Life after valve replacement
The lifespan after surgery directly depends on the individual characteristics of the patient’s body and on whether the patient complies with the necessary rules or not.
Having a valve replacement procedure not only improves a person's overall well-being, but also minimizes the likelihood of death due to heart failure. Only 0.2% of people die after surgery, so the prognosis can confidently be called favorable. Patients need to avoid stress and psycho-emotional stress in every possible way.
Diet after surgery
Many patients forget about general recommendations as soon as the rehabilitation period passes.
In fact, a certain diet must be followed throughout your life. It means:
- caffeine withdrawal;
- giving up alcohol and nicotine;
- refusal of unhealthy foods (fried, fatty, floury);
- inclusion of fruits, vegetables, herbs in the diet;
- consumption of cereals, lean meat and fish.
After surgery you need to give up coffee
Such nutrition increases the patient’s life expectancy, since it partially eliminates the risk of blood clots. People with a biological prosthesis are also not recommended to indulge in junk food, alcoholic drinks and cigarettes.
Gymnastics
For the first year after surgery, the person will need to see the doctor monthly. It is the specialist who, if necessary, can prescribe a course of therapeutic exercises. You should not resort to performing any strenuous exercises. As an alternative, you can do the simplest exercises, or better yet, do therapeutic walking.
In the second postoperative year, you will need to visit a specialist every 6 months, and all subsequent times – once every 12 months.
The patient is prohibited from engaging in heavy work or participating in various sports competitions. The patient needs to spend at least 1-2 hours in the air every day.
- Life against the tide. Mitral valve prolapse and what is behind it
The patient needs to spend 1-2 hours in the fresh air every day
After open surgery, a scar or a noticeable scar remains on the chest, which plastic surgery (in particular, laser correction) can help remove. Such procedures must be agreed upon with the attending physician.
Valve replacement is a procedure that significantly increases the patient's chances of living a normal life. It can restore a person’s efficiency, cheerfulness and activity.
Symptoms
Often, heart valve defects do not appear clinically for a long time, and complaints depend on the severity of the disease. When the disease manifests itself, patients experience shortness of breath, dizziness and fainting during exertion, a feeling of heaviness, chest pain, heart rhythm disturbances (arrhythmias), swelling, fatigue, and decreased performance. Often the heart’s ability to compensate for defects lasts for a long time. Therefore, patients seek help at a time when it is already difficult to help them due to the “neglect” of the disease, when the heart has exhausted its compensation capabilities and has turned, figuratively speaking, into an “overinflated balloon.”
Who needs such an operation
In a situation where the valve ceases to fulfill its purpose, a disruption occurs in the direction of blood flow. As a result, the heart muscle begins to wear out extremely quickly and gradually leads to heart failure. This, in turn, does not allow the blood to circulate well and provide the human body with the necessary amount of oxygen and nutrition. These problems will eventually lead to irreversible processes throughout the body and even to the death of the patient. The only way out of this situation can be heart surgery.
Important! The main reasons why a doctor recommends surgical intervention is a severe organic pathology that can develop into a heart defect.
- Birth defects, which today are most often diagnosed in childhood.
- Adhesions or seals between valve petals. Quite often, such patients undergo a surgical operation known as commissurotomy, but sometimes, due to individual characteristics, this manipulation cannot be performed. It is in this case that the valve is replaced.
- Wrinkling of valve leaflets or tendon strands. This may be a consequence of rheumatic carditis, which usually develops due to a streptococcal infection in the body.
- Myocardial fibrosis is a disease in which the valves become covered with connective tissue. This pathology usually develops as a consequence of complications of certain inflammatory heart diseases.
- Calcification. Calcium salts accumulate on the valves. Most often this happens as a consequence of metabolic disorders or hormonal imbalances. Quite often this is a hereditary pathology. In addition, cardiac rheumatism also has such consequences.
- Aortic stenosis, which developed as a complication after previous coronary artery bypass grafting.
Etiology:
- Inflammatory lesions: rheumatism, systemic scleroderma, aortoarteritis.
- Degenerative processes: myxomatous degeneration.
- Atherosclerosis.
- Infectious processes: infective endocarditis.
- Congenital pathology: bicuspid aortic valve.
