Briefly about the treatment method
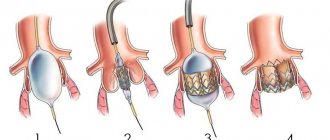
Endovascular treatment of abdominal aortic aneurysm (EVAR) is a minimally invasive alternative to major open surgery for abdominal aortic aneurysm, which reduces the risk of surgery, speeds up recovery time and increases survival rate for this dangerous disease. Endovascular surgery involves only small incisions in the thigh through which an artificial vessel called a stent graft is installed inside the aneurysm. A stent graft is a metal mesh of a special design (stent), which is covered from the inside with a sealed polymer fabric (graft). A metal mesh fixes this device to the walls of the aorta and iliac arteries, and polymer fabric isolates the lumen of the artificial vessel from the aneurysm cavity. Thus, the aneurysmal sac is isolated from the blood flow, and the risk of continued growth and rupture of the aneurysm after installation of the stent graft is significantly reduced. The operation is performed without the use of general anesthesia and is not accompanied by significant blood loss. Installation of a stent graft for an aortic aneurysm is much safer than classical open surgery.
Causes of development of abdominal aortic aneurysm
- atherosclerosis, in which the appearance of cholesterol plaques on the wall of the aorta gradually reduces its strength, which contributes to protrusion in one of the areas;
- congenital predisposition, transmitted through the male line, confirmed by many years of observations: the presence of an aneurysm in the father indicates a 50% chance of this disease occurring in his son;
- an inflammatory process of a chronic, sluggish nature that occurs in the aortic wall itself or in the adipose tissue that surrounds the vessel;
- traumatic damage to the wall due to trauma or injury to the abdomen, surgery or endovascular intervention.
Atherosclerotic manifestations become the cause in 85-90% of cases of the development of acquired aneurysm in the abdominal aorta. Signs of predisposition to the development of the disease are smoking, arterial hypertension and chronic pulmonary diseases.
Advantages of treatment at the ISC
The innovative vascular center always strives to introduce the most advanced technologies of vascular surgery into its practice. Considering that endoprosthetics is a safer alternative to open surgery for aneurysms, since 2015 we have practically replaced aneurysm resection operations with this intervention. In our practice, we use the best stent grafts from Western manufacturers, which are selected individually for each patient. Our specialists successfully perform endoprosthesis replacement operations for the most complex forms of abdominal aortic aneurysms.
Indications and contraindications for the treatment method
Indications
- The standard endoprosthetic procedure is suitable for an aneurysm that begins 2-3 centimeters below the orifices of the renal arteries, that is, it has a neck for reliable fastening of the endoprosthesis, preventing blood leakage around the endoprosthesis - “endoleak”.
- Surgery is indicated when the aneurysm reaches a sufficiently large diameter (usually more than 5 cm) that the risk of complications (rupture or thrombosis) exceeds the risk of surgery.
- Installation of a stent graft into an aortic aneurysm is also carried out when the aneurysm is growing rapidly (diameter according to ultrasound increases by more than 0.5 cm per year)
- For embolism (transfer of blood clots from the aneurysmal sac to the arteries in the legs).
- Aortic aneurysms that cause abdominal pain, which may indicate an impending rupture.
When selecting patients for aortic replacement, we proceed from an assessment of the risk of open surgery. Studies that compare EVAR with open surgery have demonstrated fewer early complications with the endovascular approach and lower overall mortality rates. Endovascular treatment requires more careful monitoring and sometimes additional interventions when various leaks are detected. If surgery is planned in young patients in good general health, open surgery is preferable. In elderly patients, endovascular surgery is the method of choice, since the mortality rate after open surgery exceeds 10%. As the technology for manufacturing stent grafts develops, indications for open surgery are becoming less and less common.
Placement of a stent graft for a ruptured abdominal aortic aneurysm provides a significantly better chance of survival compared to emergency open surgery, as well as helping patients with thoracic and abdominal aortic dissection survive if performed in a timely manner.
