Causes of coronary artery stenosis
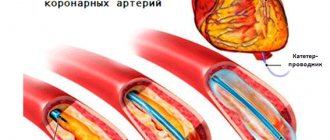
The main cause of stenosis is atherosclerosis, in which cholesterol deposits accumulate on the walls of blood vessels, gradually forming plaques that block the lumen.
Also among the provoking factors include:
- anomalies in the development of coronary vessels (tortuosity, incorrect location);
- cardiomyopathy;
- endarteritis;
- systemic diseases (vasculitis, systemic lupus erythematosus, rheumatoid arthritis);
- benign and malignant tumors;
- heart transplantation.
Increase the risk of vasoconstriction:
- hereditary predisposition;
- hypertension;
- diabetes;
- pathologies of the thyroid gland;
- excess weight;
- sedentary lifestyle;
- smoking;
- frequent stress;
- elderly age.
Stenoses in oncology
Malignant tumors often block the lumen of hollow organs, disrupting their functions. In this case, the patient’s condition always worsens significantly, and the prognosis becomes more serious. If radical surgery for a malignant neoplasm is not possible, then the doctor performs palliative surgery to eliminate stenosis, restore organ function, and improve the patient’s condition.
The patient's condition improves when the tumor begins to disintegrate - it no longer blocks the lumen of the organ. The tumor disintegrates under the influence of chemotherapy, less often on its own. Substances that are released into the blood during massive decay of tumor cells poison the body and can lead to serious complications.
Symptoms of coronary artery stenosis
The main sign of narrowing of the coronary arteries is discomfort, burning and pain in the heart area that occurs during physical and emotional stress. There may be burning pain lasting from 30 seconds to 10 minutes, radiating to the shoulder blade and left arm.
Clinical manifestations may include:
- attacks of dizziness;
- increased heart rate;
- heart rhythm disturbance;
- increased blood pressure;
- shortness of breath;
- weakness.
In some cases, the disease is asymptomatic for a long time and manifests itself only when the vessel is completely blocked by a thrombus or atherosclerotic plaque, which causes ischemia and myocardial infarction. Heart attack is the leading cause of death (90%) from heart disease.
Usually the heart experiences oxygen starvation when the lumen is blocked by 51%. If the artery narrows by 75%, then any physical activity can cause a heart attack, accompanied by necrosis of cardiac tissue. But due to the individual characteristics of the body, some people feel a deterioration in their condition already at 44%, while others do not notice changes even with a narrowing of 75%.
Prevention of cervical stenosis
To prevent the development of the disease, preventive measures should be used:
- kneading the neck - eliminating physical inactivity;
- exercise therapy;
- correct posture, including while working at the computer;
- proper nutrition;
- if necessary, timely contact a specialist.
Feedback from patients suggests that when contacting a medical facility in the early stages, within 6-12 weeks, the pain syndrome disappears in most of them. In advanced cases, as a rule, cervical vertebral artery stenosis requires hospital treatment for a long time.
Diagnosis of coronary artery stenosis
To determine the extent of damage, the doctor sends the patient for a diagnostic examination:
- blood chemistry;
- blood test for cholesterol and glucose levels;
- load tests (treadmill test, bicycle ergometry);
- stress echocardiography;
- electrocardiography;
- 24-hour Holter monitoring;
- ultrasound examination of the heart and blood vessels;
- coronary angiography;
- computer or magnetic resonance imaging of the chest area.
Diagnostic features
The doctor begins with a conversation with the patient, during which he finds out:
- complaints at the time of application;
- factors predisposing to the disease;
- previous diseases.
For the doctor, the body position that the patient is forced to take is important; he palpates the spine in order to determine the affected area.
The patient is prescribed additional examination:
- X-ray of the spine in two projections to determine bone growths, identify destroyed and fused vertebrae, disruption of the structure of joints, the presence of neoplasms, determine their size, location and structure;
- CT scan of the spine to find the cause of the disease, taking into account the smallest changes;
- MRI (if there are no contraindications) to detect changes in cartilage, nerves and blood vessels;
- myelogram to find changes in the structure of the spinal cord, the patency of the canal and the condition of the cerebrospinal fluid.
Treatment of coronary artery stenosis
The doctor selects the method of therapy depending on the degree of development of pathological changes, the cause of stenosis, the presence of concomitant diseases, the age and general health of the patient.
Conservative treatment includes:
- drug therapy (the doctor selects medications individually);
- diet therapy;
- lifestyle changes (giving up bad habits, moderate physical activity).
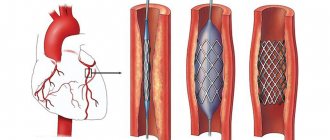
In severe cases, surgery is indicated. Typically, stenting is performed (the vessel is expanded with a balloon and secured with a stent) or bypass surgery (a bypass is created for blood flow).
