Diagnostics
Suspicion of a lacunar infarction appears only if the patient suffers from arterial hypertension, diabetes mellitus or diseases associated with cerebral vessels. Due to the difficulties caused by the specificity of symptoms, it often takes a very long time to make a final diagnosis. First, the neurologist conducts a survey, and then necessarily prescribes the following examinations:
- Laboratory blood tests;
- CT scan;
- Magnetic resonance imaging;
- Angiography of cerebral vessels.
Modern medicine makes it possible to accurately and quickly identify any disturbances in the functioning of the body. However, in the case of lacunar stroke there are a number of problems:
- Consequences of the disease
- Classification
- Treatment of ischemic stroke of the brainstem and lacunar
- Rehabilitation period
- Treatment of lacunar stroke
- Treatment tactics
- Features of the development of lacunar stroke
- Danger and consequences
- Cerebral infarction (lacunar infarction)
- Clinical picture
- 5 Causes of lacunar stroke
- Forecast and consequences
If the cause of a stroke is an increase in blood pressure, then there may be cases where the deviation from the norm is so insignificant that doctors do not take it into account. Therefore, they begin to look for other reasons why the patient experiences certain symptoms
At this time, the patient’s condition may worsen, which, as it later turns out, was caused by circulatory disorders associated with increased blood pressure. The size of the gaps can be extremely small, which is why even modern equipment will not allow them to be noticed during the first study. This is why sometimes doctors have to perform a CT or MRI again. Gaps may not be identified immediately. This is due to the fact that on CT or MRI they appear in real form only a week after formation. Until this point, they are either visible in a much smaller and lower-density state than they actually are, or not visible at all. Symptoms appear gradually. Even after a serious circulatory disorder, the patient may not have any external signs of a stroke. The condition usually worsens over several days. For this reason, there are great risks of not identifying the disease at all until the patient’s health deteriorates critically. Angiography may not show any abnormalities that could indicate a problem with the blood vessels in the brain. There is no guarantee of their detection even with repeated studies.
All these problems make lacunar ischemic stroke a particularly dangerous phenomenon. Only the highest quality and responsible examination will identify violations in the first days. But even with the work of highly qualified doctors and the availability of modern equipment, there is no guarantee of a quick correct diagnosis.
Etiology of the disease
The causes of lacunar stroke are as follows:
- Uncontrolled arterial hypertension with severe pressure surges, crises in the absence or improper therapy;
- diabetes mellitus, in which the metabolism of carbohydrates and electrolytes is disrupted;
- pathologies with increased blood clotting and the risk of blood clots, including erythremia, extensive injuries and burns, shock, dehydration caused by prolonged vomiting and diarrhea;
- arteritis caused by infection or allergy and poor circulation;
- atherosclerosis, in which there is an imbalance in blood circulation, as a result of which the brain does not receive enough nutrients, which causes the progression of hypertension;
- genetic changes in the structure of the artery wall.
Sometimes the disease can provoke non-ischemia and tissue necrosis, as well as minor hemorrhages in the area, as a result of which the piercing vessels thicken, reduce the amount of hyaline and stick together.
Figures and facts
- More than 400,000 strokes are registered annually in Russia, with a mortality rate reaching 35%.
- The overall risk of recurrent stroke in the first 2 years after the first stroke ranges from 4 to 14%.
- With an increase in potassium intake with food (potatoes, beef, bananas), a significant decrease in blood pressure was noted in individuals with moderately elevated levels by 11.4/5.1 mm Hg. Art.
- In patients receiving diuretics (diuretics) for a long time, hypokalemia develops (diagnosed when the potassium concentration is less than 3.5 mmol/l) and an increase in the incidence of cardiovascular complications.
- By increasing daily potassium intake by 10 mmol (for example, when taking the drug potassium and magnesium aspartate), the risk of fatal stroke is reduced by 40%.
Classification
Clinical classification is based on clinical symptoms and is discussed in the section on symptoms of lacunar infarction.
In the development of the disease there are:
- the most acute period is the first 3 days;
- acute – 28 days;
- early recovery – the next 6 months after suffering a circulatory disorder;
- late recovery – for 2 years.
