Pulmonologist
Prokhina
Maria Egorovna
Experience 38 years
Pulmonologist
Make an appointment
Pulmonary edema is a pathological, very serious condition, which is characterized by the release of transudate into the lung tissue. As a result, gas exchange is disrupted, which leads to serious consequences, including death.
Emergency care for pulmonary edema is the only thing that can increase the patient’s risks of survival and recovery. A person in such a situation requires immediate medical attention.
Pulmonary edema itself is most often a complication that accompanies serious problems of organs and body systems, for example, the cardiovascular system, gastrointestinal tract, etc.
The main symptoms of pulmonary edema in humans
Pulmonary edema is a life-threatening condition for the patient that requires urgent hospitalization and emergency care.
The pathology is characterized by the accumulation of intercellular fluid inside the alveoli and in the lung tissue. The main symptoms of pulmonary edema in humans in the initial stage are: increasing weakness, tachycardia, increased sweating, dry paroxysmal cough, worsening in a lying position. Depending on the course, the following types are distinguished: acute, subacute, fulminant and prolonged edema. The main reasons for the development of pathology:
- acute intoxication of the body;
- acute left ventricular failure;
- chronic lung diseases;
- TELA;
- severe traumatic brain injury with convulsive activity;
- long-term artificial ventilation;
- diseases accompanied by increased intracranial pressure.
The main causes of toxic pulmonary edema: inhalation of irritating or suffocating gases.
Diagnostics
If the symptoms of pulmonary edema are not pronounced, additional studies are required in parallel with emergency care:
- biochemical screening. This is a blood test;
- study of blood gases;
- ECG, ultrasound of the heart;
- X-ray of the chest area;
- pulmonary artery catheterization.
In many cases, diagnosis of pulmonary edema is possible immediately - only based on the signs that appear visually in the patient and without additional examination.
Classification of pathology
There are cardiogenic, non-cardiogenic and mixed pulmonary edema. Non-cardiogenic edema is a condition not associated with heart disease. This term combines toxic, nephrogenic, allergic and other forms of pulmonary edema. Cardiogenic is a consequence of heart disease. First aid for pulmonary edema due to heart failure will be discussed below.
Classification according to the development of pathology:
- fulminant edema (develops very quickly and, as a rule, ends in the death of the patient);
- acute (develops within 4-6 hours and is a complication of heart attack, severe traumatic brain injury and anaphylaxis);
- subacute (characterized by a wave-like increase in symptoms, being a complication of uremia and liver failure);
- prolonged edema (develops over the course of a day and is characteristic of chronic lung diseases).
Mechanism of edema development
Normally, lung tissue consists of many tiny air-filled bubbles called alveoli. If, in addition to air, liquid begins to accumulate in the alveoli - as a result of sweating from the circulatory and lymphatic systems - pulmonary edema occurs.
The mechanism of occurrence of this pathological condition is as follows:
- As a result of stagnation in the pulmonary circulation, the outflow of blood and lymph is disrupted and intravascular pressure in the pulmonary capillaries and lymphatic vessels increases.
- Blood and lymph accumulate in the vessels and begin to penetrate through their walls into the pulmonary structures of the alveoli - the so-called fluid effusion occurs.
- The liquid or transudate that has penetrated into the alveoli seems to displace air from them and significantly reduce their respiratory surface. The situation gets worse as the amount of transudate in the lungs increases - the effect of “internal drowning” is observed when the lungs fill with water and cannot fully function.
- Transudate is very rich in protein and therefore easily foams when in contact with air in the alveoli. The resulting foam makes breathing even more difficult.
- As a result, breathing becomes almost impossible, oxygen does not enter the blood, hypoxia and death occur.
Clinical manifestations in adults
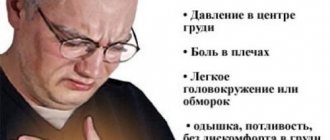
Pathology does not always develop rapidly. In some cases, it is preceded by weakness, dizziness, chest tightness, dry cough, headache and tachypnea. These symptoms can appear a few minutes or several hours before swelling develops.
