Is leukopenia cancer?
Leukopenia is not cancer.
This is a separate condition characterized by a decrease in the level of white blood cells in the blood. It is also diagnosed in healthy people. Often this clinical picture is observed in patients who have recently had ARVI or influenza. The stages of physiological changes are also considered to be a serious pathology: in children 6 months, 5-6 years. Leukopenia is benign when it is caused by “lazy leukocyte syndrome.” Of particular danger is the situation when a decrease in leukocytes is accompanied by the appearance of bruises throughout the body, an increase in body temperature, rapid fatigue, and numerous skin rashes. In this case, you need to undergo a comprehensive diagnosis and consult a doctor.
Leukopenia is one of the symptoms of blood cancer. This is a dangerous disease, the main insidiousness of which is the absence of a tumor that needs to be removed. That is why leukopenia requires a mandatory diagnostic examination, because oncology detected in the initial stages is highly treatable.
Recommendations for patients with leukopenia after chemotherapy
The key secret in the successful fight against any disease is the coordinated work of the patient and the oncologist. Their joint efforts will make it possible to successfully fight the disease. To do this, it is important to know and follow the recommendations of your doctor. The correct diet deserves special attention - it is determined individually for the patient, in order to stimulate the production of leukocytes. Also, the Vitamed clinic will establish recommendations on lifestyle, taking into account possible symptoms of the problem and other procedures that have proven their effectiveness in practice.
Causes of leukopenia
Many factors can provoke the development of leukopenia. It is very important to determine the exact cause of this disorder, because treatment tactics will depend on it. The following factors can cause a decrease in leukocytes in a person’s blood:
- Pathologies of blood cells and bone marrow
: aplastic anemia, myelofibrosis, myelodysplastic syndromes, hypersplenism, myeloproliferative syndrome; - Hereditary diseases
: myelocathexis, Kostman's syndrome; - Infections
: tuberculosis, HIV, AIDS, various viral infections; - Autoimmune pathologies
: systemic lupus erythematosus, polyneuritis, rheumatoid arthritis; - Vitamin deficiency
: lack of B vitamins, copper, zinc, and other minerals. Usually occurs due to an unbalanced diet; - Taking certain medications
: Interferon, Clozapine, Minocycline, Cyclosporine, some antibacterial agents; - Sarcoidosis
: a disease in which there is an overreaction of the immune system; - Oncology
: Cancer causes a decrease in the concentration of white blood cells due to damage to the bone marrow. A similar clinical sign is also observed in patients after radiation or chemotherapy, or bone marrow transplantation.
Reasons for a decrease in the level of leukocytes in the blood after chemotherapy
It should be borne in mind that leukopenia is a polyetiological syndrome, which can be a primary condition or a complication of other ailments. Among the main possible causes of leukopenia are:
- The problem of congenital genetic defect.
- Myelotoxic leukopenia, which is provoked by taking chemotherapy drugs used to treat oncology, also in the case of a systemic oncological process developing in the human body.
- Tumor lesion of the bone marrow.
- Disturbance of the body's metabolic processes.
- Infectious damage to the body - with rubella virus, cytomegalovirus infection, Epstein-Barr virus, hepatitis, etc.
- For various forms of tuberculosis.
- The effect of drugs for the treatment of diseases of various organs and systems of our body.
- When the patient works with chemicals for a long time.
Diagnosis of leukopenia
Leukopenia can be determined using a general blood test. It shows the concentration of leukocytes in the blood. Additionally, a blood test is performed with leukocyte differentiation: the study helps determine which white blood cells are insufficient. This analysis allows us to identify a range of possible causes of leukopenia. Also, diagnosis of leukopenia includes:
- Hemogram
- determines the absolute number of red blood cells, leukocytes, platelets, shows the percentage of different types of white cells; - Immunological blood test
- detects antigranulocyte and antinuclear immunoglobulins; - Biochemical blood test
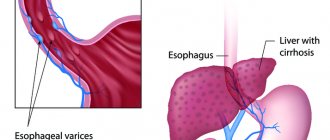
- reflects the amount of folate, vitamin B12, liver transaminases, bilirubin in the blood; - Cytological examination
- aimed at determining the specific type of leukopenia, establishes the mechanism of its development; - Blood test for hepatitis
, rheumatoid factor.