Due to mild symptoms and the absence of pronounced motor, speech and sensory disorders, it is very difficult to describe the features of each interval. Therefore, this division is of secondary importance.
Treatment of ischemic stroke of the brainstem and lacunar
The most common brain disease that leads to disability and death is stroke. Stroke is often caused by blockage of blood vessels. This is caused by elevated cholesterol levels. If you want to be healthy and not encounter this disease, watch what you eat.
Ischemic stroke treatment
Treatment in the acute period is the most important, then treatment of ischemic stroke proceeds as follows:
- normalize respiratory function normalize the functioning of the cardiovascular system correct blood pressure antioxidants vitamins neuroprotectors
After the rehabilitation period, regular consultations and examinations with the attending physician and a visit to the sanatorium are prescribed.
Treatment of ischemic stroke of the brain is quite serious, since the flow of blood to the brain is stopped. The first thing they do is hospitalize the patient. They are already conducting a thermogram, which will help determine the degree of brain damage and the type of stroke, and based on this they make a prescription for stroke treatment.
After treatment and discharge, the patient continues to undergo rehabilitation, since it is necessary to eliminate the consequences of a stroke as much as possible, restore the functions of the brain and other affected parts of the body.
Ischemic stroke left side treatment
Each side of the brain is responsible for a specific area of human life.
Right hemisphere for:
Which hemisphere is affected, those abilities are distorted, speech and many other visible signs of a stroke are often affected.
Treatment of ischemic stroke drugs
Drug treatment of ischemic stroke:
- Anticoagulants - nadroparin, heparin, enoxyparin, daltoparin
- Neuroprotectors - glycine, piracetam, cerebrolysin, pentoxifylline, vinpocetine, calcium channel blockers and instenon
- Recovery - ginkgo biloba, vinpocetine, pentoxifylline, piracetam, phenotropil
In principle, these drugs are the standard treatment for ischemic stroke.
Drugs for the treatment of ischemic stroke:
Ischemic stroke treatment and recovery are interconnected, since after hospitalization the treatment does not end, there is also a course of physical therapy and massage.
Stem ischemic stroke treatment
A brain stem stroke is one that occurs in the brain stem.
Causes of brainstem stroke:
- hormonal contraceptives, taken for a long time
- control heart rate
Ischemic stroke symptoms, treatment, symptoms:
- pale skin or red face
- blood pressure increases
- breathing and blood circulation are impaired
Repeated ischemic stroke treatment prognosis In half of the cases the disease recurs, but in 70% it leads to death. You need to monitor your health before a relapse occurs.
Lacunar ischemic stroke treatment
Lacunar ischemic stroke provokes heart attacks.
Often in the evening I had a headache and high blood pressure, and in the morning the first symptoms appeared - fatigue, numbness, disorientation.
Lacunar ischemic stroke can be treated well; you need to start treatment on time and remember that lifestyle is the key to recovery.
If a stroke occurs - assessment of the person’s condition, symptoms and first aid
If you notice the first symptoms, which is typical for an ischemic stroke, then you need to call an ambulance as soon as possible. A quick response will save time, and therefore increase the chance of reducing the various consequences of this unforeseen disease.
When diagnosing yourself, you need to pay attention to the following signs - what is included in an ischemic stroke, symptoms:
- weakness, loss of sensation, numbness in the face, arms or legs. Most often on one side of the body;
- decrease or loss of vision;
- loss of speech, difficulty pronouncing a word or sentence, impossible to understand someone else's speech;
- severe headache without any reason, which does not go away with the use of medications that previously helped;
- memory loss;
- it is difficult to navigate in space and perceive what is happening;
- nausea;
- vomit;
- swallowing disorder;
- loss of balance for no apparent reason.
The above signs of ischemic stroke are quite difficult to remember. To make it easier for you, experts have developed a special test that helps identify stroke symptoms and quickly provide assistance for ischemic stroke. It is called FAST - after the first abbreviations of human body parts.
