October 22, 2012
There are eight blood types, which are determined by the presence or absence of certain antigens. Why is it necessary to know yours?
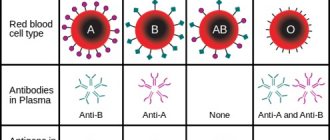
Different people have approximately the same blood composition: it contains the same basic elements. However, there are eight types of blood
, which are determined by the presence or absence of certain antigens.
These substances can cause a reaction from the immune system if they are foreign to it. Blood is divided into four groups according to the type of antigens
, as well as into two large groups
according to the presence of the Rh factor
.
How were blood groups discovered?
Experiments with transfusions of blood or its components have been carried out for hundreds of years.
For some, this treatment saved their lives, but most patients died after the transfusion. The reasons for this remained unknown until 1901, when the Austrian physician Karl Landsteiner discovered differences between blood samples from different people. How to become a donor?
Who can become a donor, how safe is it and how to prepare for blood donation? The answers to these and other questions are in the article on blood donation.
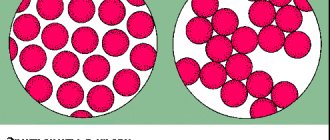
Thus, during experiments, Landsteiner noticed that in some cases mixing the blood of two patients can lead to agglutination - the clumping of red blood cells.
It turned out that it is this process that leads to fatal consequences. As it turned out, incompatibility of blood from different people is caused by the response of the immune system. If the recipient has antibodies against donated blood cells, the immune system tries to get rid of the foreign cells. The work of Karl Landsteiner made it possible to identify four blood groups and make blood transfusions safe
.
For this discovery, the scientist was awarded the Nobel Prize in Physiology or Medicine in 1930.
What other group classifications are there?
Research in the field of hematology is gradually expanding the list of classifications that are taken into account during blood transfusions and can reduce the likelihood of developing both quickly occurring and delayed complications.
The following additional identification systems exist:
NameDescription
| Kell | The factors included in this classification follow Rhesus and the ABO system in terms of immunogenicity. This means that it is impossible not to take into account the peculiarities of these antigens during transfusions: this will end disastrously for the recipient. The classification is taken into account not only for blood transfusions, but also when monitoring the course of pregnancy in cases where the risk of an immune conflict is increased. There are two specific proteins in this system, and they are designated by the letters: “k” and “K”. |
| Duffy | In terms of the severity of the immune response, it follows the Kell system, but these protein compounds do not lead to the development of hemolytic disease during pregnancy. Complications may develop during blood transfusions. |
| Kidd | Contains two antigen proteins, which form three possible varieties. They do not lead to severe immune reactions if uncontrolled, but can still lead to some complications. Few people have them. |
| MNSs | It has four factors that give a total of nine genotypes. Belongs to the most difficult categories. Antibodies are inactive, but in some cases lead to hemolytic disease and complications during transfusions. |
| Lutheran | This type of antibody is rare and inactive: immune reactions associated with it have not been identified. |
| Levis | It includes two types of antigens that form three phenotypes and rarely lead to complications. |
| Vel-negative | It is rare and can lead to significant complications, especially in the presence of severe diseases. The protein compound was discovered in 2013, but medicine encountered incompatibility due to it earlier. |
Clinics that do not specialize in hematology do not have the ability to thoroughly determine blood characteristics. And usually this is not necessary: the classical AB0 and Rh systems are sufficient for transfusions.
What are blood groups?
The difference between the blood of different people lies in the presence or absence of certain protein molecules
called
antigens
.
They are located on the surface of red blood cells, erythrocytes and in the blood serum. It is these proteins that are responsible for the immune system’s reaction to “foreign” blood. The combinations of these molecules vary from person to person. They depend on the genetic information that people inherit from their parents. The blood group is determined by the presence or absence of two antigens A and B on the surface of red blood cells and antibodies to them in the blood plasma. In Russia, it is usually customary to name blood groups by numbers
: first, second, third and fourth.
In international practice, the designation of blood group follows the AB0
: 0 - First group, A - second group, B - third group, AB - fourth group.
- The first (0) blood group has antibodies A and B only in the blood plasma.
- The second (A) group has antigen A on the surface of red blood cells and antibodies B in the blood plasma.
- The third (B) group has antigen A in the blood plasma and antibodies B on the surface of red blood cells.
- The fourth (AB) group has A and B antigens on the surface of red blood cells.
