Translation of the presentation “Anomalies and normal variants of the intracranial arteries: proposed workflow for classification and significance.”
| Congress: | ECR 2016 |
| Poster No.: | C-0199 |
| Authors: | A. Hakim1, J. Gralla1, C. Rozeik2, P. Mordasini1, F. Pult1, L. Leidolt1, E. Piechowiak1, K. Hsieh1, M. El-Koussy1; 1Bern/CH, 2Loerrach/DE |
| DOI: | 10.1594/ecr2016/C-0199 |
| DOI-Link: | https://dx.doi.org/10.1594/ecr2016/C-0199 |
Translation into Russian: Simanov V.A.
1.1. Variants of origin (discharge) of vessels
1.1.1. Common origin : two different vessels can have the same origin (discharge)
SCA/PCA: 2-22% Fig.3 :
The common trunk arises from the basilar artery, then branches into the posterior cerebral artery (PCA) and the superior cerebellar artery (SCA) [1].
PICA / AICA: common option Fig. 4 :
The anterior inferior cerebellar artery (AICA) shares a common trunk with the posterior inferior cerebellar artery (PICA) [2].
1.1.2. Funnel: 7-15% Fig.5 :
It is a funnel-shaped dilatation of the vessel at the origin. Its diameter should be no more than 3mm. It is most common at the origin of the posterior communicating artery (Pcom). A similar variant has also been described in the anterior communicating artery (Acom), ophthalmic artery and anterior choroidal artery [2].
1.1.3. Abnormal origin (discharge) due to persistent fetal circulation:
Fetal type PCA:
The posterior communicating arteries are the terminal branches of the basilar artery. During development, RCAs originate from the internal carotid artery (ICA). This variant, if it persists into the postnatal period, is called “fetal origin.” This option can be classified into two subtypes: Fig. 6
- Complete fetal PCA: 4-26% unilateral, bilateral 2-4%. PCA is entirely derived from the ICA. The P1 segment is absent, i.e., only the ICA supplies the occipital lobes [3]. In bilateral complete fetal type PCA, the basilar artery may be hypoplastic Fig. 7 .
- Partial fetal PCA: 11-29% unilateral, 1-9% bilateral. The P1 segment is still present, but is smaller or equal in diameter to Pcom, i.e. Most of the blood supply to the occipital lobes comes from the ICA[3].
Persistent dorsal ophthalmic artery (PDOA): 1.1% Fig.8, Fig.46 :
During embryonic development, the orbit is supplied with blood through the anterior and posterior rami, which originate from the ICA. Typically, the posterior branch is obliterated, while the anterior branch continues to supply the orbit. However, with this option the opposite happens. The PDOA enters the orbit through the superior orbital fissure [4].
The ophthalmic artery can also arise from other parts of the ICA, including the cavernous segment, in 8% of the population [2] Fig. 9 .
MMA from the orbital artery: 16% Fig. 10 :
During embryogenesis, the middle meningeal artery (MMA) arises from the stapedial artery. The stapedial artery gives off branches to the ECA. One of these branches is the supraorbital artery, which forms an anastomosis with the developing ophthalmic artery. Along this anastomosis, failure of segmental regression or persistence of segments that should regress leads to a number of anomalies, such as the origin of the MMA from the ophthalmic artery [2]. In this case, the foramen spinosum will be absent.
Fig. 3 TOF MRA, common trunk of PCA and SCA (red arrow) and ipsilateral dominant vertebral artery (white arrow)
Fig. 4 3D TOF MRA of the AICA (white arrow) extending caudally, supplying the PICA territory. Note the absence of PICA ipsilaterally. The contralateral PICA is present (green arrow).
Fig. 5 3D TOF MRA, funnel-shaped expansion (funnel) at the origin of Pcom (arrow).
Fig. 6 3D TOF MRA, complete fetal PCA (white arrow) with P1 segment absence on one side and partial fetal PCA (red arrow) with P1 segment hypoplasia (green arrow) on the other side. Note fenestration of the proximal part of the P1 segment (blue arrow).
Fig. 7 3D TOF, complete fetal PCAs on both sides and hypoplastic basilar artery
Fig. 8 Persistent dorsal ophthalmic artery: MIP (a) and 3D TOF MRA (b) show the ophthalmic artery arising from the posterior surface of the ICA (arrow in a ) and marked in red ( b ).
Fig. 9 Cavernous origin of the ophthalmic artery: MIP TOF lateral view (a), 3D TOF MRA ventral view (b), and 3D rotational DSA lateral view (c) showing the ophthalmic artery (white arrow) arising from the lateral surface of the cavernous segment of the ICA . Note the incidentally discovered Pcom aneurysm (red arrow).
Fig. 10 DSA (a) showing the MMA (red arrow) arising from the ophthalmic artery (white arrow). MIP reconstruction in the CT bone window (b), showing the absence of the foramen spinosum on the left side. Foramen spinosum on the right side is marked for comparison (blue arrow).
1.2. Change in the number of vessels
1.2.1. Reducing the number of vessels
ICA agenesis: 0.01% Fig.11 , Fig.47 :
Around day 24 of embryogenesis, the ICA develops from the dorsal aorta and third arch. Subsequently, at approximately the 5th - 6th week, the base of the skull begins to take its shape. Thus, absence of ICA will result in absence of the carotid canal, identification of which is the most practical method in identifying this anomaly in a clinical setting. Typically, patients with ICA agenesis are asymptomatic due to well-developed collateral circulation through the ECA and vertebrobasilar system [2].
Aplasia of the A1 segment: 1-2%. Fig.12 and Fig.15 :
In this situation, both A2 segments are supplied by the existing A1 segment [2].
Azygos ACA: less than 1% Fig. 13 :
Both A1 segments form a common A2 segment, which supplies blood to both hemispheres[2].
Lack of Acom: 5% Fig.14 [2]:
Typically, the absence of the anterior communicating artery (Acom) is not easy to detect on time-of-flight MR angiography because the artery may be present but the flow signal is too weak to be visualized.
Lack of Pcom: 0.6% Fig.15 :
The posterior communicating artery (Pcom) is usually smaller than the P1 segment. Complete absence is rare [2].
Artery of Percheron: 4-11.5% Fig. 16 :
The thalamo-mesencephalic arterial supply can be divided into 3 types: type 1 is the most common, with perforating arteries on both sides arising from the P1 segments; type 2 , known as the artery of Percheron, arising from one of the P1 segments, supplying both sides; type 3 is an arch that connects both P1 segments and from which the perforating arteries arise [5].
1.2.2. Increase in the number of vessels
Incremental MCA: 2.7% Fig. 17 :
Literary definitions of accessory middle cerebral artery (MCA) and MCA duplication are quite dichotomous. In this paper, we use the definition of Teal et al., who limited the term “accessory MCA” to the branch arising from the anterior cerebral artery (ACA) and the term “duplicate MCA” to the artery arising from the distal segment of the ICA [6]. To distinguish an accessory MCA from a duplex one, the dominant vessel must be identified by carefully searching for the MCA bifurcation. Comparison with the contralateral side is also useful to find the level of ICA bifurcation [1].