Primary manifestations: compressive chest pain, increasing tachycardia, dry wheezing turning into wet wheezing, increased breathing.
Signs of progression of pathology:
- shallow breathing;
- bubbling wet rales;
- earthy skin color;
- increased suffocation;
- cold sweat;
- the appearance of foamy sputum with a pink tint from the mouth.
On our website Dobrobut.com you can learn more about pathology and, if necessary, make an appointment with a specialist. The doctor will answer questions and tell you the difference between interstitial and alveolar pulmonary edema.
Wheezing when breathing
Noises of pathological origin may occur in the respiratory tract. Such noises, better known as wheezing, can be detected in any area of the respiratory system: in the lungs, trachea, bronchi, and so on.
Wheezing as a symptom of illness
Wheezing is a characteristic manifestation of most diseases or pathological changes in the respiratory system. Among them:
- bronchial asthma ;
- anaphylaxis (instant allergic reactions);
- COPD;
- broncho- and pulmonary pneumonia. bronchitis. tracheitis. tuberculosis;
- pulmonary infarction, cancer, pulmonary edema. bronchiectasis and other diseases.
Causes of wheezing
The mechanism of wheezing, as well as the location and intensity of its manifestation, differ depending on the reasons for the occurrence of this symptom. Noises in the respiratory organs appear as a result of two main pathological processes:
- narrowing of the lumens in the bronchi as a result of inflammatory changes or spasms in them;
- the lumen of the respiratory tract is clogged with mucopurulent substances of varying degrees of viscosity and density, which means that during inhalation and exhalation these masses will be in constant motion.
Characteristic features of noise
Only a specialist can recognize what type of wheezing this or that noise belongs to.
Wet wheezing
The so-called moist rales are the result of the accumulation of sputum (liquid mucus) in the bronchi. The doctor can determine their type after auscultation: when an air flow passes through the sputum, bubbles form in it, which constantly burst. This “mass explosion” provokes the formation of moist rales. Basically, this manifestation occurs when inhaling, less often it can be recognized when exhaling air from the lungs.
The size of air bubbles may vary. This directly depends on the mass of accumulated mucus, the diameter of the bronchi and the volume of the cavity itself. Accordingly, small-, medium- and large-bubble moist wheezing is distinguished.
Bronchopneumonia. pulmonary infarction and bronchiolitis are characterized by fine-bubble noises, similar to the noise of foaming soda.
Medium vesicles are formed as a result of bronchiectasis or hypersecretory bronchitis. To the ear, such wheezing resembles the sound of air blowing into a liquid through a straw. The same wheezing may indicate small abscesses in the lungs (bronchi) that accompany the development of pneumonia, or can be heard at the first stage of pulmonary edema. A type of medium-bubble noise is the so-called “crackling” noise, they appear due to the opening of the walls of the bronchioles and acini, closed by the surrounding tissue during exhalation. This symptom allows one to diagnose, for example, pneumosclerosis or pulmonary fibrosis.
Large-bubbling or “bubbling” wheezing occurs when mucus accumulates in large bronchi, trachea, or in large cavities of pathological origin. This noise is heard on auscultation when air passes through the organs during inspiration. Note that you can hear bubbling wheezing even without the help of a phonendoscope; they can be heard even at some distance. Such symptoms are characteristic of the late stages of pulmonary edema. Also, similar accumulations in the trachea or bronchi can form in patients who have a weakened (or absent) cough reflex.
Dry wheezing
The second type of wheezing is dry. Among them are “whistling” and “buzzing”.
A whistling noise is a sign of an asthma attack. Such noises are produced by the bronchi as a result of uneven narrowing of the lumens during bronchospasm.
“Buzzing” when breathing is observed in those patients in whom thread-like mucous bridges form in the lumens of the bronchi due to inflammation.