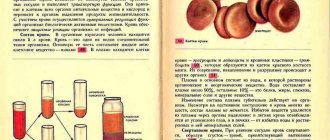
Blood and its antigens
This liquid tissue of the body unites all organs and systems into a single whole and connects every cell. It is not surprising that its indicators can tell a lot about the state of the body, identify diseases and the smallest disturbances in metabolic processes. Blood consists of a liquid part - plasma, in which there is a large amount of proteins and salts, and formed elements:
- red blood cells that carry oxygen thanks to hemoglobin;
- leukocytes involved in immune defense;
- platelets responsible for clotting
The membrane of red blood cells contains proteins or protein-carbohydrate complexes called antigens. They are needed to transport other molecules out of cells and support the structures of red blood cells. They detect foreign agents and destroy them, they also determine the blood type.
Rh factor
In addition to antigens A and B, many people also have the so-called Rh factor on the surface of their red blood cells. This is also an antigen that is shared by 85 percent of Europeans and 99 percent of Asians. Such people are called Rh positive or RH+
.
Those who do not have the Rh factor in their blood are called Rh negative or RH-
. If blood is transfused from a person with a negative Rh factor to a person with a positive Rh factor, no problems arise. Otherwise, Rh antibodies begin to be produced in the recipient’s blood, which lead to the destruction of red blood cells. Taking into account the presence of the Rh factor, a total of eight blood groups are obtained: 0 Rh+, 0Rh-, A Rh+, A Rh-, B Rh+, B Rh-, AB Rh+, AB Rh-.
Nutrition
The irrepressible passion of representatives of the third positive group for everything “delicious, sweet, spicy” and the desire to pamper themselves with a loved one can create health problems such as digestive disorders, intestinal dysfunction, the development of diabetes and obesity.
Taking into account the fact that the body of “nomads” is, in principle, omnivorous, intolerance to any product is not typical, it is easy for them to choose a diet that would be healthy, tasty and not harmful. For this purpose, the following products are recommended:
- dishes made from lean meats;
- fish and seafood dishes;
- various porridges, with a preference for rice and oatmeal;
- eggs;
- low-fat dairy products, including cheeses;
- boiled and raw vegetables in the form of salads with vegetable oil;
- drinks made from medicinal herbs (chamomile, St. John's wort, lemon balm, rose hips).
Products that are not recommended for consumption:
- pork meat, lard and fatty chicken;
- smoked meats;
- tomatoes and dishes made from them, tomato juice and ketchup;
- all kinds of sweets - ice cream, pastries, pies, sweets, they should be replaced with fruit, or light fruit cakes without baking.
Acceptable, but with restrictions: black tea and coffee, corn, legume dishes, nuts, spicy and hot seasonings. Meals should be more frequent, without waiting for feelings of extreme hunger, when overeating is often allowed.
What if you mix blood from different groups?
If the blood types of the donor and recipient are incompatible, agglutination
- the sticking together of red blood cells due to the interaction of antigens. This process occurs if, for example, a person with blood type B receives the blood of a person with blood type A. Agglutinated red blood cells clog the blood vessels and stop blood circulation. This process resembles the formation of blood clots, although it is caused by other reasons. In addition, “broken” red blood cells lose hemoglobin, which, once outside the cell, becomes toxic. This can lead to fatal consequences.
Blood type diet: expert opinion
Is it worth trying the blood type diet? Commented by Tatyana Shapovalenko, chief physician of the Treatment and Rehabilitation Center of the Russian Ministry of Health.
What is Rh incompatibility?
The presence of a negative Rh factor (Rh(-) factor) in the mother and a positive Rh factor (Rh(+) factor) in the father is called Rh incompatibility.
Rh Factor is a small protein antigen on erythrocytes, our red blood cells. Most people have them, then they talk about the Rhesus (+) factor, if a person does not have them Rhesus (-). There are 3 types of antigens (CDE), but the antigen that causes the most trouble is D.
In this case, the blood group can be any (i.e., a pregnant woman and her husband can be with any combination of groups I, II, III, IV), only the above-mentioned combination of Rhesus is Rh-incompatible.
The combination is the opposite, i.e. a mother with Rh(+) and a father with Rh(-), or a coincidence of Rhesus, are not Rhesus incompatible.
The child may inherit Rh negative or Rh positive. If Rh(-), then there will be no problem. However, with a Rh positive factor, in some cases a Rh conflict may develop. I would like to immediately reassure parents who have Rh incompatibility: nowadays, thanks to vaccinations, early diagnosis and control, Rh conflict develops extremely rarely.
Rh incompatibility is observed on average in 13% of couples, but only 1% develop Rh conflict. Thus, Rh incompatibility and Rh conflict are not the same thing, and not every couple with Rh incompatibility has an Rh conflict. I am writing about this in such detail because there is a lot of confusion. Unfortunately, not only on the part of patients, but also on the part of doctors. Married couples often come to us, saying with tragedy in their voices that they are Rhesus incompatible and they will most likely have a miscarriage or a dead child!!!