Duplication: refers to two separate arteries that do not exhibit distal fusion. For example:
- MCA duplication: 0.2-2.9% Fig. 18 : MCA duplication is an artery that arises from the ICA and runs parallel to the main trunk of the MCA. This variant should not be confused with early branching of the MCA, in which a short single M1 segment is present. It should also not be confused with the anterior temporal branch, which often arises from the M1 segment.
- Acom doubling: 18% Fig. 19 [1].
- SCA doubling: 14% Fig. 12 [2].
Trifurcation:
- ACA trifurcation: 2-13% Fig. 20 : trifurcation refers to the presence of three A2 segments and is described by various names such as pericallosal triplex, arteria mediana corporis callosi and persistent primitive median artery of the corpus callosum [2]. Early origin of a frontopolar branch, for example from Acom, may appear as a third A2 segment.
MCA trifurcation: 12% Fig. 21 : The horizontal segment of the MCA is divided into superior and inferior trunks in approximately 78%. In 12% there is an additional (middle) trunk, this situation is called trifurcation, and the presence of more than 3 trunks, for example, quadrifurcation, is observed in approximately 10% Fig. 22 [2].
Fig. 11 Agenesis of the left ICA. TOF MRA (a), no signal from the flow in the left ICA. MIP CTA (c), CCA continues as ECA with no ICA. Bone window CT (b), absence of bony carotid canal on the left side. The normal carotid duct on the right side is marked with a red arrow for comparison.
Fig. 12 3D MRA, absence of A1 segment of ACA, both A2 segments extend from the contralateral side. Note the partial fetal PCA (white arrow), duplication of the superior cerebellar artery (blue arrow), and hypoplastic vertebral artery (red arrow) that terminates as the PICA.
Fig. 13 3D MRA, fusion of both A1 segments to form a single A2 segment (azygos ACA) (arrow).
Fig.14 3D TOF MRA, no Acom.
Fig. 15 3D TOF, absence of Pcom and A1 segment on one side. The significance of this option is that if the ICA is occluded on that side, there will be no possibility of collateralization through the circle of Willis. Incidental finding: aneurysm of the terminal portion of the contralateral ICA (arrow).
Fig. 16 MIP (a) and 3D TOF (b), type 2 thalamo-mesencephalic arterial supply (artery of Percheron) with a single arterial trunk (arrow) arising from the P1 segment, the branches of which supply blood to both sides.
Fig. 17 3D TOF, additional MCA (arrow) extending from the A1 segment.
Fig. 18 3D TOF of a duplicated MCA (red arrow) extending from the distal ICA. This artery should not be confused with the anterior temporal branch (white arrow), which is a common finding.
Fig. 19 3D TOF, Acom duplication (white arrows), proximal A2 segment fenestration (red arrow), A1 segment aplasia and complete fetal PCA (blue arrow).
Fig. 20 3D TOF, ACA trifurcation with three A2 segments (arrows), the third branch arises from Acom
Fig.21 3D TOF, MCA trifurcation with additional middle trunk.
Fig.22 3D TOF, MCA quadrifurcation.
1.3. Change in morphology
1.3.1. Hypoplasia
ICA hypoplasia: 0.079% Fig. 23 :
In contrast to agenesis, the thin vessel is identifiable. Again, skull base tomography is useful in visualizing the bony carotid canal, which is thinner than normal in hypoplasia [2].
Hypoplasia A1: 10% Fig.24 :
Asymmetry of A1 segments is observed in 80% of cases. Hypoplasia is defined when the vessel diameter is less than 1.5 mm [2].
Hypoplasia A2 (bihemispheric ACA): 7% Fig. 24 :
One of the A2 segments is hypoplastic. In this variant, the blood supply to the ipsilateral hemisphere occurs mainly from the contralateral (dominant) A2 segment [2].
Hypoplasia Pcom: 34% Fig.25 :
but complete absence is a rare finding [2].
Hypoplasia of the vertebral artery:
50% on the right side (left dominant), 25% on the left side (right dominant), 25% codominant. In approximately 0.2%, the vertebral artery ends in the PICA Fig. 12 and Fig. 26 [7] [2]
1.3.2. Hyperplasia
Hyperplasia of the anterior choroidal artery: 2.3% Fig. 27 :
The anterior choriodal artery arises from the posterior surface of the terminal segment of the ICA, distal to the origin of the Pcom. This is usually a small branch. If it is enlarged (hyperplastic), then it supplies blood to part of the territory of the posterior cerebral artery (occipitotemporal branch) [1, 2].
1.3.3. Early bifurcation (early division):
Early MCA bifurcation: This is a common finding Fig.28 :
The horizontal segment of the MCA is usually 12 mm long, but may be shorter, with early branching (bi- or trifurcation) [1].
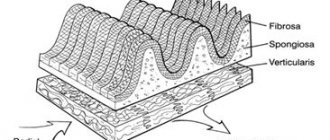
1.3.4. Fenestration: 0.7% including all intracranial vessels Fig. 6 , Fig. 19 and Fig. 29 . Fenestration is the division of the lumen of an artery into two separate channels. Each canal has its own endothelium and muscle layer and can separate the adventitia. These two canals merge distally. Fenestration is most often observed in the posterior circulation [1, 2].
- Fenestration A1: 0-4% [1]
- Fenestration A2: 2% Fig. 19 [1]
- Acom fenestration: 12-21% [1]
- Fenestration of the vertebral artery Fig. 29 : 0.3-2% [1].
Fenestration of the basilar artery Fig. 29 : 0.12-1.33%: the basilar artery is formed by the fusion of two longitudinal neural arteries. Incomplete fusion results in segmental fenestration, which is usually present in the proximal segment of the basilar artery [2].
Fig. 23 CTA (a), hypoplastic ICA (arrows). CT bone window (b) asymmetrical bony carotid canal
Fig. 24 3D TOF, hypoplasia of the A2 segment (white arrow) and the contralateral dominant A2 segment “bihemispheric ACA”. Note hypoplasia of the A1 segment (red arrow).
Fig. 25 MIP CTA, right Pcom hypoplasia (arrow). Note the pathological occlusion of the contralateral ICA.
Fig. 26 3D TOF, hypoplasia of the vertebral artery (white arrow) that ends as a PICA (green arrow).
Fig. 27 3D TOF, hyperplasia of the anterior choroidal artery (white arrow). The contralateral anterior choroidal artery is of normal caliber (green arrow). Red arrow points to fetal PCA, blue arrow to Pcom.
Fig. 28 3D MRA, early bifurcation with short prebifurcation segment M1 (arrow).
Fig. 29 Fenestration of the A1 segment (a), Acom (b), M1 segment (c), V4 segment (d) and the proximal part of the basilar artery (e).
Symptoms
As mentioned earlier, in the early stages, signs of hypoplasia may be completely absent.