Other studies may be required. They are needed to determine the cause of leukopenia. Some time after the first examination, repeat tests are prescribed - this is necessary to obtain a reliable result.
Treatment of leukopenia during chemotherapy at the Vitamed clinic
In case of severe leukopenia, a comprehensive, attentive approach to treatment is required, combining a set of appropriate actions:
- Treatment of the underlying disease that caused the problem of leukopenia.
- Maintaining sterile and comfortable conditions for the patient.
- Determining the appropriate course of hormonal therapy.
- Developing a diet, making adjustments to the usual diet.
- Measures to prevent infectious complications.
- Stimulation of leukopoiesis.
For the patient, the Vitamed clinic offers a comprehensive approach aimed at accurately diagnosing and solving the problem. The necessary conditions are created for the patient to prevent infectious complications, simultaneously eliminating the root cause of the pathology.
9-20
Treatment methods
At the first signs of infection, patients with leukopenia are prescribed antibacterial drugs. Initially, broad-spectrum antibiotics are used. When the results on the sensitivity of microorganisms are ready, suitable therapy is selected. If the patient's condition improves within 72 hours, then the treatment regimen has been selected effectively. The drugs are continued to be taken for a week or until symptoms disappear completely at the same dosage.
The lack of effect of treatment indicates antibiotic resistance, when microorganisms are resistant to the active ingredients of the drug, or the presence of two or more infections. If the patient has no signs of infection, but the white blood cell count is significantly reduced, prophylactic antibiotic therapy is given. For fungal infections, antifungal drugs are indicated.
Colony-stimulating factors - growth factors - are also prescribed for the treatment of leukopenia. They force the red bone marrow to more actively produce new blood cells. Two types of drugs are used:
- G-CSF
– granulocyte colony-stimulating factors. Promotes rapid growth of neutrophils; - GM-CSF
– granulocyte-macrophage colony-stimulating factors. Causes accelerated production of granulocytes and macrophages.
Glucocorticosteroids, anabolic steroids, and vitamin complexes are prescribed as maintenance therapy. They do not help produce white blood cells, but prevent their rapid destruction.
With the development of a severe infectious process (sepsis, pneumonia, necrotizing enteropathy) and in the absence of effect from antibiotics, a leukocyte transfusion is performed. If leukopenia occurs during radiation or chemotherapy, it is necessary to reconsider the treatment regimen used or replace individual drugs.
Bone marrow transplantation for leukopenia
In rare cases, leukopenia is caused by a low level of agranulocytes in the blood. In this case, drug therapy is ineffective. Chemotherapy, which is necessary to treat cancer, destroys your own bone marrow. To treat this type of leukopenia, a bone marrow transplant is performed - the transplantation of part of the stem cells. They are the ones who will produce new leukocytes.
If the leukocyte count is low, a leukocyte transfusion is also performed. Typically, the procedure is prescribed to patients with a systemic viral infection in the absence of effect from antibiotics. However, in case of local bacteriological inflammation or infection with a virus, transfusion of leukocyte mass does not give any result.
Classification
Before talking about the causes of leukopenia, let's consider its main types. First of all, you need to understand that white blood cells come in different types and they perform different functions. Depending on which cells are missing, there are neutropenia (neutrophils), eosinopenia (eosinophils), monocytopenia (monocytes) and lymphopenia (lymphocytes). If the number of cells is reduced compared to the norm, this is absolute leukopenia, and if only the percentage is reduced relative to other types of leukocytes, this is relative leukopenia.