What happens with Rhesus incompatibility?
If there is Rh incompatibility, if the child is Rh positive, during pregnancy or childbirth red blood cells (erythrocytes) of the fetus can enter the mother's bloodstream. Only then, when the blood of mother and fetus mixes, does the protective mechanism start. Fetal red blood cells contain Rh positive antigens (including the strongest D antigen). Mom will protect herself from them (there are none in her body!), producing antibodies (her army) of two types: M and G, in order to destroy foreign bodies. Normally, the blood of the child and the mother do not come into contact: the mother has her own circulatory system, the fetus has its own. Only useful substances that serve the nutrition and growth of the fetus are supplied to it from the mother. Moreover, before getting to the child, they must pass the placental barrier - a strict inspector who blocks the path to suspicious and obviously harmful substances. Antibodies M do not pass through this barrier, so they do not harm the child. Antibodies G are produced slowly, over 3-6 weeks, and in later stages are also not dangerous. Since there were no antibodies before pregnancy, during the first pregnancy, as a rule, a conflict does not occur: because for the first time, the mother’s body produces it in very small quantities.
The problem is that our defense mechanism is a very cunning thing: as in the case of fighting an infection, the immune system retains the memory of the enemy. During subsequent pregnancies (again, only in the case of inheritance of positive Rh!) the production of antibodies by the body prepared for the meeting occurs at a much higher speed and in greater quantities. Then G antibodies can enter the blood of the fetus in order to destroy antigens, but at the same time the red blood cells of the fetus are destroyed, which leads to the development of intrauterine hemolytic anemia of varying severity.
With a mild degree of anemia, no changes are visible on fetal ultrasound; with a moderate degree, a condition called Erythroblastosis is observed (replacement of destroyed red blood cells with a young team, as a protection against anemia). At the same time, the pigment bilirubin is released from the destroyed red blood cells, a substance that is deposited in the tissues of the body, coloring them yellow (jaundice) and is also very dangerous for the fetal brain. In addition, due to developing heart failure, the fetus experiences fluid retention in the body: between the membranes of the abdominal cavity, around the lungs, heart, etc.
This condition is called Hydrops fetalis and is life-threatening. Fortunately, severe complications in the fetus develop extremely rarely: only 10% of all cases of Rh conflict. Let me remind you of the statistics: Only 13% of couples have Rh incompatibility, only 1% of these couples develop Rh conflict, and only 10% of all Rh conflicts have a severe disease! Most often, these are cases when the pregnant woman did not visit doctors, did not register on time, or refused the Rho-gam injection. Therefore, early consultation with a doctor and regular monitoring will help you give birth to a healthy baby.
Conditions under which blood contact between mother and fetus may occur:
| Threatened miscarriage accompanied by bleeding |
| Miscarriage |
| Abortion |
| Frozen pregnancy |
| Ectopic pregnancy |
| Chorionic villus biopsy |
| Amniocentesis |
| Low placenta previa |
| Placental abruption |
| Pregnancy with twins |
| Trauma during pregnancy |
| Childbirth (both caesarean section and normal) |
What to do?
In the above cases, to destroy the antigen in the mother’s body, the mother is immunized: injection of anti D-gamma globulin (Rhogam 300 mgr) during the first 3 days after the above conditions. Anti D-gamma globulin (another name for anti-Rhesus D-immunoglobulin) destroys the D antigen in the body of a pregnant or postpartum woman and prevents an immune reaction from starting. Since the antigens will be neutralized, the mother will not need to produce antibodies and there will be no danger in subsequent pregnancies. Literary data suggests that it is not too late to carry out immunization within 14-28 days (as mentioned above, dangerous G antibodies are formed within 3-6 weeks), but in practice they try to give an injection in the first 3 days.
How is pregnancy managed with Rh incompatibility and is Rh conflict diagnosed?
If the pregnant woman is Rhesus negative and her husband is Rhesus positive, at the first visit an antibody test called the Indirect Coombs test is performed. If the result is (-) (i.e. everything is fine, no antibodies were formed), the analysis is repeated at 20 weeks and then monitored every 4 weeks. If the result is positive, i.e. the presence of antibodies is detected, their level in the blood is determined: 1/16 - no risk to the fetus, 1/32 and above: additional research is necessary: a detailed ultrasound of the fetus in the perinatology department and amniocentesis. Amniocentesis is the removal of a small amount of amniotic fluid using a procedure very similar to a regular injection, only in the umbilical area of a pregnant woman. In this case, it becomes possible to assess the condition of the fetus (degree of anemia) and develop treatment tactics: deciding on the issue of intrauterine blood transfusion to the child (replacing destroyed fetal red blood cells and thus compensating for anemia) and early delivery.