The development of the pathological process can last for years and only when the arterial lumen narrows to a certain value will some symptoms appear. The paradox is that in the complete absence of manifestations of pathology in the early stages, the entry of the disease into the so-called active phase is accompanied by a rich clinical picture. However, in each patient with narrowing of the vertebral artery (right or left), symptoms manifest themselves completely differently:
- Headaches of different nature and specificity. Painful sensations can be periodic or constant, intensify after intense physical activity or occur at rest. With hypoplasia of the cerebral artery, the pain also differs in intensity, from strong, which has to be relieved with analgesics, to weak, which many tolerate without medication. As for the specifics, in most cases we are talking about dull and aching pain, however, they can also be sharp, stabbing.
- Unreasonable dizziness indicates cerebral circulatory disorders. This clinical sign is the second most common and also varies in nature. In some cases, dizziness is not associated with physical exertion, emotional state and other factors; they simply occur more frequently and disappear as quickly as they appeared. In other cases, dizziness begins after a change in body position, any load, stress, etc.
- Often hypoplasia of the right vertebral artery is accompanied by emotional disturbances. A person experiences frequent and sudden changes in mood, depression, which can last up to 2-3 days, then disappear without a trace, constant lethargy, states of apathy and even depressive states.
- If we talk about hypoplasia of the left vertebral artery, this form of the pathological process is more often characterized by changes in blood pressure. Yes, with right-sided hypoplasia they are also present in the clinical picture, but in this case they are noted more often.
- The pathology affects the patient’s body with a state of drowsiness, fatigue, and a feeling of weakness. People with hypoplasia do not get enough sleep even with a full, sound eight-hour sleep, are in a lethargic state, and often yawn.
- The pathology may be accompanied by disorders affecting the vestibular apparatus. In this case, dizziness is also present among the clinical signs, but they become more intense, and are accompanied by nausea, excessive sweating, and changes in skin color (pallor or, conversely, redness of the face). The clearest signs of damage to the vestibular apparatus and the progression of this pathology will be impaired coordination. A loss of balance appears, the gait becomes uncertain, the person sways from side to side, all movements become unclear, and loss of space may develop.
Over time, the symptoms worsen; severe forms of vertebral artery hypoplasia are accompanied by damage to the nervous system. On the one hand, this is expressed in numbness of certain parts of the body (usually limbs), on the other, visual hallucinations. In some cases, partial paralysis even occurs.
1.4. Changing the course
1.4.1. Aberrant lateral pharyngeal ICA, tortuous ICA, and kissing carotid arteries:
During embryonic development, the ICA is thought to begin to unwind as the dorsal aortic root descends into the thorax, providing a direct pathway for the ICA. Failure in unwinding results in tortuosity of the ICA, which runs close to the midline of the posterior pharyngeal wall, called the aberrant lateral pharyngeal artery [6].
This morphology is more commonly seen in older patients or those with hypertension, but should not be confused with the fetal variant, although both have the same meaning (see below). The incidence of aberrant lateral pharyngeal ICA is approximately 5%, but the exact prevalence of the anomaly is unknown as it cannot be differentiated morphologically from tortuosity. Studies conducted by Ekici et al. showed that the least affected age group with ICA tortuosity was the younger age group [8].
The term "kissing carotid arteries" describes the elongated carotid arteries that meet at the midline; can be observed retropharyngeal or intrasphenoidal / intrasellar Fig. 30 [2].
1.4.2. Persistent primitive olfactory artery: 0,14%
The ACA is derived from the primitive olfactory artery, which regresses to form the recurrent artery of Heubner. Violation of regression leads to preservation of the primitive olfactory artery. This artery has an extreme anterior-inferior course in the A1 segment, which moves along the olfactory tract before the posterosuperior transition to the A2 segment, forming a hairpin-shaped configuration [9].
1.4.3. Persistent embryological anastomosis
+ persistent carotid-vertebrobasilar anastomosis:
During embryonic development, the anterior circulation supplies the hindbrain through several anastomoses, since the posterior circulation is not yet sufficiently developed. After the development of the vertebral arteries, these anastomoses regress. Impaired regression results in abnormal communication between the anterior and posterior circulation in the postnatal period. The most common form of these anastomoses is the fetal type PCA (see variants of origin/origin of vessels). Recognizing the course of these abnormal vessels, as well as the level of entry into the skull, is critical for their differentiation Table 1
- persistent trigeminal artery (PTA): 0.1-0.2% Fig. 31 Fig. 48 : PTA originates from the cavernous segment of the ICA and communicates with the basilar artery. Proximal to the level of the anastomosis, the basilar artery is usually hypoplastic. On the angiogram, when viewed from the side, it has a characteristic “Trident of Neptune” or Tau sign configuration, reminiscent of the Greek letter “Tau” [1] [2]. There are two different classifications Table 2 Fig. 32 and Fig. 33 [10].
- PTA variants (Saltzman III): 0.18-0.76%: Arteries that supply the posterior fossa, arising from the precavernous segment of the ICA and not communicating with the basilar artery [1].
- Persistent auricular artery (otic artery): the rarest carotid-vertebrobasilar anastomosis. The existence of the auricular artery is controversial because it has not been identified in lower animals. It passes from the petrosal segment of the ICA to the basilar system through the internal auditory canal [2].
- Persistent primitive hypoglossal artery (PPHA): 0.03-0.26% Fig. 34 Fig. 49 : This artery runs from the cervical segment of the ICA to the basilar artery through the hypoglossal canal. The vertebral artery is hypoplastic. CT scan of the skull base shows an enlarged bony hypoglossal canal [1, 2].
- Proatlantal intersegmental artery: very rare. Connects the cervical segment of the ICA or external carotid artery (ECA) to the vertebrobasilar system. The artery enters the base of the skull through the foramen magnum, which allows it to be differentiated from the hypoglossal artery. There are two types:
- Type I: joins the vertebral artery above the atlas.
- Type II: enters the vertebral artery through the atlas [1, 2].
+ persistent internal-external carotid anastomosis
- Aberrant intratympanic ICA: very rare. This variant is an anastomosis between the ICA and the ECA, as it is believed to arise from agenesis of the cervical segment of the ICA and the development of an anastomosis between the horizontal (petrosal) segment of the ICA and the enlarged inferior tympanic artery, which is a branch of the ECA. The ICA (or rather the enlarged inferior tympanic artery) in this case has a smaller diameter than the usual ICA, with the absence of the ascending part of the carotid canal as it enters the base of the skull, posterior and parallel to the jugular bulb, which resembles a mass in the hypotympanum; there is also no bone plate between the carotid canal and the tympanic cavity [1].
- Persistent stapedial artery: 0.48%. This anomaly occurs due to the persistence of the anastomosis through the stapedial artery, which is usually present during development between the ECA and ICA. The artery arises from the petrosal segment of the ICA, passes through the obturator foramen, and ends as the MCA in the epidural space of the middle cranial fossa. A CT scan of the skull base may show a small canal near the carotid canal. Foramen spinosum, which contains MMA, will be absent. a persistent stapedial artery may be associated with an aberrant ICA [1, 2].
Table 3 shows the frequency of variants discussed, however, there are other rare variants that cannot be included in a single document. Finally, having a fully developed Circle of Willis can be considered an option since it is present in less than 50% of the population [2]
*NB: Frequency varies between authors depending on the type of study performed (CT, MRI, surgical or post-mortem). Frequency may also vary depending on geographic distribution; Published data may not always be applicable to other populations.
