First, a small test. Answer FOUR SIMPLE QUESTIONS. Only honestly:
- Are you familiar with pain in the leg muscles, which recently only occurred when walking, but is now present all the time?
- Do you feel unusually tired and weak in your legs after walking just a few steps?
- For some reason your feet have become unusually cold?
- Do you suffer from diabetes and have recently been experiencing burning, tingling and loss of sensation in your feet?
If you answered “Yes” to at least one of the questions, then with a high degree of probability, your health is at risk, and the threat is extremely serious.
These symptoms are an extremely alarming sign of one of the diseases that affects the blood vessels of the legs. The lumen of the arteries narrows, allowing less and less blood to pass through, and in some cases complete blockage occurs. The result is ischemia - that is, insufficient oxygen supply to tissues.
PAINFUL SENSATIONS are just the first signs of an extremely serious threat. Ischemia is an extremely dangerous pathological condition, one of the consequences of which is tissue death, necrosis, gangrene, and, ultimately, amputation.
SAVE YOUR FEET! SEE A DOCTOR IMMEDIATELY!
The cause of ischemia of the lower extremities can be a number of diseases - from atherosclerosis to diabetes. They are united by one quality - large-scale damage to the blood vessels of the lower extremities.
ONLY AN OPERATION TO RESTORATION OF VASCULAR FUNCTIONS CAN OVERCOME THE DISEASE!
Attempting to use advertised “miracle ointments” or folk remedies can lead to wasted time and serious complications. Therapeutic methods are aimed at combating symptoms, but cannot restore vascular function.
Modern medical technologies offer two methods that can radically solve the problem of damaged blood vessels:
BALLON ANGIOPlasty and vascular stenting
Both methods are the result of the development of innovative vascular surgery. Operations are performed inside vessels using ultra-modern micro-instruments and under constant visual X-ray control.
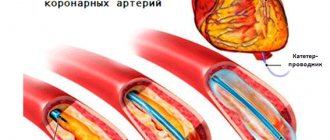
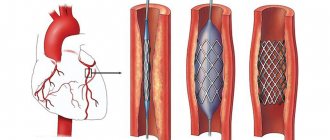
Balloon angioplasty is the insertion of a special balloon into a vessel that has narrowed as a result of the disease. When folded, the balloon is delivered through the vessel through a puncture to the site of narrowing. There, the balloon is inflated with air and expands the vessel from the inside, normalizing the size of the lumen. After this, the balloon is deflated and removed from the vessel. Often, after balloon angioplasty, the vessel is strengthened with a stent - a mesh endoprosthesis.
Vascular stenting. In some cases (for example, with “diabetic foot”), stenting is an operation that is the only way to avoid amputation. In essence, this is prosthetics of damaged sections of the artery. A stent is inserted into the vessel, which is a mesh cylinder that serves as a rigid frame. The stent fixes the walls of the vessel and establishes the necessary lumen, as a result of which the blood flow is completely normalized.
GET YOUR HEALTH BACK TODAY! TOMORROW WILL BE LATE!
Balloon angioplasty and stenting are not a panacea, but a chance to regain lost health.
Remember that the further the disease has progressed, the more difficult it is to achieve a complete recovery!
CONTACT A SPECIALIST IMMEDIATELY!
Features of angioplasty
Angioplasty is one of the methods of endovascular treatment. The advantage of angioplasty is that it is less traumatic for the patient and does not require general anesthesia or a long hospital stay. Angioplasty is considered a minimally invasive type of intervention on a vessel, since reconstruction is carried out from the inside. Angioplasty is usually combined with a stenting procedure. During stenting, a stent is implanted into the vessel, which subsequently keeps the vascular walls from narrowing.
