What is coronary artery stenting?
More than 2 million stents are implanted annually. And this is understandable, because stents are used to treat one of the most common diseases - coronary heart disease.
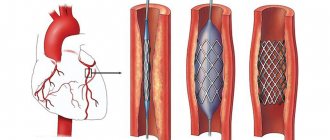
Coronary angioplasty and stenting is an intravascular treatment for coronary heart disease. The basis of coronary heart disease is the narrowing of the blood vessels that supply the heart (coronary arteries) by cholesterol plaques. Stenting allows narrowed arteries to widen. To do this, a special balloon is placed inside the artery and inflated, thus “flattening” the cholesterol plaque and restoring blood flow through the artery. After this, a metal frame—a stent—is implanted into the narrowing site to “fix” the result. In this case, there is no need to open the chest and all manipulations are carried out through a small puncture in the artery in the arm or groin.
Percutaneous transluminal coronary angioplasty (PTCA)
The method of percutaneous transluminal coronary angioplasty (PTCA) was discovered back in the 80s of the 20th century. This technique was developed to remove a narrowed section of a coronary artery to allow adequate blood flow. Typically, this operation is performed in patients with acute myocardial infarction after thrombolytic therapy, or in situations where it is not available. In addition, PTCA is performed in patients with coronary heart disease, when chest pain increases with physical activity, shortness of breath and other manifestations are noted.
Previously, many cardiac surgeons performed coronary artery bypass grafting, but now doctors use an alternative method - PTCA. Before angioplasty, the patient undergoes a full medical examination. At the Isar Heart Center clinic in Germany, a thorough examination is carried out, which includes blood tests, urine tests, coagulation tests, as well as ECG, vascular ultrasound and many other procedures. All medications taken are discussed with the attending physician, as their effects may cause unwanted reactions during surgery.
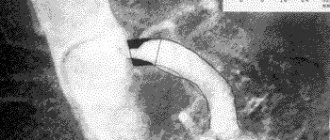
Particular attention is paid to antidiabetic drugs and agents that affect blood clotting. The operation is performed through the femoral artery under local anesthesia. A special needle is inserted into the artery, after which a catheter with a balloon is inserted to the point of narrowing of the vessel. With the help of such a catheter, it is possible to perform coronary angiography during surgery, which allows you to immediately assess the condition of the vessels and adjust the surgical tactics.
After the angiography, the cardiac surgeon will see the narrowing sites and will be able to insert the tip of the catheter behind it. In addition, angiography allows you to evaluate what type of catheter is needed for surgery. During the entire operation, X-ray control is carried out, which allows you to see the location of the catheter. After the catheter is installed behind the narrowing of the vessel, the doctor begins to advance the balloon along it. The balloon inflates at the site of the atherosclerotic plaque, as if crushing it. At the same time, the lumen of the vessel increases, which helps normalize blood flow. This operation can be supplemented with stenting, when after angioplasty a stent is inserted and works as a scaffold in the affected vessel.
With such an intervention, complications are possible in the form of allergic reactions, bleeding, and damage to heart structures. In addition, rhythm disturbances are possible during the procedure. However, the X-ray operating room has all the necessary resuscitation equipment, which is designed to quickly relieve an emergency condition.
Thanks to percutaneous transluminal coronary angioplasty, the symptoms of coronary heart disease are significantly reduced, chest pain becomes less frequent, and patients feel much better. However, in the future, the atherosclerotic plaque may re-grow, and to avoid this, you need to give up bad habits, change your diet and increase physical activity.
The operation must be performed by a highly qualified cardiac surgeon with extensive experience in performing it.
Cost of services
- Name of serviceAdditionalPrice, €
- Percutaneous transluminal coronary angioplasty in Germany – from 4000
cardiac examination price percutaneous transluminal coronary angioplasty PTCA
Who is indicated for cardiac stenting?
Stenting of cardiac vessels is indicated for patients with severe angina pectoris, after myocardial infarction and pre-infarction conditions, patients with proven ischemia (lack of blood to the heart) based on the results of stress tests. In this case, the decision on stenting is made only based on the results of coronary angiography - a contrast study of the heart vessels. Coronary angiography, like stenting, is performed in the cath lab. Often coronary angiography “transitions” into vascular stenting because performed through the same puncture in the artery.
What alternative methods to stenting exist?