Table 1: Types of persistent carotid-vertebrobasilar anastomoses
Table 3: occurrence of anatomical variants
Fig. 30 Coronal MIP CTA of a patient with a history of hypertension shows elongated carotid arteries reaching the midline (“kissing” carotid arteries).
Fig. 31 3D TOF, lateral view (a) and dorsal view (b), persistent primitive trigeminal artery (red arrow) arising from the cavernous segment of the ICA and communicating with the basilar artery, which is hypoplastic to the level of the anastomosis (white arrow). In lateral view, the anomalous artery with ICA resembles Neptune's trident and the Greek letter "tau".
Fig. 32 MIP CTA of persistent primitive trigeminal artery (red arrow) in two different cases. According to Salas there are 2 types: medial sphenoidal or intrasellar (a), which extends into the sella turcica and perforates the dura mater or dorsum sella (green arrow), as in this case, and lateral petrosal or parasellar (b), in which the vessel goes with the sensory roots of the trigeminal nerve, on the side of the sella turcica.
Fig. 33 3D TOF showing two different cases of persistent primitive trigeminal artery (red arrow). Classification according to Saltzman: Type I (a), in which the PCA supplies the superior part of the basilar artery, including the posterior territory, and type II (b) with the fetal PCA (white arrow).
Fig. 34 3D CE MRA oblique (a) and posterior (b) views showing the persistent primitive hypoglossal artery (red arrow) which arises from the cervical segment of the ICA (green arrow) and continues as the vertebrobasilar artery (blue arrow). ECA is marked with a white arrow.
The problems of treatment and prevention of cerebrovascular diseases remain among the most pressing, since cerebral circulatory disorders continue to occupy a leading position among the causes of persistent disability and mortality throughout the world. Vascular diseases of the brain are the main cause of ischemic stroke. It has been proven that lesions of the extracranial parts of the internal carotid (ICA) and vertebral arteries in 65-70% of cases lead to ischemic disorders of cerebral circulation. Pathological deformations (PD) of the ICA are one of the most common diseases of the brachiocephalic vessels, second only to atherosclerosis in frequency. ICA PDs lead to cerebral circulatory disorders of varying severity [1–6]. The overall incidence of ICA PD among the adult population, according to the results of angiographic and pathomorphological studies, varies from 10 to 40%. In children with manifestations of brain failure, this pathology occurs in 14-30% [2, 7, 8].
The etiology and pathogenesis of ICA PD are not fully understood. Most authors believe that their origin may be congenital or acquired. Evidence of the congenital origin of PD of the ICA is the presence of deformations of the carotid arteries in childhood and young age, frequent bilateral lesions, a combination of lesions of the carotid arteries with other manifestations of systemic connective tissue dysplasia [9-11] - Marfan and Elars-Danlos syndromes [12], coarctation of the aorta, vascular hypoplasia [13-16]. The causes of acquired PD are considered to be weakening of the elastic frame of the artery wall, atherosclerosis, age-related changes in the cervical spine, hypertension, diabetes mellitus, and obesity [1, 2, 5, 17, 18].
Congenital PD of the ICA
occupy 1st place among the causes of cerebrovascular accidents in childhood. According to Yu.V. Smirnova [8], ICA PDs occur in 26.9% of children with neurological symptoms. M.A. Lobov et al. [7] identify PD as one of the main causes of vasopathic headaches in childhood, recording them in 1/3 of cases. The incidence of PD in boys and girls is comparable.
Initial manifestations of cerebrovascular insufficiency usually occur in children 4-6 years old. These include delayed speech development, late formation of self-care skills, impaired adaptation in a team, hyperexcitability and irritability. Later, at 5-6 years of age, headaches appear. The described symptoms are nonspecific and can mask vascular anomalies of the carotid arteries, so ultrasound examination of the neck vessels is mandatory in the presence of such a clinic. Acute cerebrovascular accidents in children occur quite rarely: transient cerebrovascular accidents - in 4.3% of cases, ischemic stroke with the development of focal lesions of the brain substance is observed even less often - in 2.1% [7, 8, 10, 15-17] . A feature of the clinical picture of PD in children is epileptic seizures (in 19.3% of cases).
The predominant types of ICA PD are couling, C- and S-shaped tortuosity (20-30%). This is explained by intrauterine development disorders [1, 13, 18-20]. Back in 1925, A. Kelly [21] believed that loops are formed at the 5-6th week of embryo development. The ICA originates from the third branchial arch and the dorsal aorta, at the junction of which a distinct bend is formed, which appears in a 5-week embryo. In the process of further development of the fetus, due to the lowering of the heart into the chest cavity and its vertical rotation along the axis, the carotid artery straightens. If this straightening or turning is incomplete, this leads to the formation of bends, loops, and kinks of varying degrees of severity. Another contributing factor to the deformities may be the more pronounced growth of the arteries of the aortic arch compared to the growth of the neck. This is confirmed by the presence of tortuosity of the ICA in embryos and children at the level of the glossopharyngeal nerve [13, 19]. The frequency of such anomalies in newborns ranges from 5 to 10% [2, 10, 11].
There are no data in the literature on the etiological factors leading to disembryogenesis and the development of congenital vascular deformations. It should be noted that bends and loops can also be found in the cerebral, coronary, retinal and vertebral arteries, but they are more often acquired. Bends of the coronary arteries are associated with hypertension and myocardial infarction, retinal arteries with retinopathy in malignant hypertension and diabetes mellitus, capillaries of the muscles and heart with arterial hypertension and diabetes mellitus, and veins with varicose veins [22].
B. Callewaert et al. [23] describe a special “arterial tortuosis syndrome”. This is a congenital disease with an autosomal recessive mode of inheritance (defect of the SLC2A10
), which is characterized by tortuosity, elongation and the formation of aneurysms of large arteries due to disruption of the structure of the elastic fibers of the media of the vascular wall. The combination of tortuosity and arterial aneurysms is the main feature of Loeys-Dietz syndrome, a congenital disease with a mutation in the TGF β receptor. In this case, the aneurysm is primary and becomes the background for the development of tortuosity.
Yu.V. Smirnova [11] proved that the trait of tortuous ICA can be inherited in an autosomal dominant or autosomal recessive manner. An association has been established for the A80807T polymorphism of the transcription factor 8p4
with pathological tortuosity of the carotid arteries. The probability of having PD ICA in A80807/A80807 homozygotes is 1.64 times higher compared to carriers of the other two genotypes (A80807/T80807, T80807/T80807).
M.A. Lobov et al. [10, 24] also indicate the hereditary determination of ICA PD in children. According to them, the frequency of familial cases is 50%. Segregation analysis of these cases demonstrates that ICA PD can be either isolated or a manifestation of hereditary syndromic connective tissue pathology. The segregation frequency is 45% [24]. Researchers regard hypoplasia, aplasia and anomalies in the position of arteries as nonspecific signs of dysembryogenesis and classify them as precerebral angiodysplasias.