FAST = FAST
Face - face
Arm - hand
Speech - speech
Time - time
We have described how to use the test in the instruction table:
| Part of the body | What to do | If it's a stroke, then... |
| Face | Ask the person to smile or show their teeth | An asymmetry appears on the face: the lips on one side of the face will rise in a smile, and on the other they will be lowered down. |
| Hand | Ask the person to raise both arms and hold them there for 5 seconds. | One hand will go down at once |
| Speech | Ask the person to say a simple phrase, for example, “the sun is bright outside.” | A person may not understand what you asked to do, and if he understands, the spoken phrase will sound incomprehensible, incoherent, and illegible. |
| Time | Call an ambulance if you see any of the signs above. | It is important not to waste time and seek help as quickly as possible. |
Rehabilitation period
During the rehabilitation period, a whole range of measures is carried out, both medical and pedagogical, legal, social and psychological. All of them are aimed at restoring lost functions as a result of a lacunar stroke.
Principles of the rehabilitation program:
- If rehabilitation measures are started as early as possible, for example, from the first days of the onset of symptoms of the disease, recovery occurs much faster and more fruitfully. This is an excellent chance to avoid possible secondary complications, such as contractures, congestive pneumonia, thrombophlebitis and others.
- Rehabilitation should be carried out only under the supervision of specialists. If events are organized incorrectly, the chance of full recovery will be significantly less.
- Recovery requires the participation of a physical therapy methodologist, a neurologist, a physiotherapist, a psychotherapist, an occupational therapist and a speech therapist.
- The rehabilitation process involves the presence and support of the patient’s loved ones. It is best to entrust the patient with the most basic household chores on weekends or in the afternoon.
Rehabilitation after stroke
The consequences of lacunar stroke include both motor and psychological disorders, so the rehabilitation of such patients must be comprehensive. It needs to start as early as possible and be carried out under the supervision of a specialist.
Motor rehabilitation is aimed at eliminating negative consequences from the musculoskeletal system. Its goal is to restore full range of motion. For this use:
- special physical exercises;
- electrical stimulation of the neuromuscular system;
- passive gymnastics;
- training on simulators.
The prognosis for early initiation of motor rehabilitation is positive. In most patients, the amount of motor activity in the affected limb increases.
Speech impairment is a common consequence of lacunar stroke. For the rehabilitation of such patients:
- conduct classes with a speech therapist;
- communicate with family.
The absence of speech isolation is the most important factor for positive rehabilitation. It significantly improves the prognosis and increases the likelihood of restoration of speech understanding and production.
Social rehabilitation is achieved by creating a favorable microclimate in the family, gradually involving the patient in household chores, and interesting hobbies.
Treatment of lacunar stroke
Patients with lacunar infarctions are treated in neurological departments. They are necessarily prescribed antihypertensive therapy, drugs to restore nervous tissue, and prevention of thrombosis and embolism.
Antihypertensive therapy includes the prescription of ACE inhibitors (enalapril, lisinopril), diuretics (indapamide, furosemide), vasodilators (nifedipine, diltiazem), etc.
Patients with lacunar stroke need constant monitoring of blood pressure levels, but it is important that it does not become too low
In cases of severe atherosclerotic damage to the carotid and vertebral arteries, as well as in patients over 75 years of age, the pressure should not be quickly reduced, as this can cause even greater disruption of blood flow in the brain.
Antithrombotic therapy is considered an important stage in the treatment of cerebral infarctions. Patients are shown aspirin, heparin, clopidogrel. With the cardioembolic mechanism of stroke, when the cause is blockage of the perforating arteries by fragments of blood clots or deposits on the heart valves, anticoagulants (heparin, warfarin) are necessarily prescribed.
To prevent subsequent lacunar strokes, which tend to recur, aspirin up to 325 mg is prescribed. If the patient does not tolerate aspirin well, then its dosage is reduced to 50 mg per day and treatment is supplemented with dipyridamole at a daily dose of 400 mg in two doses.
Aspirin is indicated in the presence of microangiopathy, a combination of brain pathology with cardiovascular lesions. With concomitant lipid metabolism disorders, diet and lipid-lowering drugs (statins) are prescribed.
To improve microcirculation in the brain tissue, nicergoline, vinpocetine, and nootropil are used. It is advisable to prescribe neuroprotectors (akatinol, magnesium sulfate), B vitamins. If depression develops, antidepressants (fluoxetine, amitriptyline) are indicated.
