are used.
After puncture of the artery, having installed a guide catheter into the carotid artery affected by atherosclerosis, the doctor passes the guide with a filter above the narrowing of the artery. Then a stent is installed along the guidewire into the area of stenosis. On the monitor, the doctor can see and evaluate the result. In some cases, it may be necessary to inflate the installed stent with a special balloon catheter. At this point, you may feel some discomfort in the neck and a change in heart rate. This is normal and should not be a concern. All manipulations are monitored using X-rays using a special high-tech angiographic device. The radiation dose is minimal and absolutely safe. Many such operations are performed around the world every year.
At the end of the intervention, the filter, balloon (if used) and guiding catheter are removed. The stent remains in the artery permanently, keeping it open. The doctor will apply pressure to the puncture site of the femoral artery for several minutes until the bleeding stops completely. The patient may be transferred to the intensive care unit for several hours to monitor vital signs. Strict bed rest should be observed for 24 hours after stenting. After returning to the room, you can eat and drink as usual.
The length of hospital stay depends mainly on the patient's well-being. After returning home, it is important to strictly follow all doctor’s instructions and regularly take prescribed medications. The further success of the operation depends on this. You should undergo regular examinations by a neurologist. If new complaints appear, you should immediately consult a doctor. For postoperative dynamic monitoring, Doppler ultrasound of the carotid arteries is very informative.
Following the doctor's recommendations after surgery improves treatment results and prognosis of the disease.
Prevention
The earlier stenosis of the artery carrying blood to the brain is detected, the easier it is to prevent the development of ischemic stroke and prevent disability of the patient. Therefore, at the first symptoms you should immediately consult a doctor.
Indications for intervention:
As has been described in detail above, candidates for carotid artery stenting are patients with hemodynamically significant stenoses of the internal carotid arteries. If the patient has already suffered an ischemic stroke or transient ischemic attack (TIA) in the territory of a stenotic artery, then the latter is considered symptomatic (that is, with a high degree of probability, it is the cause of the cerebral catastrophe that occurred). In such cases, stenosis of the internal carotid arteries (ICA) of more than 50% in diameter is subject to surgical treatment. If the patient has not suffered an ischemic stroke or TIA, but an ultrasound examination reveals ICA stenoses of more than 70% in diameter, the patient is also subject to surgical treatment. In cases where patients meet the indications described above, surgical treatment of targeted ICA stenoses has been shown to reduce the risk of ischemic stroke.
Clinical examples:
To illustrate clinical examples of performed stenting of the carotid arteries, there is no need to describe in detail the condition of the patients before and after the intervention, because the patient's well-being may not change significantly. The main goal of the intervention is stroke prevention.
Below are some illustrative examples of stenting:
Now patients have the opportunity to undergo examination and treatment at Medservice LLC by specialists with extensive experience in this area using the most modern angiographic complex Philips Allura Xper FD20 (Netherlands). This device with a new digital image processing system has a unique technology for suppressing noise and artifacts, which makes it possible to significantly increase image clarity without increasing radiation exposure and to see the thinnest vascular structures and stents. The latest generation X-ray tube minimizes radiation exposure to the patient.
You can ask questions related to angiographic and X-ray endovascular interventions at Medservice LLC:
Tel., email mail
Ivanov Andrey Gennadievich (head of the department of x-ray surgical methods of diagnosis and treatment, doctor of the highest category in the specialty “endovascular diagnostics and treatment”)
Therapeutic tactics
When lesions of the brachiocephalic vessels are detected, specialists traditionally choose conservative treatment tactics. It involves taking certain medications (anticoagulants or antiplatelet agents), vitamin therapy, and diet therapy. The patient is given detailed recommendations regarding lifestyle and nutrition correction. He is obliged to control the level of cholesterol in the blood, as well as monitor the condition and stability of blood pressure.
Surgical intervention as a therapeutic tactic is chosen in conditions of a direct threat of stroke. If there is no immediate risk, the patient is registered and observed.
Surgical intervention happens:
- Open (resection of the affected arterial section with its immediate prosthetics or suturing);
- Endovascular (introduction of a stent into a vessel).
The category of open interventions includes endarterectomy (carotid eversion).
Stenting is a more modern, atraumatic and effective method, but it is acceptable and not indicated in every case. The later you seek professional medical help, the less likely you are to be cured using these methods.
Diseases of the brachiocephalic arteries are a serious disorder leading to unpredictable consequences. We urge you to promptly contact vascular surgeons with alarming symptoms in order to avoid the need for aggressive treatment and save your life.
After operation
In the postoperative period, the patient is prescribed antiplatelet therapy - drugs that “thin” the blood. These drugs should be taken only as prescribed by a doctor with strict adherence to the dosage and regimen. Self-cancellation or replacement with other drugs without a doctor’s prescription is unacceptable .
Otherwise, the postoperative period after surgery on the carotid arteries does not differ significantly from any other operations: limiting physical activity, wound care. You can read more about the postoperative period in the article: “How to behave after surgery on the arteries.”
In the vast majority of cases, the operation is quite comfortable and well tolerated by patients.
A timely operation saved the lives of many thousands of patients. Remember, there is nothing more expensive than your life and health.