In recent years, the role of congenital connective tissue deficiency in the formation of ICA PD has been discussed. Clinical observations of a combination of elongation and deformation of the carotid and vertebral arteries with phenotypic signs of hereditary connective tissue pathology, Elars-Danlos, Marfan, Sturge-Weber syndromes are presented [5, 9, 12, 15]. At the same time, combinations of ICA PD with the above syndromes are described in isolated cases. It should be noted that there is a higher incidence (60%) of minor forms of connective tissue dysplasia in children with PD ICA, such as joint hypermobility, skin hyperextensibility, muscle hypotonia, poor posture, flat feet, mitral valve prolapse, abnormal chordae, abnormal growth and development of teeth. However, the degree of “phenotypic intensity” of the signs does not reach the severity corresponding to the established criteria for diagnosing connective tissue pathology syndrome [24]. Therefore, the question of whether ICA PD in children can be considered a manifestation of connective tissue dysplasia syndrome remains open.
The pathomorphological signs described by P.O. support the dysembryogenetic theory of the origin of the ICA PD. Kazanchyan et al. [1], including degenerative changes in elastic fibers, compensatory hyperelastosis, multiplication of the internal elastic membrane, development of mucoid edema, proliferation of smooth muscle cells.
The most acceptable hypothesis for the pathogenesis of carotid artery anomalies is the appearance of defects in the structure of elastin and collagen due to an endogenous or genetically determined increase in the activity of degradative enzymes - collagenase and elastase [20, 25-27]. It is advisable to emphasize that the same changes in the structure of elastin and collagen are considered the main pathogenetic factor in the development of vascular pathology - both congenital and acquired.
A possible reason for the development of ICA PD in children may be birth trauma or overstretching of the neck structures during childbirth. It is known that collagen fibers under conditions of uniaxial tension are the main factor preventing deformation. Collagen concentration correlates positively with tensile strength and negatively with maximum elongation. The experiment proved that when collagen is removed from the vascular wall, the tensile strength and rigidity decrease, and when elastin is removed, the wall strength and relative deformation decrease. The significant content of elastin in the wall of the carotid artery determines its greater elasticity reserves compared to the vertebral artery. O.V. Kalmin [28] proposed a hypothesis about the sequence of damage to neck structures during hyperextension, hyperflexion and longitudinal stretching during childbirth. Nerve trunks have relatively low extensibility and the least rigidity, and the wall of the common carotid artery (CCA), on the contrary, has the greatest extensibility and the least rigidity. With hyperextension, the phrenic nerve is at greatest risk of injury, followed by the vagus nerve, and damage to the carotid artery wall is unlikely. With hyperflexion, the spinal cord can be damaged first, and only after the spinal ligaments are torn, massive damage to the arterial walls will occur. With longitudinal stretching of the neck, the main part of the deforming load will fall on the vertebral trunk and its ligaments, then the nerve trunks, the vertebral artery and, lastly, the carotid artery. The greatest reserve of lengthening - 33.8%, without disturbing the structure and functions of the neck structures, is found in the OCA. Based on the above, it follows that damage to the CCA during childbirth is unlikely [1, 18]. At the same time, the ICA remains outside the attention of researchers. During longitudinal stretching during childbirth, the greatest load, in our opinion, occurs at the site where the carotid artery enters the skull, which can lead to the development of deformities.
The question of the advisability of surgical intervention for ICA PD in children remains open. There is evidence that in some children, during the process of growth, the straightness of the course of the vessel is restored, and in some patients, the deformity remains with the leveling of local hemodynamic disturbances [1, 8]. It should be taken into account that generalized epileptic seizures, which often occur with anomalies of the carotid arteries, are a contraindication to surgery [6, 8, 11]. Conservative therapy is still considered the priority direction for treating children [7, 15, 17]. If it is ineffective, neurological symptoms increase and the rate of cerebral blood flow decreases, surgical intervention is necessary. Reconstructive elimination of deformity leads to a reduction in the manifestations of chronic brain failure in the immediate postoperative period in all patients [2, 4]. At the same time, among the literature data, we did not find any scientific studies assessing the impact of surgical or conservative treatment of children with ICA PD on their quality of life in the postoperative period.
Acquired pathological deformations of the ICA occupy 2nd place among the causes of ischemic cerebrovascular accidents, second only to atherosclerosis [1, 4-6, 18, 20, 22, 25]. ICA PDs occur predominantly in patients over 60 years of age. It is believed that kinking is detected in 5-16% of patients, more often in men [1, 4, 29, 30], although there are reports of predominant lesions in women, which is explained by damage to the elastic framework of blood vessels associated with hormonal changes [31-33] . L. Del Corso et al. [34] based on a study of 469 patients with PD (tortuosity, kinking and bending) confirm the high incidence of lesions among women. E. Ballotta et al. [35] believe that in women, asymptomatic carotid kinking progresses with age and becomes symptomatic after 60 years. R. Zanetti et al. [6] indicates that in adults, changes in the length and shape of the carotid arteries most often appear in the sixth decade of life, with a male to female ratio of 4:1. Perhaps such disagreements are associated with the presence of concomitant pathologies in patients - atherosclerosis, hypertension, diabetes mellitus, hyperlipidemia, hormonal changes, as well as the influence of toxic substances and smoking.
The clinical picture is characterized by cerebrovascular accidents. The most common symptoms are dizziness, cochlear, sensory and cognitive impairment, and ischemic retinopathy. Symptoms of cerebral ischemia in the hemisphere on the side of the ICA tortuosity occur in 26% of patients, cerebral manifestations in 41.75%, and their combination in 27.5%. There is evidence that the clinical picture depends on the type of ICA PD. C- and S-deformations most often occur asymptomatically - about 70% of cases; kinking, loop- and spiral-shaped tortuosity have pronounced clinical symptoms - in more than 80% of cases [18, 35, 36]. The development of symptoms also depends on the severity of the angle in the kinking segment - the sharper the angle, the more severe the lesions. When the angle is less than 45°, all patients experience severe brain symptoms requiring surgical intervention [18, 19, 36].
Among the types of ICA PD, kinking, elongation, and kinks are most often described, which is associated with the peculiarities of the origin of acquired deformities. So, Z.K. Mackevicius et al. [37] identify a group of causes of ICA PD, dividing them into 2 subgroups. The first is a bend at the site of the carotid artery in the area where the atherosclerotic plaque ends, the second is bends and deformations based on age-related destructive changes in the muscular-elastic frame of the arterial wall. Arterial hypertension that appears with age contributes to the worsening of PD, since vascular deformations become a functional device to reduce the pulse wave and ensure uniformity of blood flow [4, 19, 25]. However, P.A. Pauliukas and E.M. Barkauskas [29] believe that in these cases hypertension is secondary, has a reflex nature and develops in response to cerebral ischemia. As hemodynamic studies show, when kinks and loops of brachiocephalic vessels are eliminated, systemic blood pressure decreases [5, 9, 18, 25].
