The best specialists in the industry work in cardiology at the IMMA medical center. An individual approach to each patient ensures a reliable collection of the clinical picture of a dangerous heart disease – myocarditis. In their work, cardiologists are guided by evidence-based medical practice, the principles of evidence-based medicine and the recommendations of the WHO of the Russian Federation. Which together gives high efficiency and a positive prognosis of therapy. The use of modern equipment for diagnostic measures makes it possible to accurately determine the presence or absence of myocarditis.
In our clinics you can:
- Get a consultation with a cardiologist;
- Take an ECG and get a professional interpretation of the results;
- Complete the ABPM procedure;
- Undergo Holter monitoring;
- Take advantage of other services of our clinics.
For more details and any questions, please contact the number listed on the website
Myocarditis - basic definition
Inflammation of the heart muscle that is not associated with impaired blood circulation in the coronary arteries is called myocarditis. The disease affects the middle layer of muscle tissue - the myocardium. The causative agents are specific infections and viral pathologies. In some cases, inflammation can be triggered by allergic, autoimmune diseases and acute intoxication. According to the World Health Organization, myocarditis is diagnosed in 10% of cases of all heart diseases.
The main danger of the pathology is the absence of an age threshold. Myocarditis can develop in both children and the elderly. Although the prognosis for most cases is positive, the disease is highly unpredictable. Without timely diagnosis and treatment, a sudden disturbance in heart rhythm may occur - arrhythmia, which causes extremely serious consequences, including death.
How often does it occur?
The statistics of myocarditis are based on data on the dead - 3-9%, it is discovered almost by accident, when a person dies from an unknown cause and seems to be in complete health. In cardiology departments, its share is barely 1% of all patients. In infectious diseases hospitals, where, logically, myocarditis should be much more common than anywhere else, it is hidden from statistical accounting in the group of numerous complications of an infectious disease.
European studies give a wide range of incidence from 0.12 to 12%, but in 8.6% of people who suddenly died, myocarditis is found, despite the fact that no one suspected the disease during their lifetime. Acute myocarditis is undoubtedly a disease of the young: among all causes of sudden death before the age of 40, its share is 12%; in no other age cohort there is such an incidence. As a rule, the sudden death of a child is also on the “conscience” of myocarditis, as is the death of conscripts and athletes. Men get sick more often because estrogen protects women from heart disease.
Types of myocarditis depending on the causes
The classification of the disease according to the ICD is based on the cause-and-effect factor that causes myocarditis. Depending on the provocateurs, the disease takes the following forms:
- Infectious myocarditis
Infectious diseases of various origins, in severe manifestations, cause complications on the myocardium - inflammation develops. The cause may be all kinds of herpes, influenza, and hepatitis viruses. Bacterial diseases. Fungal pathologies of Candida and Aspergillus. Parasitic organisms. Diphtheria bacillus, chlamydia, streptococcus.
- Rheumatic myocarditis
It is a derivative of infectious myocarditis. Develops against the background of a depressed immune system. The main reason is hemolytic streptococcus, which causes pathologies on the mucous membranes.
- Allergic myocarditis
The disease develops against the background of an allergic reaction. In this case, the factors can be very different. Burns that provoke the release of large amounts of toxic substances into the blood. Organ transplantation, transplantation leading to implant rejection and myocardial damage. Allergy to drugs, as a result of which the drugs cause inflammation of the heart muscle.
- Toxic myocarditis
Alcohol poisoning, kidney failure, which results in increased uric acid levels, and heavy metal vapors can cause inflammatory processes in the myocardium.
- Symptomatic myocarditis
The consequence of chronic diseases can be myocarditis. As a rule, these are autoimmune diseases - lupus erythematosus, rheumatoid arthritis, scleroderma, which have an extremely negative effect on all internal organs, including the heart.
- Idiopathic myocarditis
A disease with unknown etiology. It is characterized by partial damage to the myocardium and a severe form of the course. Most often it becomes the cause of death. This is due to the current impossibility of establishing the causes of development.
Based on the classification of the disease, most existing infections can cause an inflammatory process in the heart muscle. Therefore, even a seemingly banal cold can give impetus to the inflammatory process in the myocardium. A preventive examination after a viral illness is the best way to prevent myocarditis.
Important! A timely detected and fully treated infection minimizes the risk of complications affecting the heart muscle.
Myocarditis code according to ICD-10
I01.2 - Acute rheumatic myocarditis
I40 - Infectious myocarditis
I40.1 - Isolated myocarditis
I41.0 - Myocarditis in bacterial diseases classified elsewhere
I41.1 - Myocarditis in viral diseases classified elsewhere
I41.2 - Myocarditis in other infectious and parasitic diseases classified elsewhere
I41.8 - Myocarditis in other diseases classified elsewhere
I51.4 - Myocarditis, unspecified
Symptoms
The signs of myocarditis are extensive and completely depend on the form, course and degree of development of the pathology. The development of the disease is divided into several groups:
- According to the form of the course: acute, chronic and rapid.
- By localization: focal and diffuse.
- By severity: light, medium and severe.