In addition to drug therapy, patients undergo rehabilitation courses to restore motor function, sensitivity, speech, etc. Massage, physiotherapy, special exercises for paresis, and speech training help. You can restore memory and intellectual abilities by solving problems, memorizing poems or short texts.
Patients with cardiovascular pathology predisposing to thrombosis and embolic complications are observed by a cardiologist, who always prescribes aspirin and, if necessary, anticoagulants. If atherosclerosis of the carotid and vertebral arteries is diagnosed, then surgery may be needed to improve blood flow.
After suffering a lacunar stroke, patients are prescribed maintenance therapy with neuroprotectors, vitamins, and vascular medications, which are prescribed in courses 1-2 times a year.
The prognosis after a lacunar infarction is considered favorable, since the resulting neurological disorders regress quite quickly, and a complete restoration of impaired functions is possible
At the same time, this pathology should be given due attention by a neurologist, since repeated heart attacks occur in at least every tenth patient, and in a third, after a few years, signs of vascular encephalopathy with intellectual deficit and mental disorders increase
According to some data, after 10 years only 30% of patients remain alive, most of whom have severe signs of dementia. To avoid such developments, you need to strictly follow the doctor’s recommendations and take measures to prevent circulatory disorders in the brain.
2012-2020 sosudinfo.ru
Display all posts with the tag:
Stroke
Go to section:
Diseases of the brain and blood vessels of the head, cerebrovascular diagnostics, anatomy, pharmacology
Recommendations to SosudInfo readers are given by professional doctors with higher education and specialized work experience.
One of the leading authors of the site will answer your question in the form below.
Causes of stroke
Factors that influence the development of ischemic stroke, increase the likelihood of the disease occurring, experts divide into two groups: those that can be influenced and, thanks to proper treatment, prevent a stroke, and those that cannot be influenced, but with proper prevention the risks can be reduced.
The first group (cannot be influenced) includes the following symptoms:
- floor;
- age;
- genetics - first-degree relatives who had a stroke.
The second group (can be influenced) includes:
- arterial hypertension (high blood pressure);
- diabetes;
- TIA and/or previous stroke;
- obesity;
- cardiac ischemia;
- lipid metabolism disorder;
- carotid artery stenosis;
- heart rhythm disturbance - atrial fibrillation;
- heart failure;
- smoking;
- alcohol abuse;
- use of certain medications;
- severe stress.
Having these diseases and habits, it is necessary to consult a specialist to prevent a stroke and reduce the risks of it happening.
Treatment tactics
For adequate therapy and in the future for the purpose of preventing recurrent cerebrovascular accidents, patients are prescribed aspirin to reduce the aggregation of blood elements (sticking together and forming blood clots) and improve its fluidity. The most acceptable dose is considered to be 75 mg of acetylsalicylic acid, produced specifically for these purposes.
If it is impossible to take aspirin due to intolerance or side effects, it is possible to replace it with dipyridamole at a dose of 200 mg daily or 75 mg of clopidogrel. Dosages are specified and regulated by specialized specialists.
Normalization of blood circulation is achieved by prescribing drugs that improve microcirculation. The optimal choice is nicergoline, vinpocetine, pentoxifylline. First, a course of intravenous drips is carried out, followed by a transition to long-term use of tablet forms.
At the same time, neurotrophics are recommended - medications that optimize the supply of oxygen to the brain and stimulate recovery. These are Cerebrolysin, Actovegin, citicoline and ginkgo biloba preparations (memantine, tanakan, bilobil).
With the development of signs of dementia and the formation of a lacunar state, anticholinesterase drugs and precursors of acetylcholine, a biologically active substance involved in the conduction of impulses along nerve trunks, are prescribed. These are prozerin, neuromidin, galantamine in the required dosages.
With parkinsonism, the patient needs to take specific drugs to reduce tremors (cyclodol, amantadine).
To restore mental abilities and reduce the manifestations of dementia, it is necessary to use the patient’s intelligence as much as possible, forcing him to memorize poems, allowing him to solve simple mathematical problems.
Since the leading cause is hypertension, its adequate reduction can be considered as one of the links in the treatment process. The therapist and cardiologist select an adequate dose and combination of drugs. When prescribing a correction regimen, the patient’s age and the presence of significant concomitant diseases are taken into account: diabetes mellitus, chronic kidney disease.