There is a tendency to increase the frequency of involutional (degenerative-atherosclerotic) causes of aortic stenosis, which has led to an increase in age patients over 60-65 years of age requiring surgical correction of aortic disease.
With congenital or rheumatic valve damage, a long latent period without clinical manifestations is observed. Mortality and the risk of complications increase significantly with the onset of symptoms of the disease. With angina pectoris, fainting and manifestations of heart failure caused by systolic dysfunction of the left ventricle, the average life expectancy is 5, 3 and 2 years, respectively. In asymptomatic patients, the risk of sudden death is low (even with severe aortic stenosis), while in the presence of symptoms, 15–20% of patients die suddenly.
Types of heart valve replacement surgeries
The operation is performed on an open heart with the patient connected to the artificial circulation system. Currently, innovative minimally invasive techniques have been introduced in advanced clinics such as the Almazov Center, where heart valve replacement is carried out under local anesthesia without dissecting the chest.
Read more about the types of prostheses
The prosthesis is selected individually, depending on the diagnosis, the patient’s condition, and the presence of comorbid pathology. The shape of the implant depends on which heart valve is affected. Prostheses are made either from artificial materials (mechanical) or from tissues of animal origin (biological). The patient is often interested in which option is better to choose. Let's try to figure it out.
Characteristic features of mechanical products:
- Made from plastic, carbon, metals.
- They are highly durable and have a 15-20 year warranty.
- Recommended for young patients.
- Increase the risk of blood clots.
- In the postoperative period, lifelong use of anticoagulants is required.
Biological prostheses can be described as follows:
- Pain in the late period of rehabilitation after knee replacement
- They are xenografts and allografts.
- Relatively short-lived, requiring replacement after 8-12 years.
- It is advisable to implant in people of older age groups, with a risk of blood clots, and allergies to anticoagulants.
- There is no need to prescribe antithrombotic drugs.
Among cardiac surgeons, the popularity of the Ross operation is increasing - replacing the aortic valve with a pulmonary valve (autograft), and the pulmonary valve with a prosthesis made of biomaterials.
Patient preparation
During hospitalization, the clinic’s doctors will ask the patient to take with him all the extracts, examination data, ask about existing diseases, taking medications, and then prescribe additional tests on the eve of the operation.
Preparing for heart valve replacement has two goals:
- Identification of possible risks during and after prosthetics.
- Planning the course of surgical intervention and rehabilitation procedures.
The effectiveness of treatment depends on this. It is important to inform specialists even of minor points, in the patient’s opinion.
The doctor needs to know the following:
- heart valve condition;
- degree of severity of disorders in the myocardium;
- changes in heart function;
- the patient has a tendency to bleed;
- danger of respiratory and allergic complications;
- features of the liver, endocrine and excretory systems;
- history of bad habits;
- taking medications and biological supplements.
It is usually recommended to undergo a laboratory examination (general clinical tests and biochemistry), instrumental diagnostics (x-ray, ultrasound, functional methods), and obtain consultations with specialized specialists (including an anesthesiologist, even if a minimally invasive intervention without general anesthesia is planned). On the eve of prosthetics, the patient will be asked not to smoke, eat or drink.
Technique of the operation
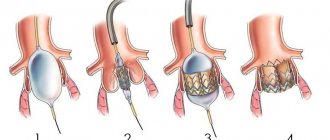
The technique for performing prosthetics is almost the same when replacing different valves. The order of the stages of the operation is strictly observed. Access to the heart is carried out by dissecting the sternum or ribs along the lateral lines.
A longitudinal incision is made to open the pericardium. The artificial blood circulation machine is connected. Procedures are carried out to cool the heart and prevent air embolism. Temporary electrodes are sutured to the myocardium, and drainage is left in the pericardial cavity and mediastinum.
Progress of the procedure
The person is given general anesthesia. The cardiac surgeon removes the affected valves, installs artificial ones in their place, then connects the myocardium, starts the organ’s work, and sutures the covering tissue.
- Mechanism of development, diagnosis and treatment of aortic calcification
A self-expanding artificial biovalve is passed by a catheter through an artery or vein (depending on which valve needs “repair”) to the required part of the heart, melts under the influence of body temperature, and is put into operation immediately after transportation.