- Drug therapy. You need to understand that it is tablets, and not stents, that primarily reduce the risk of myocardial infarction and determine the prognosis in patients with coronary artery disease. Therefore, in many patients with controlled angina pectoris, in the absence of objective evidence of severe myocardial ischemia (lack of blood), coronary stenting can be abandoned, despite significant narrowing in the coronary arteries.
- Coronary bypass surgery. Abdominal surgery, which is often performed using a heart-lung machine. During bypass surgery, bypasses (shunts) are constructed from the patient’s arteries and veins, allowing blood to be supplied to the heart, bypassing areas of the arteries affected by cholesterol plaques.
National Society for the Study of Atherosclerosis
In recent years, the number of cases of sudden death in patients with coronary artery disease has been increasing. Damage to the arteries supplying the heart leads to their stenosis and obstruction; As a result, the blood supply to the heart muscle is disrupted. As a rule, the cause of such narrowing is the presence of atherosclerotic plaque on the artery wall.
These fat deposits lead to a decrease in oxygen supply to the heart. When the blood supply to the myocardium falls below a certain level, drug treatment is required. The photo shows a lesion in the coronary artery.
The main non-surgical way to restore the lumen of the coronary artery is to perform percutaneous transluminal coronary balloon angioplasty. You can judge the essence of this manipulation based on its name:
Percutaneous - means that the catheter is inserted into the vessel through a puncture of the skin.
Transluminar means that all manipulations are carried out through the coronary arteries.
Coronary - means that the coronary artery, that is, the artery that supplies blood to the heart, is affected.
Angioplasty means that the lumen of the vessel is restored (using a balloon).
The term “balloon” means that restoration of the lumen of the affected artery (shown in the figure) occurs by inserting a catheter with a balloon and then inflating it.
The figure demonstrates the restoration of the lumen of the artery by inflating the balloon. In some cases, a stent is then placed into the lumen of the artery to maintain the lumen of the vessel. A special catheter is used to install the stent. The question of performing balloon angioplasty and stenting is decided after receiving the results of coronary angiography - images of the coronary arteries. To do this, contrast is injected into the lumen of the coronary artery using a catheter. The balloon angioplasty procedure can be performed either simultaneously during coronary angiography or after some time (but no more than 6 months, since changes in the angiographic picture may occur during this time). The advantage of one-stage angioplasty is less trauma (the artery is punctured once). The advantage of delayed angioplasty is the ability to more accurately select a stent (type, length, diameter). The choice of procedure in each case is determined by the doctor performing the coronary angiography. Below is step-by-step information about the technique of Transluminal Balloon Coronary Angioplasty (TBCA).
TBCA procedure
Preparation
After a preliminary examination (tests, ECG, ECHO, isotope diagnostics), you need to take a shower, shave the hair in the groin area (if accessed through the femoral artery). You should skip breakfast, or have a light breakfast. You need to have 1.5-2 liters of mineral water without gas and a new video cassette (or a blank CD with the ability to record).
Procedure
The duration of the procedure varies in each specific case, on average 1-2 hours. The patient is taken to the angiography laboratory after preliminary premedication (im administration of sedatives). In the laboratory, the patient is placed on the surgical table and a cubital catheter is installed (in a vein in the arm).
The laboratory is kept sterile, so family and friends cannot be present during the procedure. Electrodes are placed on the arms and legs to continuously monitor the ECG. The puncture site is treated with an antiseptic, then an anesthetic (novocaine, lidocaine, etc.) is injected. The procedure is performed under local anesthesia. During anesthesia, the patient may feel a “tingling sensation of needles.” The necessary medications are administered through a cubital catheter. Remember - you can talk during the procedure, report any changes in your well-being to the doctor. The entire procedure is carried out under X-ray control. A catheter with a balloon at the end is inserted through the puncture site and advanced towards the heart.
When the catheter reaches the site of stenosis, you may feel discomfort in the chest, this is normal. Pain may occur while inflating the balloon. The doctor may ask you to hold your breath for a few seconds.
After the procedure, the patient is transferred to the intensive care unit for dynamic monitoring of ECG, blood counts and puncture site. A small, flexible catheter (introducer) is placed in the artery for several hours, which is then removed by the doctor. A pressure bandage is applied to the puncture site. At this time, you are not allowed to bend your leg. The next day, the patient is transferred to the ward, the bandage is removed and allowed to walk.