According to N.V. Vereshchagin and A.N. Koltover [20], hypertension is the primary cause of ICA PD. In response to increased pressure in the walls of the carotid arteries, adaptive changes occur in the form of focal and circular muscular-elastic thickening of the intima, sclerosis of the inner and middle membranes with destruction of the elastic frame. As sclerotic changes develop, the muscular and elastic elements of the arteries are lost, their tone is lost, resulting in the formation of pathological tortuosity and kinks of these vessels with pronounced septal stenosis against the background of arterial hypertension. The latter, by limiting blood flow, can act as an independent pathogenetic factor in cerebrovascular accidents. Hypertension, according to J. White et al. [27], leads to stretching of the smooth muscle cells of the vessel media, loss of elastin and fragmentation of elastomers. The progression of these processes causes pathological lengthening of the vessel. Data from P. Pancera et al. [38] demonstrate a clear predominance of hypertension in patients with kinking compared with individuals without vascular anomalies. However, D. Radak et al. [39] believe that there is still no clear understanding of the pathogenetic relationship between known vascular risk factors and the development of kinking.
The main reason for the development of acquired ICA PD in patients over 60 years of age is atherosclerosis. The question remains open: what comes first, atherosclerosis or PD? There is no consensus among researchers on this matter. Some believe that atherosclerosis leads to the development of destructive changes in the elastic framework of the vessel and, together with arterial hypertension, contributes to the development of deformations, such as elongation and kinking [4-6, 19, 20, 22, 31, 32, 37, 40-42]. Other authors call atherosclerosis an aggravating disease in ICA PD. Disruption of local hemodynamics in the bending zone of a deformed vessel leads to intimal injury, damage to the endothelium and the initiation of the pathological process [1, 5, 20, 29, 34, 38]. Based on this, early atherosclerosis should develop in the carotid arteries, clinically and angiographically manifested before the age of 40 years, which is not confirmed by literature data [2, 19, 37, 40, 41]. Other researchers have proven that when bending, a pressure difference is created at the outer and inner radius, leading to the development of turbulence in hemodynamic flows and, as a consequence, the growth of endothelium and connective tissue in the vessel. At the same time, signs of proliferative sclerotic remodeling are found in the vessel due to activation of the immune system - high apoptotic activity of smooth muscle cells and the development of chronic inflammation in the tortuosity zone [42]. At the same time, in a series of morphological studies there is no data on inflammation and the presence of vasculitis [20, 37, 38, 43].
It is important that it is atherosclerosis in PD that increases the risk of stroke several times. This combination is observed in 40-70% of patients with cerebrovascular accidents [1, 4, 19, 22, 31, 34, 38, 41, 43].
Fibromuscular dysplasia is considered one of the important causes of the development of ICA PD. There are no exact data on the incidence of dysplasia in PD ICA. It is believed that fibromuscular dysplasia and PD of the ICA occur more often in middle-aged people, although there is data on patients over 60 years of age. The mechanism of development of deformations of the carotid arteries in this disease is unknown. Fibromuscular dysplasia is a non-atherosclerotic and non-inflammatory arterial disease with predominant involvement of the renal arteries and ICA, developing predominantly in young women. The predominant pathomorphological variant of carotid artery lesions in fibromuscular dysplasia without PD is medial fibroplasia. It is characterized by fibrosis with partial or total damage to the media, complete or partial loss of elastic fibers. This leads to the formation of multiple aneurysms, as a result of which the vessel resembles a “string of beads.” In addition to the development of aneurysms, vascular dissection, occlusion of the vascular lumen, and vascular ruptures are possible. It can be assumed that the commonality of the pathological process in fibromuscular dysplasia and PD of the ICA—the loss of the elastic framework of the vessel—is probably a significant factor for the development of pathological bends in fibromuscular dysplasia [44–47].
Age-related changes in the vertebrae of the cervical spine are considered an important factor in the development of acquired ICA PD. Vertebrogenic compression contributes to hemodynamic disturbances and the development of ICA PD. In patients with tortuosity, there is a forward displacement of the head, smoothing of the cervical lordosis, kyphosis in the thoracic region, and pronounced tension in the sternocleidomastoid, scalene muscles, and muscles located above and below the hyoid bone. Shortening of the muscles of the anterior surface of the neck and deformation of the fascia lead to extravasal effects on the carotid and vertebral arteries [18, 48]. Thus, mechanical deformations of the fascia against the background of disorders in the cervical spine can be considered as one of the reasons for the formation of arterial deformities. R. Wirbel et al. [49] proved that hyperextensional and rotational effects on the cervical spine, which occur during manual therapy sessions and sports, such as wrestling, can lead to damage to the vertebrobasilar vessels. A number of authors believe that although most injuries to the vessels of the neck occur for no apparent reason to the patient, minor trauma to the cervical spine is detected in 80% of cases [50]. With significant displacements of the vertebrae or their parts, sharp changes in the normal course of blood vessels are detected, while twisting, compaction and overstretching of the vertebral and carotid arteries are macroscopically observed.
Other causes of ICA PD include diabetes mellitus, hyperlipidemia and other vascular risk factors [2, 5, 6, 20, 34, 38, 41].
Possible factors contributing to the development of ICA PD include smoking, taking contraceptives, and toxic influences [5]. According to the new theory of D.D. Zerbino [51, 52], heavy metals damage the muscular-elastic framework of arteries and lead to the development of arteriosclerosis and arterial hypertension [51]. It has been proven that the toxic effects of cadmium lead to massive elastolysis of the media due to the activation of elastases and the development of aortic aneurysms. It is known that heavy metals contained in cigarettes cause irreversible changes in the coronary arteries, leading to the development of atherosclerosis and myocardial infarction in patients under 40 years of age. Smoking and many years of professional contact with toxic substances are important reasons for the development of vascular pathology in middle age.
Some authors mention vasculitis among the possible causes of the development of ICA PD in young patients [20, 37, 43]. Z.K. Matskevichus and P.A. Pauliukas [37] describe angiitis vasa vasorum
, which is explained by ischemic damage
to the vasa vasorum
with the development of inflammation and subsequent severe sclerosis.
The mechanism of development of ICA PD in patients aged 40–50 years remains unclear. The prevailing opinion in the literature is that they are a consequence of impaired embryogenesis [2, 5, 22, 32, 35, 43]. Based on the above, it follows that congenital deformities in children are characterized by loop-shaped deviations (cowling), C- and S-shaped tortuosities, and for patients over 60 years old - kinking, elongations and kinks. Whether it is possible to transition from one type of PD to another remains unexplored.
Yu.V. Rodin et al. [53], using mathematical modeling methods, a hypothetical assessment of the development of S-shaped tortuosity was given - any bend, under certain conditions, tends to an angular bend. The results obtained are also valid for other types of crimp, since they typically contain S-shaped crimp. At the same time, this hypothesis completely refutes the possibility of the transition of one type of tortuosity to another and requires further research.
The pathomorphological picture of ICA PD is characterized by pronounced sclerotic changes in the vessel wall, destruction of the elastic frame, and proliferation of connective tissue around the vessel [13, 20, 37, 38]. Since such changes contribute to stable irreversible deformities that increase with age, the question of whether changes in the configuration of deformities is possible remains open.