Features of the development of lacunar stroke
Lacunar stroke is a type of ischemic brain injury that occurs in people suffering from arterial hypertension and related vascular changes. Elderly people are the main risk group. This type of stroke is characterized by pathological changes in small-caliber perforating arteries. A characteristic feature of a lacunar stroke is the formation of lacunae, that is, small cavities, in the depths of the brain.
Lacunae are round or irregular in shape and range from 1 to 20 mm in diameter, although formations larger than 15 mm are rare and are considered gigantic. Inside these cavities there is blood or plasma with fibrin. Their walls look like a bag, which can rupture when exposed to certain factors. Foci of necrosis are located deep in the gray matter; damage to the cerebral cortex does not occur even in the event of minor bleeding. A person can live with small gaps in the brain without even realizing it until histological analysis is carried out. All people associate stroke with severe neurological disorders, leading to paralysis and disruption of the patient’s usual life activities.
But there are types of pathology during which external symptoms do not appear, brain disorders are weak and characterized by regression. The person continues to live his usual life, unaware of the changes that have occurred. These types include lacunar ischemic stroke, which is called silent.
Features of the pathology
Lacunar ischemic stroke was described in 1965 as a symptom of hypertensive encephalopathy.
With the development of this type of pathology, patients do not suffer from the cerebral cortex. Cavities are localized
- in the white matter, large ganglia, internal capsule and optic canal;
- in the cerebellum and varus ponsi.
Unlike other types of stroke, when the lacunar form develops, disturbances occur not in the main artery, but in capillaries, the size of which is only a few tens of microns. They are located inside the brain and their task is to ensure blood flow in this organ.
The following elements are characteristic of changes in perforated arteries:
- If they are damaged, it is almost impossible to replace them with support ships;
- local lesions, no more than 2 cm in size;
- microaneurysms may develop, causing bleeding;
- There are no cholesterol plaques in these vessels.
Danger and consequences
When a patient is diagnosed with a single case of lacunar stroke, the prognosis for him is often favorable. In most cases, the victim completely recovers impaired brain functions, and only some patients may still experience partial impairments of sensitivity or motor function.
If a stroke relapse occurs, then certain negative consequences are possible, for example, a lacunar state of the brain (not uncommon in people with vascular dementia). In addition, the formation of lacunae in the area of the brain stem is especially dangerous, since this is where the respiratory and cardiovascular centers are localized.
If we talk about life prognosis, then the mortality rate as a result of lacunar stroke is only 2%, but this percentage increases with a second attack. However, it is quite difficult to say anything about life expectancy in this case. Much depends on the age of the person, the location of the pathological foci, the severity of concomitant ailments, as well as the timeliness of the assistance provided.
First aid for stroke
In the case of a stroke, the most important thing is to get the person to a specialized hospital as quickly as possible, preferably within the first hour after symptoms are noticed. It should be borne in mind that not all hospitals, but only a number of specialized centers are equipped to provide proper modern stroke care. Therefore, attempts to independently transport a patient to the nearest hospital during a stroke are often ineffective, and the first action is to call emergency services for medical transport.
Before the ambulance arrives, it is important not to allow the patient to eat or drink, since the swallowing organs may be paralyzed, and then food entering the respiratory tract can cause suffocation. At the first signs of vomiting, the patient's head is turned to the side so that the vomit does not enter the respiratory tract. It is better to lay the patient down with pillows under his head and shoulders, so that the neck and head form a single line, and this line makes an angle of about 30° to the horizontal. The patient should avoid sudden and intense movements. The patient is unbuttoned from tight, obstructive clothing, his tie is loosened, and his comfort is taken care of.
In case of loss of consciousness with absent or agonal breathing, cardiopulmonary resuscitation is started immediately. Its use greatly increases the patient's chances of survival. Determining the absence of a pulse is no longer a necessary condition for starting resuscitation; loss of consciousness and absence of rhythmic breathing are sufficient. The use of portable defibrillators further increases survivability: when in a public place (cafe, airport, etc.), first aid providers need to ask the staff if they have a defibrillator or nearby.