Contraindications
Anatomically unsuitable structure of the aortic aneurysm for endoprosthetics. Most often this is the absence or a very short section of the normal abdominal aorta below the renal arteries (absence of an aneurysm “neck”). In this case, it is not possible to secure the upper section of the stent graft well to avoid leakage. However, stent grafts with side branches for the renal arteries have now been proposed for use, which allow the stent graft to be placed higher, restoring flow into the renal arteries.
Relative contraindications are small diameter or aneurysms of the iliac arteries, severe calcification and occlusion of the femoral arteries, however, modern stent grafts and the possibilities of hybrid (open and endovascular joint) surgery make it possible to solve these problems.
Open surgery for aortic aneurysm
The operation is performed under general anesthesia. The essence of the operation is to remove the aneurysmal expansion and replace it with a synthetic prosthesis. In most cases, the consequences of the operation are favorable. The average rate of serious complications and death with open procedures ranges from 2 to 5%. However, it may be higher if the renal and/or iliac arteries are involved in the aneurysm, as well as due to the patient’s concomitant pathology.
Postoperative observation in the hospital usually ranges from 10 to 14 days. Rehabilitation in the early postoperative period takes about 1-2 months.
More information can be found on the open surgery page.
Preparing for treatment
To determine the indication for endovascular treatment of an aortic aneurysm, patients must be properly evaluated.
- General clinical blood and urine tests
- Biochemical blood test (urea and creatinine)
- Blood tests for infections (hepatitis, HIV, syphilis)
- Ultrasound of the abdominal cavity and aorta
- Ultrasound of the carotid arteries
- ECHO cardiography
- Examination of the stomach (gastroscopy) to prevent bleeding from an ulcer.
- Multislice computed tomography (MSCT) of the aorta and arteries of the lower extremities. This study should show the thoracic and abdominal aorta with branches and arteries of the lower extremities. Based on MSCT, the operation is planned and the size and type of stent graft is selected.
Diagnostics
Very often patients do not make any complaints. But if symptoms appear, they are nonspecific. The most common symptoms include pain in the abdomen, back, or chest area. Patients describe this pain in different ways: some feel moderate to severe pain or tenderness in the middle or upper abdomen or lower back, while others feel the aneurysm itself as a beating and pulsating mass in the abdominal cavity. But, as noted, many may not experience any symptoms. Sometimes abdominal aortic aneurysm
may be detected during a routine physical examination. When palpating the abdomen, the doctor may detect a bulge or pulsation in the abdominal cavity. But most often, an aneurysm is detected during medical tests such as an abdominal ultrasound (ultrasound) or computed tomography (CT) scan. The size and location of the abdominal aortic aneurysm, as well as the general condition of the patient, help to choose the right treatment method. If the aneurysm is small, your doctor may recommend surveillance (regular examinations to monitor its size). A large aneurysm or a rapidly enlarging aneurysm has a high chance of rupture and requires treatment.
Pain relief during treatment
To access the aorta, the femoral arteries are usually used, which are exposed openly through small incisions. For pain relief, epidural anesthesia is used (the insertion of a catheter into the spine through which an anesthetic solution is supplied). Full patient monitoring is mandatory. Respiratory equipment for artificial ventilation of the lungs is at the ready. For intravenous infusions, a subclavian venous catheter is used.
How the treatment method works
The operation is performed under sterile conditions, under the control of an X-ray angiographic unit, by a joint team consisting of a vascular and endovascular surgeon.
The patient's femoral arteries are accessed by a vascular surgeon using 4-5 centimeter incisions. The femoral arteries are isolated and placed on supports that allow them to be manipulated.
A diagnostic catheter is passed through the brachial or radial artery in the arm into the abdominal aorta for angiographic evaluation of the aneurysm and the condition and origin of the renal arteries. This is very important, since it is impossible to close the renal arteries with a stent graft, as renal failure will develop.
The endoprosthesis reliably closes the aneurysm cavity from the inside, conducting blood without contact with the aneurysmal sac, which over time leads to thrombosis of the aneurysm and a decrease in its size.