Primary appointment (examination, consultation) with a cardiovascular surgeon
1850 rub.
Sign up
Why does cervical stenosis occur?
Cervical spinal stenosis develops for several reasons:
- Spinal fracture with compression of the vertebrae (compression);
- Congenital pathological changes in the structure of the vertebrae;
- Inflammatory diseases of the spine;
- Ankylosing spondylitis;
- Tumor processes;
- Intervertebral disc herniation;
- Chronic diseases of the articular surfaces of the spine;
- Adhesions after surgery;
- Overweight;
- Intervertebral disc displacement;
- Bone growths and osteophytes;
- Violation of the structure of the posterior yellow ligament;
- Osteochondrosis.
Stenosis of the neck vessels develops due to a decrease in the cavity where the spinal cord, nerves and vessels of the spine are located. First, complaints arise during certain turns and bends, then blood flow is disrupted and the situation worsens.
Over time, the pressure of the cerebrospinal fluid increases, provoking congestion and inflammatory processes.
One of the most dangerous morphological substrates of coronary heart disease (CHD) is atherosclerotic lesion of the trunk of the left coronary artery (LMCA). Hemodynamically significant lesions of the SLCA occur in 6-11% of cases [3]. However, isolated ostial stenosis of the LMCA, according to the literature [2], is observed in less than 1% of patients and is accompanied by an unfavorable prognosis for life. Mortality with conservative treatment reaches 35% within 4 years and 56% over 6 years of follow-up [7]. Of course, the only possible treatment for this type of coronary lesion is surgery [4]. Currently, there are several methods for myocardial revascularization in case of SLCA stenosis. The main and most common method is coronary artery bypass grafting (CABG). This is the “gold standard” for treatment of this type of lesion. However, along with bypass operations, direct reconstruction techniques are also used for local lesions of the SLCA. Such operations include: endarterectomy and SLCA repair. Similar interventions have been performed around the world for 25 years. If endarterectomy, due to the complexity and uncertainty of the prognosis, has gradually lost its importance, then SLCA plastic surgery with a patch from xeno- or processed autopericardium is used and has very good both immediate and long-term results [1, 5, 6, 8, 9].
Due to the rapid development of interventional cardiology in recent years, methods of endovascular angioplasty of MLCA stenosis are being actively practiced. However, despite constantly improving stents, it is not yet possible to achieve reliable long-term results from such interventions. Recent reports indicate a continued high risk of restenosis and recurrence of angina in the long term. Therefore, at the moment we can say that the search for optimal ways to perform myocardial revascularization for various anatomical variants of SLCA lesions continues.
We present a case of direct LMCA bypass with the right internal mammary artery.
Patient X.
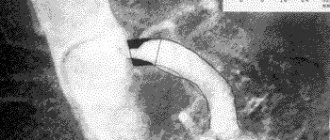
, 55 years old, was admitted to the clinic with complaints of shortness of breath and pressing pain in the chest without irradiation, occurring with little physical activity (walking up to 100 m, climbing to the 1st floor), increased blood pressure to 200/90 mm Hg. , cardiopalmus. Coronary history - 4 years. Examined: electrocardiogram (ECG) - sinus rhythm, heart rate 70 beats/min, signs of left ventricular (LV) hypertrophy; echocardiogram (EchoCG) - LV ejection fraction (EF) 53-55%, local contractility - without clear zones of hypokinesis. Coronary angiography (CAG): right type of blood supply, ostial critical stenosis of the LMCA, stenosis of 30% of the right coronary artery in the middle section, the remaining coronary arteries without hemodynamically significant narrowing (Fig. 1).
Rice.
1. Coronary angiography before surgery. The arrow indicates stenosis of the left coronary artery. Considering the critical lesion of the MLCA, high class of angina pectoris against the background of drug therapy, according to vital indications the patient underwent direct myocardial revascularization. Considering the isolated local (ostium only) lesion and sufficient length, a decision was made to perform bypass surgery directly on the left artery trunk itself.
Technique of operation.