Cerebral infarction (lacunar infarction)
One of the types of cerebral infarction (ischemic stroke) is lacunar infarction, which is a small (up to 15 mm in diameter) brain damage that occurs when local blood circulation and gas exchange are disrupted. The reasons for this situation are varied and not fully understood, but most often it is blockage of supply vessels as a result of changes in their walls (atherosclerosis, inflammation), emboli (blood clots, fat droplets, bacterial colonies, etc.). Most of them are found in the periventricular region, basal ganglia, and thalamus - the central, deep structures of the brain. Lacunar infarctions account for 20-30% of all strokes.
Lacunar infarction can occur at any age, but the likelihood of its occurrence increases with age and reaches its maximum after 85 years. More often, cerebral circulatory disorders occur in men. The most significant risk factors for the occurrence of lacunar cerebral infarctions are:
- hypertonic disease,
- diabetes,
- chronic renal failure,
- post-infarction cardiosclerosis,
- abnormalities in the circulatory system and heart defects,
- rheumatism,
- cardiac arrhythmias,
- disorders of the blood coagulation system, blood diseases.
Clinical picture
Clinical symptoms of cerebral infarction may be insignificant or distinct, but short-lived. This depends on the location of the lesion in the central nervous system. More often it is represented by mono- or hemiparesis, disorders of statics and coordination of movements, syndrome of speech disorders and memory. General cerebral symptoms (lethargy, lethargy, confusion, headache, nausea and vomiting) are usually absent.
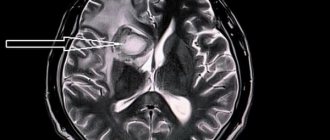
Magnetic resonance imaging (MRI) is the most preferred method in determining the location, and most importantly, in assessing the stage of development of the ischemic process. In the acute phase, the most information is carried by diffusion-weighted images (abbreviated as DWI) - images obtained using a specialized pulse sequence provided in expert-class MRI scanners, which we use in the study of all patients without exception.
Using DWI, you can see a minimal change in the diffusion (speed of movement) of fluid in brain tissue at the molecular level, which is the first sign of ischemic brain damage. In addition, when examining the brain of a patient with suspected lacunar infarction (as in all other cases), we use the entire set of pulse sequences that comply with the international standard to identify possible associated changes.
The patient is 32 years old. After visiting a neurologist, she went to the MRI room to rule out systemic damage to the central nervous system with a preliminary diagnosis of transient ischemic attack.
When scanning the brain in several modes, a lacunar infarction with a diameter of 7 mm was discovered in the cortical parts of the left parietal lobe. An acute infarction is clearly visible on DWI (a pulse sequence available in expert-class tomographs), but is poorly visible in a mode with signal suppression from free fluid.
A correct and timely diagnosis, including taking into account cause-and-effect relationships in the development of the pathological process, which is significantly facilitated by the MRI examination method described above, will predetermine the tactics of treatment measures.
After treatment, the patient's condition improved. On MRI after 3 months, positive dynamics are noticeable.
Detection of such changes is possible only with high-field magnetic tomographs of 1.5 T or 3 T, and also requires sufficient research time.
The multidisciplinary CELT clinic has a Philips Achieva 1.5T high-field tomograph, and we have an individual approach to each patient.
Registration for an MRI examination is carried out by specialists, and the examination lasts as long as necessary.
To sign up for the study, as well as find out more information about MRI, please call: 8 (495) 304-304-9.
What is a transient ischemic attack (TIA)
Transient ischemic stroke or transient ischemic attack (TIA) is a short-term disruption of brain function when blood circulation stops in one area, and is restored after a few hours. Local ischemia lasts no more than 24 hours, then it is reversible.
The main difference between TIA and ischemic stroke is that the first disease does not cause any changes in the brain. Scientists are currently examining the brain to determine whether TIA actually causes permanent changes to the brain.
New research tells a different story:
- TIA up to 5 minutes - no changes in the brain;
- TIA from 6 to 30 minutes - changes in the brain in every third person;
- TIA from 12 to 24 hours - changes in the brain of ⅔ patients.
It is important to understand that a transient ischemic attack is a precursor to a stroke, so you need to track it, see the subtle symptoms and consult a doctor as soon as possible to prevent stroke. From 10% to 40% of TIAs end in stroke, the risk is greatest in the first week after a transient ischemic attack.