After opening the femoral arteries, special tubes (intraducers) are installed in them, through which special conductors are passed into the aorta above the aneurysm. The main body of the stent graft is then passed through a guidewire through a small incision in the right femoral artery. This is the main prosthesis placed in the aorta and the right leg, which should be located in the right iliac artery. Next, the main body of the endoprosthesis is carefully positioned in the area of the “neck” of the aneurysm, so that when opening in the area of the renal arteries, only the special crown of the endoprosthesis is placed, but not the closed section of the stent-graft. Monitoring is carried out using a diagnostic catheter placed above the aneurysm.
After opening the main branch and the right leg, a guide is inserted into the hole intended for the second branch and taken out beyond the stent graft. The left leg of the stent graft is passed along this guidewire for placement in the left iliac artery. After opening this leg, the structure is assembled.
To ensure a tight fit of the stentgraft to the walls of the aorta, it is additionally straightened with special balloons. After this, control angiography is performed, which should show uniform filling of the endoprosthesis, no leakage of contrast in addition to the prosthesis, and normal patency of the arteries below the prostheses.
The stent graft delivery devices are then removed from the arteries. The holes in them are sutured with a vascular suture. Control drainage is inserted into the wound. Blood flow in the lower extremities and kidneys is monitored using angiography from the upper catheter.
Possible complications during treatment
Complications of the intervention can be divided into those that relate to the course of the operation itself or to the design and location of the endoprosthesis. Thus, myocardial infarction that occurs immediately after the intervention is a complication of the operation, not the prosthesis. On the contrary, the development of leaks along the stent graft is a complication associated with the endoprosthesis.
The longevity of the results of endovascular treatment of aortic aneurysm depends on careful monitoring of the condition of the prosthetic section of the aorta and taking action when complications are identified.
One of the main reasons for complications with EVAR is that the contact between the proximal neck of the aneurysm and the stent graft is loose, due to the complex anatomy of the neck and the discrepancy between the diameter of the stent graft and the size of the neck. Most often, this is due to the anatomical features of the neck and one can expect that with the advent of special fenestrated or branched stent grafts, this complication will become a thing of the past. Currently, the use of such stent grafts is possible, but their installation is more complex, and the devices themselves are much more expensive than standard ones. If the contact is not tight, the aneurysm does not turn off completely and can continue to grow and even rupture. Therefore, leaks (endoleaks) must be eliminated immediately after they appear.
Complications associated with surgery
- Aortic dissection
- Contrast-related renal failure
- Thromboembolism is the transfer of blood clots through the bloodstream into the underlying arteries of the legs.
- Acute obstruction of the intestinal arteries - mesenteric thrombosis
- Bleeding in the access area in the groin area
- Access area infection
- Myocardial infarction, heart rhythm disturbances, respiratory failure.
Complications associated with stent graft
- Migration of the endoprosthesis
- Aneurysm rupture
- Stent graft thrombosis
- Leaks (endoleaks) into the aneurysm cavity
There are 5 types of leaks:
Type I - Leakage in the upper and lower places of stent graft attachment (in the area of the renal and iliac arteries). The latter lies almost freely in the aorta and aneurysm without performing its protective function for the aneurysm. Type II - Retrograde blood flow into the cavity of the aneurysmal sac from branches of the aorta such as the lumbar and inferior mesenteric artery. This type of leak occurs most often and carries the least risk. Immediate treatment is not required, since the cavity may become thrombosed and the endoleak will disappear spontaneously. Type III - leakage between overlapping parts of the stent (for example, between the main body of the stent graft and the left leg) or rupture of the endoprosthesis covering. Type IV - leakage through the stent graft wall due to the porosity of the coating material. With the development of technology for manufacturing stent grafts, this type of endoleaks is disappearing. Type V—expansion of the aneurysmal sac without detectable leakage. Spontaneous growth of an aneurysm, the causes of which are not clear.