Blood group incompatibility
Is blood type incompatibility possible? As a rule, if the mother has group I (O), the father has group II (A) or III (B), and, accordingly, the child has group II (A) or III (B), they say incompatibility by blood group. Occurring in approximately 20% of cases (even more often than Rh incompatibility), it is not of great importance in practice because If a conflict develops, it proceeds in a very mild form. Unlike Rh conflict, it can develop during the first pregnancy, but does not become more dangerous during subsequent ones. The reason for the mild course is a lesser defensive reaction, because there are few A and B antigens on the surface of red blood cells; the formation in the mother’s body most often of M antibodies, which do not pass through the placenta, and the formation of G antibodies in very small quantities. Due to the ease of the course, there are no tests for intrauterine detection of blood group conflict, amniocentesis and treatment before birth are not required. If after birth the baby develops early jaundice (due to the destruction of red blood cells and the deposition of bilirubin in tissues), a group conflict is suspected and a Coombs test is performed. As a rule, phototherapy is sufficient for treatment.
This is interesting
1. Combination of conflict according to Rhesus and Group
If there is a blood group conflict, the Rh conflict proceeds much easier. Maternal antibodies against A and B antigens reduce the number of Rh(+) red blood cells in the fetus (acting similarly to an injection of anti-D-gamaglobulin).
2. Theory of Rhesus transmission from grandmother (Grandmother Theory)
According to this theory, Rh antigens of the fetus are inherited from the child's grandmother (mother's mother). For example: the child is Rh(+) and the mother is Rh(-). So the grandmother was Rh(+). Or vice versa, a Rh-positive mother has an Rh(-) child. Look at my mother's Rh: it will be negative!
Briefly
Rh incompatibility is a negative Rh factor (Rh(-) factor) in the mother and a positive Rh factor (Rh(+) factor) in the father.
Rh factor: protein bodies (antigens) on red blood cells. They either have a Rh (+) factor or they don’t: Rh (-).
If the child inherits the Rh(-) factor there will be no problem. With a Rh positive factor, Rh conflict can develop: in only 1% of cases of Rh incompatibility.
The following conditions can cause Rh conflict: miscarriage, abortion, frozen pregnancy, ectopic pregnancy, bleeding during pregnancy, twin pregnancy, childbirth, amniocentesis, chorionic villus biopsy, trauma during pregnancy, low placenta previa.
In these cases, the mother is immunized: an injection of anti-D-gamma globulin during the first 3 days. Anti D-gamma globulin destroys the D antigen in the body of a pregnant or postpartum woman and prevents an immune reaction from starting.
Management of pregnancy: if the pregnant woman has a negative Rh and the husband has a positive Rh, at the first visit an antibody test is performed, which is subsequently monitored every 4 weeks. If the result shows the presence of antibodies, their level in the blood is determined: 1/16 - no risk to the fetus, 1/32 and above: additional research is required: detailed ultrasound of the fetus in the perinatology department and amniocentesis. At the same time, the condition of the fetus is assessed,
Treatment tactics:
Observation (sufficient in 90% of cases).
Intrauterine blood transfusion to a child.
Early delivery.
Compatibility of different blood groups
Despite the difference in antigen content, in some cases, blood transfusion from a donor to a recipient with different blood groups is possible. The transfusion will be safe if the recipient does not have antibodies to the donor antigens. Thus, people with blood group 0 Rh-
are considered universal donors, since they do not have antigens or the Rh factor on the surface of their red blood cells.
AB Rh+
blood group are considered universal recipients, since their blood plasma does not contain a single antibody to the antigen and contains the Rh factor.
Blood type compatibility
Compatibility rules. This information will make it possible to understand how many blood groups are suitable for other types of transfusion.
RecipientDonor material
| I, Rh- | I, Rh+ | II, Rh- | II, Rh+ | III, Rh− | III, Rh+ | IV, Rh- | IV, Rh+ | |
| I, Rh- | + | |||||||
| I, Rh+ | + | + | ||||||
| II, Rh- | + | + | ||||||
| II, Rh+ | + | + | + | + | ||||
| III, Rh− | + | + | ||||||
| III, Rh+ | + | + | + | + | ||||
| IV, Rh- | + | + | + | + | ||||
| IV, Rh+ | + | + | + | + | + | + | + | + |
But later more and more new factors were discovered that were important to take into account. Nowadays, in medical institutions, blood is transfused to patients, which is pre-tested for compatibility and fully complies with their basic characteristics.
In some cases, material from universal donors is used, but this usually happens when there is no access to suitable material, and action needs to be taken as quickly as possible.
A hematologist is a medical specialist involved in a field that deals with the circulatory system.
He knows everything about human blood groups and treats diseases in which hematopoietic structures do not function correctly.