Surgical intervention is recognized as the most effective treatment method for acquired ICA PD. The indication for surgery is considered to be a hemodynamically significant PD of the ICA, commensurate with circulatory disorders characteristic of stenoses of 70% or more, regardless of the presence of neurological symptoms and/or hemodynamically significant atherosclerotic stenosis, as well as embologenic plaques that stenose the lumen of more than 50%, and plaques with pronounced surface and parietal thrombosis. The high effectiveness of surgical intervention in patients with symptomatic ICA deformities is known, while the question of the appropriateness of surgical intervention in patients with asymptomatic deformities remains open [1, 3, 4, 6, 19, 29, 35, 36, 42, 54].
In conclusion, we would like to mention that a comparative analysis of the literature on congenital and acquired ICA PDs showed that they have many distinctive features not only in origin and pathogenesis, but also in clinical presentation, treatment and prognosis. It is appropriate to assume that congenital and acquired ICA PD are two different diseases, the relationship between which has not been proven.
This review of the literature demonstrates the relevance of studying this disease, the presence of unresolved and controversial issues not only in the genesis, but also in the treatment tactics of patient management, and the need for a comprehensive clinical and pathomorphological study of this important vascular pathology.
Meaning
The list in Fig. 35 shows the values of the anatomical options.
2.1. Recognition of anatomical patterns and the ability to distinguish them from pathological changes:
2.1.1. Knowledge of normal variations is part of the anatomical knowledge that is important for every radiologist and surgeon. Knowledge of normal variants and their proximity to other structures facilitates the understanding and diagnosis of various diseases, such as:
- Trigeminal neuralgia, which can be caused by the presence of a variant of PTA (less commonly PTA), due to the proximity of the vessel to the trigeminal nerve [11].
- Glossopharyngeal neuralgia or hypoglossal nerve palsy, which can be caused by a persistent hypoglossal artery [1].
- Pulsatile tinnitus in cases of persistent stapedial artery [1].
2.1.2. Option against pathology:
- Infundibulum: The Pcom infundibulum should not be confused with an aneurysm Fig. 36 .
- ICA hypoplasia may be confused with dissection or fibromuscular dysplasia, while ICA agenesis may be confused with occlusion. Visualization of the skull base aids differentiation, as the bony carotid canal will be narrow in cases of hypoplasia and absent in cases of agenesis, but will appear normal in other acquired diseases Fig. 11 and Fig. 23 .
- Different patterns of perfusion abnormalities may occur with normal variations that can cause confusion, especially in the context of stroke:
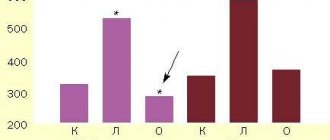
- Asymmetry of CT or MR perfusion in the occipital lobes, in the case of unilateral fetal PCA. The contralateral side may show delayed perfusion because it is supplied by the posterior circulation Fig. 37 .
- Bilateral perfusion delay in the occipital lobes compared with the frontal and parietal lobes may be observed in the absence of bilateral Pcom Fig. 38 .
- Relative hypoperfusion in the PICA territory in cases of vertebral artery hypoplasia. Hypoperfusion may present as prolonged time-to-peak, prolonged main transit time, or decreased cerebral blood flow, but it never affects cerebral blood volume ) Fig.39 [12].
2.2. Hemodynamic effect of normal variants and abnormalities:
2.2.1. Understanding collateral function: The presence of hypoplasia or aplasia of segment(s) in the circle of Willis can affect collateral function when one or more arteries are occluded Fig. 15 .
2.2.2. Explains unclear cases of stroke:
Vascular conditions that cause changes in unexpected vascular territories can be explained by normal variations such as:
- Ischemia in the posterior territory may accompany ICA pathology due to the presence of fetal PCA Fig. 40 .
- Bilateral ischemia and ischemia in certain areas may draw attention to the presence of pathology in one of the options, such as:
- Bilateral anterior infarction in case of thromboembolism of azygos ACA or dominant bihemispheric ACA Fig. 41 .
- Bilateral mesencephalothalamic infarction with Percheron's artery Fig. 42 .
2.3. Association with vascular and nonvascular congenital anomalies and other diseases:
2.3.1. Association with aneurysms: Changes in vascular anatomy may be a sign of lack of vascular maturity and vulnerability to aneurysm formation. In the work of Lazzaro et al., normal variants of the circle of Willis were more common in cases with ruptured aneurysms than in cases of unruptured aneurysms [13]. Based on a review of the literature, the following variants and abnormalities were associated with aneurysms: Table 4 Fig. 43
- Fenestrations: The incidence of aneurysms (IoA) is approximately 7% of all fenestrations. A defect in the media of the fenestrated segment and turbulent flow at both ends of the fenestration can lead to aneurysm formation. Additionally, in the work of Hudák et al., fenestration was a common finding in patients with unexplained subarachnoid hemorrhage due to a weak arterial wall [1] [2] [14]
- ICA agenesis and hypoplasia: IoA 67% [2].
- A1 segment aplasia: IoA14% [15].
- Azygos ACA: IoA 41%. Due to increased flow from both segments of A1 [2].
- Persistent dorsal ophthalmic artery: IoA 45% [4].
- Persistent primitive olfactory artery: In the work of Uchino et al, 2 intracranial artery aneurysms were found in 14 patients with PPOA (IoA about 14%); one of them is in the hairpin bend (7%) [9].
- PTA: IoA 14% [1].
- Persistent hypoglossal artery: IoA 26% [16].
- Proatlantal intersegmental artery: IoA 10% [1, 2]
- Other variants and anomalies associated with aneurysms whose cases have been reported but not available include infraoptic ACA, superior anterior communicating artery, accessory MCA, MCA aplasia, variant PTA, and asymmetry of the circle of Willis [1, 2].
2.3.2. Association with other vascular anomalies and diseases:
- Fenestration of the vertebral artery is associated with arteriovenous malformation in 7% [6].
- PTA is observed in vascular anomalies such as AVM, carotid-cavernous fistula, and Moyamoya disease in 25% of cases [17].
- Proatlantal intersegmental artery: The incidence of cerebrovascular disorders such as AVM, vein of Galen malformation and aortic arch variants is 59% [18].
- Spontaneous vertebral artery dissection was slightly more common in subjects with hypoplastic vertebral artery than in controls (30.4% vs. 17.4%). It was also found that spontaneous vertebral artery dissection occurs more often with hypoplastic vertebral arteries than with dominant vertebral arteries (68% versus 32%) [19].
2.3.3. Association with other congenital anomalies:
- Azygos ACA may be associated with holoprosencephaly and migration abnormalities Fig. 44 [1].
- ICA hypoplasia is associated with anencephaly and basal telangiectasia [2].
- Fenestration of the vertebral artery may be associated with vertebral fusion [6].
2.3.4. Association with other disorders:
- Pituitary dysfunction and acromegaly in intrasellar “kissing” carotid arteries[2].
- It was found that migraine with aura is more common in patients with an open circle of Willis [20].