It is also possible to replace the valve using a mini-access - an incision up to two and a half centimeters in the fifth intercostal space to the left of the sternum. An artificial valve is inserted to the apex of the heart.
It is important to know! A huge advantage of such techniques is not only the absence of the need to open the heart cavity, but also the ability not to resort to connecting a heart-lung machine.
Suspected complications
When replacing a heart valve, adverse consequences can occur both during the procedure and in the postoperative period. The attending physician will definitely inform the patient about possible complications. In the operating room, the patient’s condition is completely controlled by a team of doctors.
During rehabilitation, a person should immediately seek help in the following situations:
- the color of urine or feces has changed;
- shortness of breath appeared;
- have problems with hearing or vision;
- numbness of the limbs is felt;
- inexplicable fatigue sets in;
- there is swelling and hyperemia of the sutures;
- an increase in body temperature is recorded.
A negative consequence may be associated with the proliferation of fibrinous tissue, bleeding due to taking anticoagulants, the formation of blood clots, hemolysis of red blood cells, and the addition of an infection. Careful preoperative preparation and adherence to medical recommendations will help avoid dangerous conditions.
Rehabilitation
On average, the duration of hospitalization in the clinic takes 7–10 days, including the first days after prosthetics in the intensive care unit. But even a successful result requires a recovery period of up to 3-6 months.
A few simple tips that will make your rehabilitation easier:
- take all medications prescribed by your doctor;
- eat easily digestible carbohydrates;
- regularly check your sugar and cholesterol levels;
- give up baths and saunas for at least a year;
- perform measured physical activity.
Sometimes, even with very good health indicators, depression awaits a person in the postoperative period. Therefore, it is important that the person recovering is under the supervision of an experienced specialist and has psychological support.
Hospitalization at the Bakulev Center in the emergency surgery department for acquired heart defects
At the time of hospitalization in the NCPPS department, the patient was 68 years old.
In the hospital during examination
The condition is of moderate severity. Height 150 cm, weight 75 kg. BSA = 1.78. BMI = 33.33.
The body structure is incorrect. The development of subcutaneous tissue is moderately increased. There is no swelling. The color of the skin is acrocyanosis. The chest is of the correct shape. Respiratory rate 20/min. Breathing is harsh, carried out in all departments. No wheezing. Heart sounds are muffled and arrhythmic. Systolic murmur in the second intercostal space on the right, carried out to the vessels of the neck. Heart rate = 100 beats/min. Blood pressure: on the left arm - 120/60 mm. rt. Art. Satisfactory filling pulse = 100 beats/min.
The liver is not enlarged. The stomach is soft. Physiological functions are normal.
Instrumental studies
EchoCG:
| LP | 48 mm | LV: | CSR | 49 | KDO | 104 | EF 53% |
| MK: | not changed | FC 34mm | Regur. 1 tbsp. | TK: | Regur. 2 tbsp. | ||
| AK: | FC 20mm. Double-leaf. Calcification of the valves. Systolic opening is reduced. Peak gradient on the valve is 110 mmHg. Regurgitation of the 1st degree. | ||||||
| Aorta: | Ascending: 37 mm | ||||||
LA - left atrium, LV - left ventricle, ESV - end-systolic volume, EDV - end-diastolic volume, EF - ejection fraction, AK - aortic valve, FC - annulus fibrosus, MK - mitral valve, TC - tricuspid valve.
Angiocardiography:
Cardiac ischemia. Right type of blood supply to the myocardium. Anomalous origin of the right coronary artery from the left coronary sinus. Stenosis of the anterior interventricular branch in the middle third is 50%.
ECG:
atrial fibrillation with heart rate 70-90 beats/min.
Based on the results of examinations in the hospital, a decision was made to perform radical correction of the defect under conditions of artificial circulation and hypothermia.
On the seventh day of hospitalization, an operation was performed - replacement of the aortic valve with a biological prosthesis Carpentier-Edwards Perimount No. 21 supraannularly with ligation of the left atrial appendage, under conditions of bypass, hypothermia and PCCP.
About the purpose of disability and prognosis
Non-working group II is determined for a period of one year after completion of the operation to restore the myocardium. In the future, transfer to group 3 is possible.
When establishing disability, cognitive deviations (decreased mental abilities) are taken into account individually.