Treatment of wheezing when breathing
To relieve a patient of wheezing, it is necessary first of all to properly treat the disease that causes it. Treatment methods differ significantly for different diseases and types of murmurs. The most commonly prescribed types of drug therapy are:
- Mucolytics are used to thin sputum and simplify its discharge;
- eliminating spasms and relaxing the walls of the bronchi is a task that inhaled beta-adrenergic agonists can do;
- An inflammatory process in the respiratory system caused by a bacterial infection is an indication for the prescription of antibiotics.
Algorithm of action for pulmonary edema
The future fate of the patient largely depends on the correct and timely provision of pre-medical care.
Algorithm of action for pulmonary edema:
- sit the patient down and remove the foam;
- relieve pain syndrome;
- give vasodilators;
- apply venous tourniquets to the limbs.
In addition, it is necessary to monitor blood pressure, pulse and respiration rates.
Emergency care for acute pulmonary edema after the arrival of an ambulance is intravenous administration of promedol (morphine) and Lasix. For bronchospasm, the use of dexamethasone is justified. Mandatory measures: oxygen therapy and the use of electric suction to prevent foam aspiration.
Main complications after emergency care
Such complications include:
- development of a fulminant form of edema;
- intensive foam production can cause airway obstruction;
- depression (depression) of breathing;
- tachyarrhythmia, asystole;
- angiotic pain. Such pain is characterized by an unbearable pain syndrome; the patient may experience pain shock, worsening the prognosis;
- impossibility of stabilizing blood pressure. Pulmonary edema often occurs against a background of low and high blood pressure, which can alternate within a large amplitude. The vessels will not be able to withstand such a load for long and the patient’s condition worsens;
- increase in pulmonary edema against the background of high blood pressure.
Hospital treatment
Treatment of the pathology is carried out in a hospital setting and includes the following measures: oxygen therapy, the prescription of diuretics and cardiac glycosides, intravenous administration of albumin, heparin, atropine, aminophylline. In some cases, hormones are prescribed. All prescriptions are strictly individual and are adjusted taking into account the patient’s condition.
The prognosis for treatment of cardiogenic pulmonary edema depends on the type of pathology, severity, presence of concomitant diseases, as well as the quality of medical care provided.
Consequences of pulmonary edema in the elderly, prevention
Considering the severity of the disease, the prognosis in most cases is disappointing. And even if the swelling was managed in a timely manner, there is a high probability of ischemic damage to internal organs and the development of congestive pneumonia. In the absence of an established cause, there is a high risk of re-development of edema.
If we talk about the consequences of pulmonary edema in older people, then we are talking about the development of pneumosclerosis. Quite often such patients fall into a coma.
Prevention of pathology consists of early detection of diseases, the complication of which is edema, and their effective treatment.
If you have any questions, please contact our medical center. Specialists will answer all questions, including “why the lungs swell in a bedridden patient,” help determine the diagnosis and prescribe an effective course of treatment after receiving the examination results.
Related services: Ambulance call 5288
When?
NOL “emerges” due to increased filtration of fluid (i.e., its movement) through the vascular wall of the capillaries of the lungs and increased vascular permeability. When excess fluid accumulates and the functioning of lymphatic vessels decreases. The accumulated fluid fills the alveoli (the unit that makes up the lung), resulting in a severe deterioration in important gas exchange (oxygen and carbon dioxide).
NOL occurs due to acute lung damage due to sepsis and radiation, acute infectious diseases of the respiratory tract, inhalation of toxic substances, trauma, and high-altitude illness (with a rapid rise to an altitude of 3-4 km above sea level). It also appears in diffuse alveolar hemorrhagic syndrome, hemorrhagic fever, in patients with lung cancer, in surgical patients who have undergone volume transfusions of solutions and various drugs. The formation of NOL is possible in patients with PE (pulmonary embolism), in elderly people who have been taking acetylsalicylic acid drugs for a long time, in people taking narcotic drugs (heroin, methadone).