Systematization of manifestations of aortic aneurysm
Currently, there is no unified approach to systematizing the manifestations of peritoneal aortic aneurysm. Most often, doctors and authors of medical works use the method of A. Pokrovsky and R. Ermolyuk, according to which aneurysms are divided:
- by etiology
– acquired (non-inflammatory or inflammatory) and congenital; - according to morphology
- into false (traumatic origin), true and stratifying; - by shape
- diffusion and saccular; - according to the course of the clinical process
- into diseases with an uncomplicated course, complicated and dissecting; - by type and location
- on the proximal segment of the peritoneal aorta, on the infrarenal section, as well as with total damage to the entire section of the abdominal aorta.
According to medical statistics, up to 95% of aneurysms are localized in the infrarenal region.
Prognosis after treatment method
If the endoprosthetics operation is performed correctly and with a good immediate result, then the risk of aneurysm rupture is reduced many times and a year after this procedure is compared with the results of an open aneurysm resection operation. The patient can be discharged home 2-3 days after surgery. Taking into account the low postoperative mortality after endovascular treatment, the risk of endoprosthetics is significantly less than the risk of open surgery. Therefore, in Western countries, more than 80% of patients with abdominal aortic aneurysm are operated on using the endovascular method. However, for a lasting positive result, the patient must be under dynamic observation.
A giant aneurysm of the abdominal aorta was successfully operated at the National Medical Research Center of Surgery named after. A.V. Vishnevsky
The normal diameter of the aorta is 2 cm, and its expansion (aneurysm) of up to 5 cm or more is considered a reason to sound the alarm. The larger the diameter of the aneurysm, the thinner the walls of the aorta and the higher the risk of rupture. Giant aneurysms are quite rare and require immediate surgical treatment.
Patient, diagnosis
Patient, 57 years old. Diagnosis: giant aneurysm of the abdominal aorta (11 cm), coronary heart disease, involvement of the obtuse margin branch 80%, stenosis of the right coronary artery 60%, long-term persistent form of atrial fibrillation, type II diabetes mellitus.
The essence of the intervention
Resection of an abdominal aortic aneurysm was performed with aortobiiliac prosthesis; an Ecoflon prosthesis was used, the main branch with a diameter of 22 mm.
Risks and features of the situation
The risk of a giant aneurysm rupturing reaches 80% (if this happens, it is almost impossible to save the person). The presence of such a diagnosis is the basis for immediate surgical intervention.
Among other things, the patient had a narrowing of the blood vessels of the heart, which could lead to a heart attack during the operation or in the near future after it.
How events developed
The patient was admitted to the Department of Cardiac Surgery of the National Medical Research Center named after. A.V. Vishnevsky regarding coronary heart disease. An abdominal aortic aneurysm was discovered during the examination, after which the patient was transferred to the vascular surgery department.
Having a giant aneurysm, a person usually feels throbbing and pain in the abdomen (including back pain), but may not pay much attention to them until the doctor asks him a question on this topic. However, this condition is another argument in favor of urgent surgery, since we are talking about a symptomatic aneurysm, and there are signs of its impending rupture.
How the decision was made
A number of meetings and consultations were held in which the heart team participated - vascular surgeons, cardiac surgeons, X-ray endovascular surgeons, anesthesiologists, cardiologists.
It was important to decide on the sequence of actions: what to do first—to operate on the aneurysm or to carry out cardiac measures (myocardial revascularization)? Severe heart disease in a patient could provoke a heart attack even without surgery - out of the blue or under any load. At the same time, cardiac treatment involves taking antiplatelet agents, which dramatically increase the likelihood of bleeding during surgery.
A decision was made, which everyone considered the most balanced: first, resection of the aneurysm would be done. As a result, the operation was performed, and 2 weeks after it, stenting of a branch of the obtuse edge of the circumflex artery was performed. 3 days after stenting, the patient was discharged in good condition.
Why was open surgery chosen rather than endoprosthetics?