At first glance, the symptoms of a TIA are indistinguishable from a stroke:
- darkening of the eyes;
- decreased vision;
- loss of vision in one eye;
- other visual impairments;
- speech disturbance, as if “porridge in the mouth”;
- inability to pronounce a word;
- inability to formulate words and sentences in your head;
- sensory disturbance;
- movement disorders;
- weakness in the body;
- numbness of the face;
- numbness of the upper and lower extremities;
- dizziness;
- falling without loss of consciousness;
- disorientation in time and space;
- memory impairment for recent events;
- loss of balance.
Clinical picture
In most cases, the attack can be sudden, very quickly leading to blockage of the arteries, but it can last up to five days. Precursors may include ischemic attacks that cause disruption of cerebral circulation in small cerebral arteries.
During an attack, you may experience high blood pressure and an irregular heart rhythm. Single cysts - lacunae do not lead to paralysis of the body. Detection of the lacunar form of cerebral infarction is complicated by the implicit manifestation of symptoms:
- Impaired motor skills are expressed in the inability to move the limbs; they become less sensitive.
- Loss of coordination. The patient may complain that everything is floating before his eyes, there is an unsteady gait and disorientation.
- The lacunar form of the disease is characterized by neurological disorders, expressed in the deterioration of memory, the ability to analyze, there is no logic of reasoning, and other processes of the brain are disrupted.
To immediately contact a doctor, one of the following symptoms of a stroke is sufficient:
- A sharp manifestation of weakness in the legs, fainting, loss of consciousness;
- Distortion of the face, numbness of half the body, limbs, impaired skin sensitivity;
- Difficulty in speech and impairment of its perception;
- The patient begins to feel dizzy and finds it difficult to maintain coordination of movements;
- Severe pain in the head appears;
- Cramps, increased muscle tone.
The disease can occur in the form of a micro-stroke or without clinical manifestations at all. It can develop at any age. Cases of the disease have been described in patients who have just turned 25 years old.
Features of the pathology:
- stroke develops only against the background of hypertension;
- there are no headaches, dizziness, nausea, vomiting, stiff neck, loss of consciousness or disturbances thereof;
- neural symptoms increase gradually over 2-48 hours (usually the patient’s disturbances develop during night sleep, and in the morning he wakes up with symptoms of a stroke);
- the prognosis for this disease is favorable; after an attack, complete or partial restoration of brain function is observed;
- examination of cerebral vessels using contrast agents does not show any abnormalities; computed tomography and magnetic resonance imaging can reveal small foci of low density, but not always, especially if the infarction is small.
Doctors describe about 20 clinical syndromes that can be observed with the development of lacunar stroke. The following are most often diagnosed:
- The isolated motor variant is the most common and occurs in 60% of patients. Lacunae form within the capsule and pons. The patient develops paralysis of one half of the body, usually the limbs, sometimes the face. Plegia is observed on the side opposite to the lacuna. No further neurological symptoms develop.
- The isolated sensitive variant is observed in almost 20% of patients. The lacunae in this case are localized in the ventral thalamic nerve ganglion. Disturbances of all types of sensitivity develop: temperature, nociceptive, tactile, muscle-articular. Manifestations of the disease can involve the head, arms, legs and torso. Typically, after what period sensitivity is fully or partially restored.
- Atactic hemiplegia develops when pathological foci appear in the capsule and pons of the brain. Occurs in 12% of patients. The patient experiences muscle hypotonia in the arms or legs, pyramidal disorders, and impaired coordination of movement on the side of the injury.
- Dysarthria and clumsiness of the hands when moving are observed in 6% of patients; pathological foci form in the pons of the brain. The patient has a speech impairment; on the one hand, paralysis of the limbs and head may develop.
The following syndromes are also often diagnosed:
- dyskinesia;
- false bulbar syndrome;
- parkinsonism syndrome;
- forced gait in small steps;
- urgency to urinate, incontinence;
- hemiparesis and loss of sensation of one half of the body.
With the development of a lacunar stroke, there is no disorder of consciousness or vision, systemic impairment of formed speech (aphasia), or other symptoms of damage to the cerebral cortex.