Anesthesia for stenting
Most endovascular angioplasty procedures and lower extremity vascular stenting can be performed with mild intravenous sedation and local anesthesia at the access puncture site. Monitoring of blood pressure, electrocardiogram and blood oxygen saturation level (pulse oximetry) is mandatory. In case of unforeseen complications, the operating room is equipped with a breathing apparatus and a defibrillator. If the operation is performed for critical ischemia, then to make the patient comfortable, epidural anesthesia is performed (injection of an anesthetic drug through a catheter into the spinal area).
Application
The angioplasty technique is considered one of the most effective ways to restore vascular lumen. It is used in the treatment of ischemic disease, diseases of the peripheral arteries and vessels responsible for the blood supply to the brain. Angioplasty is performed in cases where the vessels of the circulatory system are narrowed and do not provide the organs and tissues with the necessary amount of blood. This intervention is prescribed when drug treatment of occlusion or stenosis does not produce an effect and the disease threatens life-threatening complications.
Rehabilitation period
After discharge from the clinic, it is recommended to avoid physical activity for several days. If a follow-up examination and consultation with a cardiologist does not show anything alarming, the patient will soon resume his usual lifestyle.
The result after coronary artery angioplasty depends on how carefully the patient follows the instructions of the attending physician:
- For 6-12 months after angioplasty, regular use of blood thinning medications is necessary.
- Lifestyle correction is no less important: quitting smoking, weight control, special diet.
- At the appointed time, the patient will have to come to see a cardiologist and undergo a preventive examination.
Kinds
- Transluminal balloon angioplasty. During the intervention, a special catheter with a balloon at the end is inserted through the artery of the thigh or arm, which is delivered to the affected area of the vessel under X-ray control. In the area of narrowing, the balloon is inflated, and it expands the vascular lumen.
- Excimer laser angioplasty. This method involves using an excimer laser device that removes atherosclerotic tissue, destroying it.
Depending on the location of the vessels, the following are distinguished:
- Cardiac angioplasty or coronary angioplasty. This is an effective method of treating coronary heart disease and angina. It is classified as percutaneous coronary intervention (PCI). Coronary angioplasty helps prevent myocardial infarction or stop its development in the early stages.
- Angioplasty of vessels of the extremities. Used to treat vascular diseases of the legs. Angioplasty is recommended in the treatment of diabetic foot, obliterating atherosclerosis of the lower extremities, obliterating endarteritis and other ailments that are accompanied by ischemia of the extremities.
- Angioplasty of the renal arteries. It is used in the treatment of diseases associated with damage to the vessels of the kidneys: renovascular arterial hypertension, renal artery stenosis, etc.
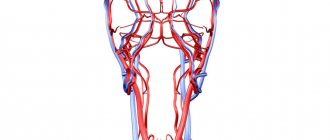
- Angioplasty of vessels involved in the blood supply to the brain and head tissues. If the carotid or vertebral arteries are affected, there is a high risk of stroke. Angioplasty is one of the types of operations on the vessels of the neck, which is used along with open interventions. Angioplasty eliminates carotid artery stenosis without traditional open surgery.
Endovascular technologies at the Innovative Vascular Center
The main mission of our clinic is the treatment of critical ischemia and gangrene of the extremities. We are committed to using the latest approaches to solve this problem. Since 2011, endovascular surgery methods for critical ischemia have been introduced into the practice of our vascular surgeons. Noting the advantages of the endovascular approach, every year we expand the capabilities of our clinic in the use of these methods.
The role of minimally invasive technologies is growing - now more than 50% of patients with critical ischemia and gangrene are operated on endovascularly, and even more than 40% use a hybrid approach. This is bypass surgery with angioplasty and stenting of the arteries of the lower extremities. The Innovative Vascular Center is a clinic where more than 500 angioplasty and stenting operations of lower extremity arteries are performed per year.
The capabilities of endovascular surgery are developing synchronously with the creation of innovative treatment tools, so in our practice, puncture operations are increasingly replacing open interventions.
How to prepare?