Surgical treatment of an aneurysm involves its removal and installation of a prosthesis during open surgery or a low-traumatic intervention (endoprosthetics). However, in order to achieve the desired result with the help of an endoprosthesis inserted inside the expansion, certain anatomical conditions are required. More precisely, a certain location of the aneurysm in relation to the surrounding vessels. This patient was not able to undergo standard endoprosthetics, since there was a risk of blocking the vessels supplying the kidneys.
There are non-standard, more complex options for low-traumatic operations, but they also did not seem justified. One of the reasons was that to protect the kidneys, endoprostheses would also be needed here: the result would be a kind of “sandwich” (parallel graft technique), which would not guarantee exclusion of the aneurysm from the blood circulation, so the goal would not be achieved. In addition, the more non-standard the intervention, the higher the risk of complications in the long term.
Taking into account the totality of all factors, a decision was made to perform an open operation.
Subtleties of anesthesiology
Vascular anesthesiology is considered one of the most difficult. And in this case, it is simply impossible to overestimate the role of anesthesiologists. Damage to the vessels of the heart and the gigantic size of the aneurysm, the specifics of the operation (the aorta is clamped and, as a result, the load on the heart increases sharply), preparing the patient for such an intervention and preventing any disturbances in cardiac activity is a highly qualified work, practically an art.
Surgeon's comment
Alexander Feliksovich Kharazov, Department of Vascular Surgery (head of the department - Academician of the Russian Academy of Sciences, Professor A.V. Pokrovsky):
“Our patient had severe heart disease, and he could have had a heart attack even without surgery - out of the blue, as they say, or with minimal stress. But it was impossible not to operate on it, since aneurysms of this size rupture in 60-80% of cases within a year. All this speaks to the skill of the doctors who performed anesthesia and did not allow severe and fatal cardiac complications to develop.
Technically, resection of a giant aneurysm is quite complicated: the larger this “bag” of blood, the greater the blood loss, the longer the blood circulation is blocked during the operation and the greater the load on the heart. Of course, this together creates a lot of dangers. In this sense, it is very important that the intervention was planned and not emergency. Using a three-dimensional model created by a CT scanner, we were able to analyze the situation in advance. When you have a picture of what you will see later during surgery in front of your eyes, it allows you to play out in your head all possible deviations from the norm. If you've done this, you're ready. And if you rush into it without a plan, then there may be nuances...
It is known that 70-80 percent of such operations in developed countries are performed using low-traumatic techniques. Does this mean that our Western colleagues would choose exactly this method? Is not a fact. A lot depends on where the patient ends up. Some surgeons practice only endoprosthetics, and stubbornly. Others, like us, make decisions depending on the situation. Let’s say, if in the USA a patient went to Professor Hazim Safi’s clinic in Houston, he would undergo the same operation as ours, because they have extensive experience in this kind of intervention. And the more experience, the better the results.
The uniqueness of our case lies in the correctly chosen balanced approach. We weighed the pros and cons of a low-traumatic intervention and analyzed the patient’s ability to undergo major surgery. We realized that our facilities, equipment, experience of our anesthesiologists, surgeons and the operating team as a whole would allow us to carry out exactly the surgical treatment that was planned. We literally walked on the edge of a knife, but emerged victorious.
Composition of the operating team
- Cameraman: A.F. Kharazov
- Assistants: V.A. Kulbak, V.N. Gontarenko, N.M. Basirova
- Anesthesiologist: A.F. Kozhanova
- Operating nurse: E.S. Zenina
Observation program after treatment method
The next day after the operation, an examination by a vascular surgeon is carried out, wounds in the groin areas are bandaged, and drains are removed. To assess the effectiveness of the operation, an ultrasound of the abdominal aorta and arteries of the lower extremities is performed.
Every 3 months after surgery, it is necessary to perform MSCT of the aorta to identify possible leaks. Such studies are carried out during the first year. Then they need to be repeated annually. If MSCT is unavailable, ultrasound of the abdominal aorta may be performed.
If leaks are detected, the patient is hospitalized in the clinic for correction, since once these complications arise, they do not go away on their own, but require intervention to correct and prevent aneurysm rupture.