With any type of myocarditis, patients have several similar symptoms: chronic fatigue, general weakness, pain in the chest and under the left shoulder blade, increased sweating, shortness of breath.
An expanded group of signs indicates the presence of a certain type of myocarditis:
• Minor symptoms are characteristic of infectious-allergic myocarditis. The patient experiences slight weakness, perceived more as a consequence of fatigue than as a symptom of a dangerous disease. Taking vitamins and aspirin, a person does not even think about the fact that dangerous inflammatory processes are occurring in the body.
• Idiopathic or rheumatic myocarditis is manifested by acute, burning pain in the heart and left arm. The clinical picture is similar to ischemic heart disease - lethargy, limited motor function, constant lack of air, and in some cases, night fever.
• Diffuse localization of the inflammatory process affecting the entire myocardium is characterized by acute heart failure and its characteristic symptoms. Swelling appears, bruises under the eyes, limbs go numb and acquire a bluish tint.
• Bacterial myocarditis is characterized by disruption of the circulatory system. There is a high risk of blood clots forming in the main arteries of the heart. It manifests itself as a change in the color of the skin, shortness of breath, even during rest, and constant aching pain behind the sternum.
The severity of the pathology is completely reflected in the appearance of the patient. At the initial stages of the inflammatory process, no visible changes are observed. The patient may complain to the attending physician about general weakness. As the disease worsens, the patient's lips become blue, the limbs become pale, and swelling occurs under the eyes. In the severe form, swollen veins in the neck and arms, a painful dry cough, and shortness of breath are clearly visible, interfering with the usual activities.
Important! If any of these signs appear, you should immediately seek medical help. It is especially important to do this after suffering from infectious diseases.
Rehabilitation
An important part of recovery is reducing the load on the heart by regulating physical activity. You should not overdo physical activity immediately after recovery. Sometimes it is better to limit physical activity, including walking, for several months. You should consult your doctor about your activity regimen and when you can return to normal activities.
It is also important to visit your doctor regularly after recovery. Usually, before the visit you need to perform an echocardiogram, an electrocardiogram, and a general blood test.
If myocarditis is prolonged or there is severe heart failure, it is important to adhere to a diet with limited salt, liquid, alcohol and smoking.
Treatment
The main attention in the conservative treatment of myocarditis is paid to etiotropic therapy - elimination of causes and complications. In the first stages, hospitalization occurs, a strict diet is prescribed, bad habits are eliminated, and inflammation is relieved.
The standard scheme of therapeutic measures is as follows:
- Strict bed rest in a hospital for at least four weeks;
- Limiting physical activity;
- Supportive complex therapy;
- Taking a wide group of anti-inflammatory drugs – NSAIDs;
- Antibiotic treatment for specific viral pathologies;
- Prescription of hormonal drugs - glucocorticosteroids (GCS). It is used in severe cases to suppress the hormone cortisone, which is responsible for the development of inflammatory processes;
- Immunomodulation. Maintaining and restoring the body’s protective function;
- Correction of metabolic processes. To enrich the heart muscle with oxygen and nutrients;
- Preventive vitamin course.
Compliance with basic treatment standards is the key to successful treatment. Therefore, self-medication of heart pain is strictly contraindicated. This can lead to irreparable complications, the mildest of which will be myocardial infarction. The patient is only required to be attentive to his own health - to listen to the first alarm bells of the body and undergo a timely examination. Only a cardiologist can make the correct diagnosis and prescribe treatment after a complete history collection.
IDENTIFICATION OF EXTENSIVE MUSCLE-MYOCARDIUM INFLAMMATION
Recognition of diffuse inflammation (myocarditis) begins with dissociating this pathology from myocardial dystrophy. Both diseases are similar in clinical description, but can be easily distinguished on an electrocardiogram.
In addition to the ECG, ultrasound examination is required for diffuse myocarditis. This is the basis for diagnosing myocarditis.
An ultrasound will show not only the presence of pathology, but also:
- stage of development of the inflammatory diffuse process;
- changes in muscle tissue caused by myocarditis;
- progressive or incipient complications;
- area of muscle damage (in diffuse myocarditis it is extensive).
Usually, ultrasound, ECG (sometimes with echocardiography) and chest x-ray are sufficient to identify diffuse inflammation. The latter is needed to view the condition of each area damaged by myocarditis.
Among other manipulations - a standard set:
- cardiological examination ( diffuse myocarditis indicates postopnea , cyanosis, swelling of the legs, rapid pulse);
- CBC + LBC, urine examination (for signs of inflammation to verify infectious diffuse myocarditis). If a bacterial attack is suspected, a microbiological test may be prescribed.
Complications
The consequences of advanced myocarditis are negative processes in the heart muscle. Depending on the course and form of the disease, irreversible changes may appear in the myocardium, which lead to disruption of the normal functionality of the heart muscle - blood pumping. In extreme cases, the lesions are so severe that they lead to cardiac arrest and sudden death.
Long-term myocarditis leads to abnormal enlargement of the heart muscle. The process is irreversible, so in such cases the patient is advised to undergo long-term therapy and a complete overhaul of their lifestyle.