You can eat and drink immediately after the procedure. It is recommended to drink 1-1.5 liters of mineral water for better removal of contrast.
The first few days after TBKA, you need to somewhat limit physical activity (load on the lower limbs).
This is what a stent looks like.
Possible complications and risks
If you follow the doctors' recommendations, the risk from the procedure is minimal. In case of complications, full assistance will be provided immediately (including emergency coronary bypass surgery).
- Possible complications:
- Bleeding at the puncture site.
- Heart rhythm disturbances.
- Allergic reaction to contrast.
- Coronary artery thrombosis at the site of ballooning.
- Development of myocardial infarction.
After the procedure
The doctor may change the therapy (for example, cancel nitrates, beta blockers, prescribe drugs that affect blood clotting). Subsequently, we recommend periodic examinations - laboratory tests, ECG, stress test, isotope diagnostics, etc. In some cases, coronary artery restenosis may occur. Therefore, if you feel chest pain, tell your doctor. Remember that the TBKA procedure is the safest method of treating coronary heart disease and is increasingly used.
How to choose between stenting, bypass surgery and drug therapy?
This is the task of your cardiologist, who takes into account the following data:
- The severity of symptoms, namely: the severity of angina pectoris, the severity of shortness of breath, in other words, how much ischemic disease “interferes with the life” of the patient.
- Objective evidence of myocardial ischemia (lack of blood). Most often this is a stress test, ideally stress echocardiography, which should be performed by qualified doctors in a center with a large number of such studies.
- Coronary angiography data. With widespread severe damage to all three coronary arteries, the results of bypass surgery are better.
- Accompanying illnesses. If a patient has diabetes mellitus and multivessel disease of the heart arteries, for example, coronary bypass surgery is usually indicated.
Technique for stenting coronary arteries (with professional jargon)
“We install the introducer”
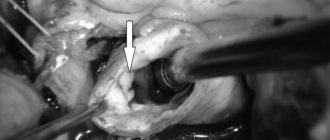
To get to the heart vessels, the doctor needs to get into the patient’s arterial system. For this purpose, one of the peripheral arteries is used - the femoral (in the groin) or the radial (on the forearm). Under local anesthesia, a puncture is made in the artery and an introducer is installed - a special tube, which is the “entry gate” for all the necessary instruments.
"Let's put a guide"
Then a special thin-walled tube about a meter long - a guiding catheter (“guide”) is passed through the patient’s arteries and stops, slightly short of the heart, in the aorta. It is from the aorta that the coronary arteries that supply the heart depart. The tips of the catheters are curved in such a way that it is convenient for the doctor to enter one of the coronary arteries, right or left. By controlling the catheter, the doctor “enters” one of the coronary arteries. Half the job is done.
“Starting a conductor”
But how to get to the point of maximum narrowing in the artery? To do this, we need a “rail” along which all our tools will “ride”. This rail is the coronary guidewire - a thin (0.014 inch = 0.35 mm) metal “lint” with a soft tip (so as not to “scratch” the artery during the operation). Sometimes it is quite difficult to place a guidewire behind the site of narrowing; the tortuosity of the artery, the angle of departure of the branches of the artery, or pronounced narrowing due to the presence of plaques interfere. You can take a “harder” or “slipperier” conductor. Well, or just a favorite, because every doctor has his own preferences. One way or another, the guide ends up behind the site of narrowing on the periphery of the artery that we want to stent.
"Ballooning"
The first instrument that gets to the site of narrowing of the artery is a coronary balloon with a diameter most often from 1 to 3.5 mm and a length of 10-20 mm. The balloon is put on the conductor and moves along it to the point of maximum narrowing where it inflates. The pressure inside the cylinder reaches 15-20 A
Next, along the conductor, to the place that was narrowed before the balloon was inflated, the same balloon is inserted, on the surface of which a stent is fixed in a folded state. The balloon is inflated, the stent is expanded and “pressed” into the artery wall. The stent does not always expand perfectly and then the final stage of the procedure is needed - postdilatation (in simple terms - re-inflation).
"Let's blow it out"
A rigid balloon is placed inside the implanted stent and inflated with high pressure (up to 25 atmospheres). Most often, after this, the stent straightens and adheres well to the walls of the artery.
Transluminal Balloon Angioplasty (TLBA) and Coronary Artery Stenting or Percutaneous Coronary Intervention (PCI) 1. What is Transluminal Balloon Angioplasty (TLBA) of the Coronary Arteries?