2.4. Preoperative planning for cranial surgery, head and neck surgery, and neurointerventional procedures:
The description of normal variations is very important for surgeons and interventional radiologists, as some of these variations must be considered to avoid catastrophic consequences during intervention.
2.4.1. The risk of catastrophic hemorrhage exists in the following cases:
- Transsphenoidal pituitary surgery in cases of PTA or intrasellar “kissing” carotid arteries.
- Middle ear surgery in cases of persistent stapedial artery and aberrant intratympanic ICA.
- Pharyngeal surgeries such as otopharyngeal tumor resection, tonsillectomy, adenoidectomy and palatopharyngoplasty in cases of aberrant lateral pharyngeal artery.
2.4.2. Knowledge of normal variations is important in interventional procedures. This knowledge may help to gain vascular access, such as dominant versus hypoplastic vertebral or variant access, or avoid complications during procedures such as tumor embolization through ECA catheterization in cases of MMA arising from the ophthalmic artery, which can lead to blindness . Fig.45 Fig.50
2.4.3. The presence of persistent carotid-basilar anastomoses should be excluded before certain procedures, such as the Wada test: in this case, injection of amytal can lead to loss of consciousness and apnea [2]
Fig.35 Meaning of normal options
Table 4: Variants associated with aneurysms and their occurrence
Fig. 36 3D TOF MRA, funnel-shaped dilatation with origin of Pcom (white arrow), which should not be confused with an aneurysm. Note the small aneurysm at the origin of the contralateral Pcom (red arrow). Also note the trifurcation of the ACA.
Fig. 37 MR perfusion, TTP map (a) shows slow perfusion in the left occipital lobe; no abnormalities were found in other perfusion parameters. 3D TOF (b), showing fetal PCA on the contralateral side (arrow).
Fig. 38 TTP perfusion map (a) shows a symmetrical delay in the occipital lobes, no deviations in other perfusion parameters were noted. 3D TOF shows no Pcom on both sides.
Fig. 39 (same patient as in Fig. 12) with hypoplasia of the right vertebral artery, which ends as the PICA. TTP map shows perfusion delay in the territory of the right PICA. An examination performed 6 weeks later for other reasons (not shown) showed no pathology in this area.
Fig. 40 MRI of a 56-year-old patient complaining of headache shows dissection of the left ICA (red arrows) with intramural hematoma on T2 (a) and T1FS (b). DWI (c) and ADC (d) show subacute infarction in the territory of the left PCA, which is due to the presence of fetal PCA (TOF not shown).
Fig.41 72-year-old patient with hemiplegia, epilepsy and impaired consciousness. DWI (a) and ADC (b) show bilateral infarcts in the ACA territory. DSA (c), shows proximal occlusion of the azygos ACA (arrow).
Fig. 42 Bilateral acute thalamic infarctions on DWI (a). DSA shows occlusion of the P1 segment of the left PCA (b). Minimal recanalization after intra-arterial thrombolysis (c), with mild opacification of the artery of Percheron (arrows) arising from the left PCA.
Fig. 43 Aneurysms (arrows) associated with abnormalities; a) A1 aplasia with Acom aneurysm. b) Azygos ACA with pericallosal aneurysm. c) fenestration of the basilar artery with proximal basilar aneurysm after coiling.
Fig. 44 Axial (a) and sagittal (b) MRI images of a child with holoprosencephaly, anterior cingulate fusion, and abnormal beak and genu corpus callosum. Note the empty flow of the anterior cerebral artery (arrow), which is single (azygos) and displaced anteriorly.
Fig. 45 55-year-old patient involved in an accident. Initial CT scan (a) shows a fracture of the left temporal bone. She later complained of pulsating tinnitus. DSA (c) with flat panel CT angiography (b and d) was performed. Reconstructed images showed the middle meningeal artery (yellow arrows) arising from the ophthalmic artery (blue arrow) and the traumatic AVM (red arrows) draining into the external jugular vein to form an aneurysm (orange arrow). Knowledge of this option is important when planning therapy.
Symptoms of the disease
Underdevelopment of the vertebral artery limits blood flow through it to the posterior structures of the brain. This is especially dangerous when turning or tilting your head.
At this time, additional pressure on the segment of the vessel, which is located between the arches of the cervical vertebrae, can cause a reflex spasm. With age, atherosclerotic processes further disrupt blood flow. Despite this, not all developmental anomalies are accompanied by symptoms, since the movement of blood through the second, paired artery increases compensatoryly, it acquires a larger diameter and takes on the main load. If pathological narrowing limits the nutrition of the brain, then manifestations of vertebral artery syndrome occur:
- migraine-like pain in the back of the head, dizziness, tinnitus, blurred vision, frequent vomiting, the appearance of sparkling spots or rainbow arcs before the eyes;
- pain in the cervical-occipital region with transition to the frontal parts of the head, it becomes stronger after sleep, especially in an uncomfortable position, with sudden movements of the head, jumping, sports training, shaking in transport;
- dizziness when turning the head with nausea, darkening of the eyes, unsteadiness, loss of balance;
- rapid fatigue during visual stress, the appearance of dark or bright spots, flashes of light (“sparks in the eyes”);
- redness of the eyes, foreign body sensation;
- tinnitus, hearing impairment, difficulty perceiving speech against a background of complete silence;
- hot flashes, sweating or chilliness of the hands and feet;
- difficulty breathing, rapid heartbeat, fluctuations in blood pressure;
- insomnia.
More dangerous signs include transient attacks of cerebral ischemia. They are accompanied by a decrease in muscle strength and sensitivity in the limbs, loss of visual fields, double contours of objects, speech and swallowing disorders, severe dizziness and vomiting.
A sharp turn of the head or an uncomfortable position can provoke loss of consciousness; such an attack lasts from a few seconds to 5 - 7 minutes; at the end, patients note severe weakness. When you throw your head back, a sudden fall occurs with the disappearance of movements in the limbs, but consciousness does not change.
Watch the video about vertebral artery syndrome and its manifestations:
Abbreviations:
- A1: Horizontal segment of ACA
- A2: Vertical segment of ACA
- ACA: Anterior cerebral artery
- Acom: Anterior communicating artery
- AICA: Anterior inferior cerebellar artery
- AVM: Arteriovenous malformation
- BA: Basilar artery
- CBF: Cerebral blood flow
- CBV: Cerebral blood volume
- CoW: Circle of Willis
- DSA: Digital subtraction angiograph
- ECA: External carotid artery
- ICA: Internal carotid artery
- IoA: Incidence of aneurysms
- M1: Sphenoidal segment of MCA
- MCA: Middle cerebral artery
- MMA: Middle meningeal artery
- MTT: Mean transit time
- PCA: Posterior cerebral artery
- Pcom: Posterior communicating artery
- PDOA: Persistent dorsal ophthalmic artery
- PICA: Posterior inferior cerebellar artery
- PPHA: Persistent primitive hypoglossal artery
- PPOA: Persistent primitive olfactory artery
- PTA: Persistent trigeminal artery
- SCA: Superior cerebellar artery
- sVAD: Spontaneous vertebral artery dissection