Angioplasty is performed routinely or urgently. In the latter case, the decision is made individually, for example, when a patient is admitted to a hospital with acute coronary syndrome, which indicates the development of myocardial infarction or unstable angina. If the doctor conducting the examination sees the need for this, the intervention is carried out simultaneously with angiography.
Angioplasty is performed in a specially equipped operating room, where X-ray equipment and recording equipment are installed. The patient prepares for planned angioplasty in advance - he will learn how to do this at an appointment with a cardiologist. On the eve of the intervention, the patient is asked to undergo additional examination, follow a diet, and take certain medications.
Preparing for stenting
Before performing stenting surgery, the patient must be properly examined for vascular lesions and risks of complications. A set of laboratory tests and a coagulogram must be performed before surgery. Considering the patient's load on antithrombotic drugs, it is necessary to exclude possible sources of bleeding (stomach ulcer, bleeding hemorrhoids).
On the eve of the intervention, a light sedative is administered, allowing the patient to sleep well and not be nervous. Before the operation, the patient will shave the site of the intended access. In the preoperative room, the nurse will place a urinary catheter and an intravenous needle for infusions. In the operating room, a pressure cuff is placed on the shoulder and sensors for continuous ECG recording are fixed on the chest.
Literature
- DORMANDY JA, MAHIR MS. The natural history of peripheral atheromatous disease of legs. In: Greenhalgh RM, Jamieson CW, Nicolaides AN, (ed.), Vascular surgery. Issues in current practice. London, Grune & Stratton, 1986 pp 3-17.
- MARTY-ANE C, ALAUZEN M, MARY H. L'expectative medicale dans les lesions obstructives isolees de l'art e re femorale superficielle. In: B ranche reau A, Jausseran JM, (eds), Traitement des lesions obstructives de l'artere femorale superficielle. Marseille, CVN, 1992 pp. 13-17.
- JOFFRE F, ROUSSEAU H, MEITES G, CHEMALI R. Resultats a long terme des angioplasties femoro-poplitees. In: Branchereau A, Jausseran JM, (eds), Traitement des lesions obtructives de l'artere femorale superficielle.Marseille, CVN, 1992 pp 39-51.
- JOHNSTON KW. Femoral and popliteal arteries: reanalysis of results of balloon angioplasty. Radiology 1992; 183: 767-771.
- HUNINK MGM, DONALDSON MC, MEYEROVITZ MF et al. Risks and benefits of femoropopliteal percutaneous balloon angioplasty. J Vasc Surg 1993; 17: 183-194.
- BECQUEMIN JP, CAVILLON A, HAIDUC F. Surgical transluminal femoropopliteal angioplasty: multivariate analysis outcome. J Vasc Surg 1994; 19: 495-502.
- MATSI PJ, MANNINEN HI. Impact of different patency criteria on long-term results of femoropopliteal angioplasty: analysis of 106 consecutive patients with claudication. J Vasc Interv Radiol 1995; 6: 159-163.
- STANLEY B, TEAGUE B, RAPTIS S et al. Efficacy of balloon angioplasty of the superficial femoral artery and popliteal artery in the relief of leg ischemia. J Vasc Surg 1996; 23: 679-685.
- COURBIER R. Le traitement des lesions de l'artere femorale superficielle. In: Branchereau A, Jausseran JM, (eds), Traitement des lesions obtructives de l'artere femorale superficielle. Marseille, CVN, 1992 pp XIII-XIV.
- DIETHRICH EB, PAPAZOGLOU K. Endoluminal grafting for aneurysmal and occlusive disease in the superficial femoral artery: early experience. J Endovasc Surg 1995; 2: 225-239.
- BERGERON P, PINOT JJ, POYEN V et al. Long-term results with the Palmaz stent in the superficial femoral artery. J Endovasc Surg 1995; 2: 161-167.
- AHN SS, RUTHERFORD RB, BECKER GJ et al. Reporting standards for lower extremity arterial endovascular procedures. J Vasc Surg 1993; 17: 1103 -1107.