How long do you live with an artificial valve? The average life expectancy in this case is approximately 20 years. However, theoretically, the valve’s lifespan is much longer (up to 300 years, according to doctors).
Indications for prosthetics
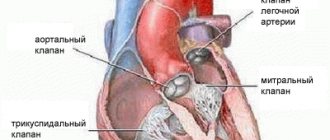
For normal blood flow, coordinated operation of the valve apparatus is necessary. The mitral, aortic, tricuspid and pulmonary valves provide blood flow from the chambers of the heart to the aorta and pulmonary trunk, playing a major role in hemodynamics. When their valves are destroyed, narrowed or incompletely closed, blood enters the vessels in insufficient quantities, which leads to progressive heart failure. The only way to improve the patient's condition is to surgically eliminate the defect and install a mechanical or biological implant. Heart valve replacement and replacement are indicated when:
- congenital or acquired cardiac pathology, heart disease;
- post-infarction pathology, aneurysm;
- prolapse, stenosis or insufficiency;
- atherosclerotic lesions;
- diseases of rheumatic etiology;
- valve atresia;
- infective endocarditis and septic lesions;
- fibrous scars or adhesions on the valves;
- calcification and compaction.
Clinical signs indicating the need for surgery:
- decreased tolerance to physical activity;
- the occurrence of shortness of breath, the inability to sleep in a horizontal position, the appearance of moist rales in the lower parts of the lungs (due to increased pressure in the pulmonary circulation);
- visualization of blood clots in the cavities of the heart on ultrasound;
- expansion of the heart cavities on echocardiography (left atrium more than 40 mm);
- the occurrence of arrhythmias (extrasystole, blockade).
After aortic valve replacement surgery
Once the operation is completed, the patient is sent to the intensive care unit. Here he is brought out of anesthesia and vital functions are monitored:
- The heart rate is determined.
- Breathing and blood pressure are monitored.
- The oxygen level in the blood is checked.
- A tube is inserted into the mouth and lungs to provide additional ventilation.
- A drain is installed to drain fluid from the chest.
- The patient has a catheter placed in the bladder to drain urine.
- Pain medications, fluids, and electrolytes are injected directly into a vein.
After aortic valve replacement, the patient usually spends 5-7 days in the hospital if there are no complications.
Telemedicine consultation at the Bakulev Center
Based on the results of a consultation at the telemedicine department of the Bakulev National Center for Cardiovascular Surgery, the patient was recommended for surgical treatment under artificial circulation - aortic valve replacement.
Polyclinic NCSS
Two weeks after the telemedicine consultation, an examination was carried out in the clinic of the National Center for Cardiovascular Surgery, based on the results of which the diagnosis was clarified:
“Calcified aortic valve disease is a critical stenosis. Relative mitral insufficiency. Relative tricuspid insufficiency. Pulmonary hypertension. Permanent form of atrial fibrillation. Atherosclerosis of the coronary arteries. NK 2A. FC 3".
A decision was made to hospitalize him.
Rehabilitation and possible complications
After successful prosthetics, the patient remains in intensive care for two days. This is necessary to restore strength after anesthesia, anesthesia and sedation. The length of stay in intensive care is two to three days, followed by three to four weeks in the hospital. During this time, the wound on the sternum heals and the body adapts to hemodynamics after prosthetics. Throughout the entire period, the doctor regularly measures blood pressure and evaluates the condition of the heart and suture using ultrasound.
After a minimally invasive replacement, recovery takes no more than seven to ten days. Considering the small size of the wound, healing occurs faster, with less severe pain.
Rehabilitation in the postoperative period includes:
- Limit physical activity in the first week.
- Gradual increase in motor activity during the first two weeks.
- Prescribing drug therapy to prevent thrombosis, blockage of the valve by a blood clot.
- Individual selection of exercise regimen after hemodynamic restoration.
- Special diet and monitoring of the condition.
The most common concerns after prosthetics are:
- general weakness;
- sometimes dizziness;
- headache;
- aching pain in the suture area;
- periodic heart pain;
- swelling of the legs;
- sleep disturbance.
As a rule, such complications are not permanent and disappear within four to five weeks after surgery.
If the condition worsens, contact a cardiologist or surgeon. Early screening prevents the surgical consequences of heart valve replacement and improves the patient's life.