Physiological leukopenia occurs in 2–12% of people. They do not experience any symptoms, their hematopoiesis is not impaired and their immunity is not reduced. This is their individual norm. Leukopenia resulting from certain diseases is called pathological .
Some people suffer from hereditary leukopenia . There are also many types of acquired leukopenias.
Sometimes the analysis reveals a reduced number of white blood cells because a significant portion of the white blood cells have moved to certain vessels. In such cases they talk about redistributive leukopenia . If the number of leukocytes has decreased throughout the bloodstream, this is true leukopenia .
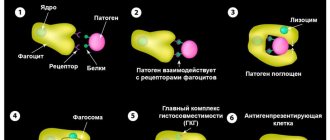
Among all types of leukopenia, neutropenia is the most common. Neutrophils make up the majority of all white blood cells. They play an important role in protecting the body: they perform the function of phagocytes (they absorb and destroy foreign particles, primarily bacteria and fungi), and secrete substances that are involved in the development of inflammation.
Neutropenia comes in three degrees of severity:
- Light: from 1000 to 1500 neutrophils in 1 μl of blood.
- Moderate severity: from 500 to 1000 in 1 µl.
- Severe: less than 500 µl in 1 ml.
Symptoms of acute neutropenia occur within hours or days. Chronic neutropenia lasts from several months to several years.
Our doctors will help you
Message sent!
expect a call, we will contact you shortly
Prognosis and prevention
Mortality from leukopenia during radiation or chemotherapy is 4-6%. If the disease is not caused by oncology treatment, then the rate fluctuates at 5-10%. Just 20 years ago this value reached 20%. A reduction in this parameter was achieved through the development of adequate antibacterial therapy, competent patient care, and the use of CSF.
High mortality is observed in elderly patients, in people with renal and liver failure, if leukopenia is complicated by septic shock or bacteremia. There is no specific prevention of leukopenia. Doctors give the following mandatory recommendations:
- Get a blood test every week;
- Take vitamin complexes;
- Minimize stress and anxiety;
- Wear a protective mask in public places;
- Follow the rules of personal hygiene, take a shower daily;
- Do not come into contact with pets or their feces;
- Avoid shaving, manicuring (anything that could cause injury);
- Avoid working with soil;
- Eat properly and nutritiously;
- Give up bad habits;
- Follow the chemotherapy protocol strictly.
Leukopenia is a dangerous condition. It requires mandatory compliance with all doctor’s recommendations. Ignoring these rules often leads to fatal complications. If you are undergoing chemotherapy, you need to be as attentive as possible to your health. Medscan Medical Center will help you monitor the course of leukopenia and choose effective treatment. Experienced doctors will be able to develop an individual treatment regimen that will reduce the risk of developing any complications.
Symptoms
Leukopenia is often discovered by chance, for example, during preventive medical examinations, since a person may not notice any disorders for a long time. The first signs of leukopenia may be:
- headache;
- dizziness;
- feeling of weakness;
- cardiopalmus;
- bleeding gums, mouth ulcers;
- hoarse voice.
As the pathology progresses, the following are observed:
- increased body temperature;
- fever, chills;
- enlarged tonsils and spleen;
- exhaustion of the body.
High susceptibility to infectious diseases is another symptom that may indicate leukopenia.
Depending on the number of leukocytes, three stages of pathology are distinguished: first (less than 1.5 g/l), second (1 g/l) and third (0.5 g/l). At the third, most severe stage, called agranulocytosis, thrombocytopenia may develop, a pathology characterized by a decrease in the number of platelets, which threatens bleeding and hemorrhage.
Agranulocytosis is a severe pathology in which the number of leukocytes and granulocytes sharply decreases. Since granulocytes provide antimicrobial protection to the body, a critical decrease in their number can lead to serious infectious complications, including death. A patient with this diagnosis is prescribed hospitalization and emergency treatment in the hematology department, with the obligatory creation of aseptic conditions.
Acute leukopenia can last up to three months; for longer periods, a diagnosis of chronic leukopenia is made.