The most severe consequences are considered to be giant cell myocarditis. Most patients with this diagnosis require heart transplantation. Otherwise, cardiologists give an unfavorable prognosis for life. According to WHO, approximately 90% of patients die within 4-5 years if a heart transplant is not performed.
The inflammatory process in the myocardium contributes to scarring of muscle tissue, which in turn completely disrupts the heart rhythm and blood supply. This leads to the development of heart failure and, as a rule, ends with ischemic heart disease.
But in most cases, normal heart function is restored, although it requires long-term preventive treatment and lifelong monitoring by a cardiologist.
Diagnostics
The examination begins with questioning the patient and assessing his condition. The doctor examines the color of the skin, determines the presence of edema, listens to heart sounds, assesses the frequency and rhythm of the pulse, and measures the temperature. Then an instrumental examination is performed:
- Electrocardiography (ECG). Allows you to determine arrhythmias and identify disturbances in myocardial contractility. A diagnosis cannot be made on the basis of an ECG alone, since there are no changes characteristic only of myocarditis.
- Chest X-ray. The image can determine the size and shape of the heart, and reveal the accumulation of fluid in the pleural sinuses, which will indicate heart failure.
- Magnetic resonance imaging (MRI). It records the size of the heart, its shape and structure, and changes in muscle motor activity.
- Echocardiography. Allows you to create moving images of a beating heart. During echocardiography, you can determine the thickness of the myocardium, detect expansion of the heart chambers, decreased pumping function, fluid in the pericardial sac, and find out whether there are problems with the valves.
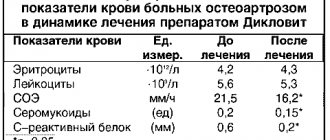
- General blood analysis. Based on the results of a general blood test, you can evaluate the ESR and the level of leukocytes - “inflammatory cells”.
- Biochemical analysis will help determine the levels of enzymes that indicate muscle damage - creatine phosphokinase, troponin. In addition, antibodies to bacterial agents can be detected in the blood, and viruses can be detected using PCR.
- Heart biopsy. This is the most accurate diagnostic method, but due to its complexity it is rarely used.
- MiniRNA profiling. This new method makes it possible to differentiate the fulminant form of myocarditis from the acute form.
Who is at risk
The most common cause of myocarditis is viral pathologies of various origins. Therefore, the risk group includes every person who has had herpes, hepatitis B, C, rubella, chicken pox, measles, diphtheria and even influenza. Since most people have been diagnosed with some kind of viral disease, everyone must undergo a preventive examination in order to exclude the presence of inflammatory processes in the heart. This can subsequently save lives.
The risk of developing myocarditis increases in proportion to the presence of infectious pathologies. Listening to your heart is recommended for everyone who has suffered or is a carrier of diseases caused by the following pathogens:
- Bacteria that provoke the development of tuberculosis, chlamydia, staphylococcus.
- Fungal genus Aspergillus fumigatus and Candida. They cause such common diseases as tonsillitis, laryngitis, otitis media, conjunctivitis, candidiasis, etc.
- Parasitic worms - roundworms, echinococci, trichinella, lamblia, toxocariasis.
- Diabetes mellitus in any degree.
- Thyroid diseases.
- Autoimmune pathologies – rheumatoid arthritis, lupus erythematosus, vasculitis.
The risk group includes people whose professional activities involve working in enterprises with hazardous working conditions, where there is a possibility of heavy metal poisoning. Taking certain medications can cause inflammation of the myocardium. For example, antiallergic cephalosporins or antidepressants have an extremely negative effect on cardiac activity. Social factors play an important role for the myocardium. Abuse of alcoholic beverages, smoking and other dangerous and harmful addictions contribute to the development of myocarditis.
Relevance of the problem
The problem of admission to pregnancy and management of women with heart and vascular lesions is becoming increasingly urgent. The desire to move higher on the social ladder, to acquire a financial “safety cushion”, and a later age of marriage have led to an increase in the age of first-time women. Motherhood in adulthood is more often associated with the risk of endocrine and cardiovascular diseases (or CVD).
Also, the high level of development of medicine has become the reason that more and more women with congenital heart defects survive to reproductive age and are allowed to become pregnant, while the increased load on the body becomes the main cause of maternal mortality. Among all CVDs, the greatest risk of adverse outcome of pregnancy and childbirth is borne by:
- congenital heart defects;
- rheumatic heart valve lesions;
- conditions with increased blood pressure.
Cardiomyopathies are extremely rare, but pose the greatest danger to women.
Timely detection of CVD allows for preventive monitoring, hospitalization and timely treatment.
Consultation and examination with a cardiologist
IMMA medical clinics have modern equipment and their own laboratories to accurately determine myocarditis in the initial stages. The full range of studies includes an initial examination by a qualified cardiologist, clarifying tests, and diagnostic measures using modern technologies. Diagnosis and treatment of myocarditis in children and adults takes place in equipped clinics, trained by experienced personnel, under the guidance of leading cardiologists.
To make an appointment, use the contacts listed on the website. The professional staff of the clinic will provide all possible information support.