2. What is coronary artery stenting? 3. What is a stent? Types of stents. 4. Indications for coronary artery stenting surgery. 5. Contraindications to coronary artery stenting surgery. 6. How to prepare for coronary artery stenting surgery: a. general principles; b. dual antiplatelet therapy. 7. Technique of angioplasty and stenting of coronary arteries. 8. Risks of percutaneous coronary interventions. 9. What is restenosis? 10. Recommendations after coronary artery stenting surgery. Surgical methods for the treatment of coronary artery disease are aimed at directly increasing coronary blood flow - myocardial revascularization. Transluminal balloon angioplasty (TLBAP) is an operation that allows you to restore blood flow in the arteries of the heart (coronary arteries) by inserting a catheter with a balloon and then inflating it. The TLBAP operation was accompanied by a high risk of complications in the form of repeated narrowing of the vessel - restenosis, acute occlusions. In modern endovascular surgery, TLBAP is performed together with endoprosthesis replacement of the coronary arteries, i.e. implantation of stents into the coronary bed.
Positive results from randomized studies have made coronary artery stenting the leading standard in the treatment of patients with coronary artery disease. Since 1999, the term percutaneous coronary intervention “by default” has meant stenting of the coronary arteries. Coronary artery stenting, or percutaneous coronary intervention , is an operation that restores blood flow in the arteries of the heart (coronary arteries) by implanting stents at the site of narrowing of the coronary artery.
Today, coronary stenting occupies a leading place in the endovascular treatment of patients with coronary artery disease. The introduction of this method has significantly improved the results of traditional TLBAP - both immediate and long-term. The main disadvantage of stenting (as well as balloon angioplasty) is the relatively high rate of restenosis. If the use of endoprostheses radically solved the problem of such acute complications of TLBAP as dissections and acute occlusions, minimizing mortality and other ischemic complications (and, accordingly, the need for emergency CABG), and the use of a new regimen of auxiliary pharmacotherapy (aspirin, clopidogrel, IIb/IIIa inhibitors -receptors), on the one hand, practically reduced the incidence of subacute stent thrombosis (and associated ischemic complications) to zero, and on the other hand, it made it possible to implant endoprostheses in acute coronary syndrome, but in terms of long-term results there was no revolutionary shift.
Despite the fact that long-term results after stenting are superior to those of TLBAP (the rate of restenosis in various clinical situations is on average 1.5–2.5 times lower than after balloon dilatation), the most serious drawback of endoprosthetics (as with all endovascular techniques) there remains a relatively high rate of recurrence of angina in the long term and, accordingly, a frequent need for repeated myocardial revascularization. A stent is an intravascular prosthesis to support the wall of the affected vessel and maintain the diameter of its lumen. The design of the stent is a thin mesh frame made of an inert metal alloy of the highest quality, which is expanded by a balloon inside the vessel to the desired diameter.
Types of stents:
Bare Metal Stent The use of metal stents is associated with a risk of thrombosis in the first 30 days and requires dual antiplatelet therapy for 1 month, as well as a 20-30% risk of restenosis (re-narrowing of the vessel) within 6-9 months after implantation.
A drug-eluting stent is an intravascular prosthesis with a coating (polymer) that releases a drug. An
antiproliferative drug-eluting stent is an intravascular prosthesis made of a coated cobalt-chromium alloy that releases a drug that prevents re-narrowing of the vessel.
The medicinal layer subsequently dissolves. First generation of drug-eluting stents: sirolimus- and paclitaxel-eluting stents. Multiple randomized trials have shown that sirolimus- and paclitaxel-eluting stents are associated with reduced rates of repeat revascularization and death from myocardial infarction compared with bare metal stents. The coating of the first generation of stents included polymers that facilitated the release of drug components, but remained on the stent after the drug layer dissolved. These permanent polymers can cause inflammation and delayed endothelialization, requiring long-term dual antiplatelet therapy to prevent high rates of late and very late stent thrombosis.
Recently, the use of drug-eluting stents has shown a clear advantage in the fight against restenosis. In clinical practice, when using bare stents, the rate of restenosis in the long term remained at a relatively high level, and polymer coatings began to be considered as a vehicle for local drug delivery. The purpose of this is the dosed release of the required drug from a stable coating into the local zone of damage to the vascular wall. The drug is released in a uniformly dosed concentration within a certain time interval. The drug delivery system does not lose its properties during sterilization, it also changes its geometric and volumetric shape following the stent during its implantation and is resistant to mechanical damage due to balloon inflation. All of the above properties of the local drug delivery system are achieved using a variety of polymer structures that ensure the integrity of this structure during clinical use.