Access: median sternotomy. The right internal mammary artery (IA) in the flap was isolated. Cardiopulmonary bypass (CPB) was started according to the aorta-right atrium scheme. The pulmonary trunk (TP) is bypassed and taken on a holder. The ascending aorta (AA) is clamped. Retrograde pharmacocold cardioplegia with Custodiol solution (1 l). LV drainage was installed through the right superior pulmonary vein. The VA is completely transversely divided at the level of the sinotubular ridge. The aortic wall from the inside is atherosclerotically changed, calcified with the transition of plaques to the mouth of the left artery, which create stenosis (Fig. 2). The lower semicircle of the aortic root is taken on supports and pulled up and brought into the wound, as a result of which the SLCA is completely and widely visualized (Fig. 3). Longitudinal arteriotomy of the SLCA at a distance of 5 mm from the mouth: the artery distal to the incision is practically unchanged, the lumen is passable for a bougie of 3.0 mm. An end-to-side anastomosis was formed with the right internal mammary artery using 8/0 Prolene thread. The integrity of the aorta was restored with a wrapping suture using 4/0 prolene thread (Fig. 4). The clamp is removed from the aorta. The heart rhythm recovered on its own. Standard end of operation. Duration I.K. was 109 minutes, aortic cross-clamping - 65 minutes. The postoperative period proceeded smoothly, angina attacks did not recur. The duration of hospitalization is 6 days. Before discharge, control coronary bypass grafting was performed: the anastomosis of the right internal GA with the SLCA was passable, no hemodynamically significant obstructions to blood flow were identified (Fig. 5). Followed up for 4 years. No angina pectoris. Tolerance to physical activity is high.
Rice. 2. Transverse aortotomy. An atherosclerotic plaque blocking the ostium of the left coronary artery is indicated by an arrow.
Rice. 3. Mobilization of the aortic root. The lower semicircle of the aortic root is taken on a U-shaped support, and the left artery trunk is visualized; LCA—left coronary artery; Ao - aorta.
Rice. 4. Scheme of the operation. 1 - trunk of the left coronary artery; 2 - trunk of the right coronary artery; 3 - right internal mammary artery; 4 - ascending aorta; 5 - pulmonary trunk.
Rice.
5. Coronary bypass grafting on the 4th day after surgery. The arrow marks the anastomosis between the right internal mammary artery and the left artery trunk. To date, there is no uniform surgical tactics for the treatment of patients with ostial lesions of the LMCA. Various surgical techniques have been proposed, each of which has its own advantages and disadvantages, and their long-term results continue to be studied. The safest and most studied in the long-term period is CABG of the LMCA branches. However, when venous material is used as a shunt to the circumflex artery, proliferation of the intima occurs over time, followed by fibrosis and its gradual closure. In addition, there is no physiological perfusion of the myocardium proximal to the anastomoses, since only retrograde blood flow is realized [2-4].
Endovascular techniques are attractive and minimally invasive, but their safety in brainstem lesions continues to be debated. In addition, they have an uncertain long-term prognosis and a high risk of developing restenosis. Moreover, stenting of the SLCA is not always possible due to the anatomical features of the structure or the nature of the lesion. The problem of intervention for an unprotected left artery trunk also remains relevant.
Reconstructive operations on the SLCA are also attractive because they allow the restoration of physiological antegrade blood flow. This approach makes it possible to use endovascular techniques in the future with the progression of atherosclerosis in the distal parts of the left artery, since a fairly wide mouth of the left artery is formed. The disadvantages include the risk of fibrous-sclerotic changes in the plastic material with possible further deformation and stenosis of the artery lumen. The study of long-term results of using patches from the autopericardium, autovenous or autoartery continues [3, 4, 6].
When performing plastic surgery on the SLCA, access to the reconstruction area is of great importance. J. Hitchcock et al. [5] use a transaortic approach, in which the aorta is divided widely transversely at the level of the coronary arteries with the incision continuing at the mouth of the LMCA to the level of the intact wall. The trunk of the pulmonary artery is taken on a holder and moved to the side. J. Villemot et al. [9] propose additionally completely transecting the pulmonary trunk, thus gaining wider access to the SLCA, its bifurcation and the proximal parts of the anterior interventricular and circumflex arteries.
Our proposed method also has its advantages and limitations. The limitation is that it can be used only in the case of isolated local ostial lesion of the LMCA and in the absence of signs of atherosclerosis in the anterior interventricular and circumflex arteries. The advantage of the approach is the use of stay ligatures, which make it possible to significantly expand the aortic root into the wound and thus improve the exposure of the SLCA. Another advantage is the relative ease of performing conventional mammary-coronary anastomosis. Moreover, a conduit made from internal HA is most durable in the long term. Finally, having only one anastomosis, performed most proximally, preserves antegrade physiological blood flow through the coronary vessels. An important point is that the conduit is located under the aorta. This greatly simplifies the surgeon’s actions if any re-intervention is necessary in the future, minimizing the risk of damage to a functioning shunt during resternotomy and cardiolysis. A good clinical and angiographic result indicates the high effectiveness of our technique.
In 2015, the team of authors received patent for invention No. 2551187 for the presented method.
There is no conflict of interest.