- BRAY AE, LIU WG, LEWIS WA et al. Strecker stents in the femoral arteries: value of Duplex ultrasonography in restenosis assessment. J Endovasc Surg 1995; 2: 150-160.
- BECKER GJ, KATZEN BT, DAKE MD. Noncoronary angioplasty. Radiology 1989; 170: 921-940.
- MATSI PJ, MANNINEN HI, VANNINEN RL et al. Femoropopliteal angioplasty in patients with claudication: primary and secondary patency in 140 limbs with 1-3 year follow-up. Radiology 1994; 191: 727733.
- Guidelines for percutaneous transluminal angioplasty. Standards of Practice Committee of the Society for Cardiovascular and Interventional Radiology. Radiology 1990; 177: 619-626.
- MURRAY RR Jr, HEWES RC, WHITE RI Jr et al. Long-segment femoropopliteal stenoses: is angioplasty a boom or a bust ? Radiology 1987; 162: 473-476.
- CURRIE IC, WAKELEY CJ, COLE SE et al. Femoropopliteal angioplasty for severe limb ischemia. Br J Surg 1994; 81: 191-193.
- SIVANANTHAN UM, BROWNE TF, THORLEY PJ, REES MR Percutaneous transluminal angioplasty of the tibial arteries. Br J Surg 1994; 81: 1282-1285.
- BLAIR JM, GEWERTS BL, MOOSA Hetal. Percutaneous transluminal angioplasty versus surgery for limb-threatening ischemia. J Vasc Surg 1989; 9: 698-703.
- SEEGER JM. Laser angioplasty. A vascular surgeon's view. Circulation 1991; 83 (I): 97-98.
- SATIANI B, DAS BM, VACCARO PS, GAWRON D. Angiographic follow-up after laser-assisted balloon angioplasty. J Vasc Surg 1993; 17: 960-966.
- FISHER CM, FLETCHER JP, MAY Jetal. No additional benefit from laser in balloon angioplasty of the superficial femoral arter y. Eur J Vasc Endovasc Surg 1996; 11: 349-352.
- DALSING MC, HARRIS VF. Intravascular Stent. In: White RA, Fogarty TJ, (eds), Peripheral endovascular interventions. St Louis, Mosby, 1996 pp 315-339.
- HENRY M, AMOR M, HENRY I et al. Placement of Palmaz stent in femoropopliteal art eries: a six year experience. Factors influencing restenosis and longterm results. In: Abstract Book 6° International course on peripheral vascular intervention. Oct 1995, Nancy, France.
- WHITE GH, LIEW SCC, WAUGH RC et al. Early outcome and intermediate follow-up of vascular stents in the femoral and popliteal arteries without long-term anticoagulation. J Vasc Surg 1995; 21: 270-281.
- DO-DAI-DO, TRILLER J, WALPOTH BH et al. A comparison study of self-expandable stents vs balloon angioplasty alone in femoropopliteal artery occlusions. Cardiovasc Intervent Radiol 1992; 15: 306-312.
- HENRY M, AMOR M, HENRY I et al. Endoluminal bypass grafting in leg arteries with the Cragg Endopro System 1. A series of 105 patients. In Abstract book 6° International course on peripheral vascular intervention. Oct 1995, Nancy, France.
- G. Agrifiglio et al.1999
A few words about stents
When performing coronary angioplasty, the following are used:
- Simple metal (without drug coating) stents;
- Drug-eluting stents are stents coated with a special polymer on the stent wall in contact with the vessel and releasing a dosed drug that prevents the development of restenosis;
- Bioabsorbable (self-absorbable) stents - when installed, they expand the lumen of the artery, and within three months they release a drug that prevents the process of restenosis. And after two years, bioabsorbable stents dissolve.
Each type of stent is selected individually, according to indications, taking into account the wishes of the patient and in accordance with all the features of the course of the disease.