The drug should have the ability to inhibit the greatest number of different components of the complex restenosis process. The uncontrolled growth of the neointima has some basic characteristics similar to the growth of a tumor, which suggested the use of the cytotoxic drugs Rapamycin (Sirolimus) and Paclitaxel (Taxol). The results exceeded all expectations.
Second generation of drug-eluting stents: zotarolimus- and everolimus-eluting stents. The stents are made of a thinner cobalt-chromium alloy (stent beams - 0.091 mm, compared to first-generation stents, where this figure was 0.132 mm), demonstrate excellent strength and radiocontrast, flexibility, which helps reduce the incidence of restenosis. The drug coating component of more biocompatible polymers is applied to the entire surface of the stent, approximately 95% of the total amount of zotarolimus is released within the first 15 days after stent installation, everolimus - 80% within 30 days, the next 20% within 4 months, which reduces inflammation of the vascular walls. Clinical results compared with first-generation stents showed effectiveness and safety.
Third generation stents - polymer-free biostents based on poly-L lactide or magnesium are created using partially and even completely biosoluble polymers. Bioabsorbable magnesium-polymer stents completely disappear after the required dose of the drug component is released and the treatment of the vessel is completed. The release of medicinal substances and the maintenance of the vessel wall is carried out only as long as the vessel requires treatment. Fully bioabsorbable coated stents reduce the incidence of stent thrombosis compared with non-eluting and drug-eluting stents.
Possible prospects for X-ray endovascular surgery of coronary heart disease are the widespread introduction into clinical practice of new generations of stents with new bioabsorbable polymer coatings. However, their initial use should be preceded by long-term and comprehensive studies examining the immediate, especially long-term, results after their use.
Thus, today there is no alternative to the use of antiproliferative drug-eluting stents in the treatment of patients with coronary artery disease. Widely debated data on possible late complications (late thrombosis) can in no way be a reason to stop their use, but only further emphasize the importance of correctly determining the indications for stenting, careful compliance with all technical aspects of the implantation procedure, and thorough adherence to the regimen of two-component disaggregant therapy in long-term period.
Continuous improvement in the design of stents, leading to the introduction of new technical implantation techniques, such as the use of high pressure, direct stenting techniques (possible by reducing the profile of the stents and attaching it to the balloon catheter of the delivery system); introduction of additional imaging methods such as intracoronary ultrasound (allowing optimization of the final result of endoprosthetics with a high degree of accuracy); careful selection of patients for the procedure (depending on the predicted immediate and long-term results), based on the enormous experience accumulated to date - all this allows us to hope for improved results of both this method itself and the overall results of treatment of patients with coronary artery disease.
Thus, there is a high probability that in the near future both the results of endovascular treatment of patients with coronary heart disease, as well as the concept of choosing a method of myocardial revascularization, and approaches to the treatment of this disease in general will change. The use of stents with antiproliferative drug coating is a highly effective method of treating patients with various clinical forms of coronary artery disease and various morphologically unfavorable variants of coronary lesions. The use of stents with antiproliferative coating, despite the increase in the volume and complexity of the interventions performed, makes it possible to achieve a significant reduction in the frequency of restenosis in the long-term follow-up period, which is the main factor limiting the effectiveness of endovascular treatment.
Back to the topic: “PCI”
Hemostasis
What to do with a hole in an artery?
If the intervention was carried out through the radial artery (on the arm), a special bracelet with a cushion (hemostatic cuff) is put on the wrist, which will put pressure on the injection site and prevent bleeding. Depending on the situation, the cuff will remain on the arm from 3 to 12 hours.
In case of femoral access, there are 2 main options:
- Manual (manual) hemostasis. After the introducer is removed, the doctor presses with his hands on the injection site for 15 minutes. Then apply a pressure bandage for 6-8 hours. The patient should lie on his back with his leg straight.
- Closure devices are special “plugs” that allow you to close the artery from the inside. In this case, there is no need to put pressure on the leg and a pressure bandage is not needed. A special patch is applied to the injection site and several hours of bed rest are recommended.
Stenting is completed.