Dementia
Dementia is a severe disorder of higher nervous activity caused by organic damage to the brain, and is manifested, first of all, by a sharp decrease in mental abilities (hence the name - dementia translated from Latin means feeble-mindedness). The clinical picture of dementia depends on the cause that caused organic brain damage, on the localization and extent of the defect, as well as on the initial state of the body. However, all cases of dementia are characterized by pronounced stable disorders of higher intellectual activity (memory deterioration, decreased ability to abstract thinking, creativity and learning), as well as more or less pronounced disturbances of the emotional-volitional sphere, from the accentuation of character traits (the so-called “caricature”) until the complete collapse of personality. Causes and types of dementia
Since the morphological basis of dementia is severe organic damage to the central nervous system, the cause of this pathology can be any disease that can cause degeneration and death of cells in the cerebral cortex. First of all, it is necessary to highlight specific types of dementia in which destruction of the cerebral cortex is an independent and leading pathogenetic mechanism of the disease:
· Alzheimer's disease;
Dementia with Lewy bodies;
· Pick's disease, etc.
In other cases, damage to the central nervous system is secondary and is a complication of the underlying disease (chronic vascular pathology, infection, trauma, intoxication, systemic damage to nervous tissue, etc.). The most common cause of secondary organic brain damage is vascular disorders, in particular cerebral atherosclerosis and hypertension. Common causes of dementia also include alcoholism, tumors of the central nervous system, and traumatic brain injury. Less commonly, the cause of dementia is infections - AIDS, viral encephalitis, neurosyphilis, chronic meningitis, etc. In addition, dementia can develop:
as a complication of hemodialysis;
· as a complication of severe renal and liver failure;
· for some endocrine pathologies (thyroid disease, Cushing's syndrome, pathology of the parathyroid glands);
· for severe autoimmune diseases (systemic lupus erythematosus, multiple sclerosis).
In some cases, dementia develops from multiple causes. A classic example of such a pathology is senile (senile) mixed dementia. Functional and anatomical types of dementia
Depending on the predominant localization of the organic defect, which has become the morphological substrate of the pathology, four types of dementia are distinguished: 1. Cortical dementia - predominant damage to the cerebral cortex. This type is most typical for Alzheimer's disease, alcoholic dementia, and Pick's disease. 2. Subcortical dementia. With this type of pathology, the subcortical structures are primarily affected, which causes neurological symptoms. A typical example is Parkinson's disease with predominant damage to the neurons of the substantia nigra of the midbrain, and specific motor disorders: tremor, general muscle stiffness (“doll gait”, mask-like face, etc.). 3. Cortical-subcortical dementia is a mixed type of lesion, characteristic of pathology caused by vascular disorders. 4. Multifocal dementia is a pathology characterized by multiple lesions in all parts of the central nervous system. Steadily progressing dementia is accompanied by severe and varied neurological symptoms. Forms of dementia
Clinically, lacunar and total forms of dementia are distinguished. Lacunarnaya
Lacunar dementia is characterized by peculiar isolated lesions of the structures responsible for intellectual activity. In this case, as a rule, short-term memory suffers the most, so patients are forced to constantly take notes on paper. Based on its most pronounced symptom, this form of dementia is often called dysmnestic dementia (dysmensia literally means memory impairment). However, a critical attitude towards one’s condition remains, and the emotional-volitional sphere suffers slightly (most often only asthenic symptoms are expressed - emotional lability, tearfulness, increased sensitivity). A typical example of lacunar dementia is the initial stages of the most common form of dementia, Alzheimer's disease. Total
Total dementia is characterized by complete disintegration of the core of personality. In addition to pronounced violations of the intellectual-cognitive sphere, gross changes in emotional-volitional activity are observed - a complete devaluation of all spiritual values occurs, as a result of which vital interests become impoverished, the sense of duty and modesty disappears, and complete social disadaptation occurs. The morphological substrate of total dementia is damage to the frontal lobes of the cerebral cortex, which often occurs with vascular disorders, atrophic (Pick's disease) and volumetric processes of the corresponding localization (tumors, hematomas, abscesses). Basic classification of presenile and senile dementias
The likelihood of developing dementia increases with age. So if in adulthood the proportion of patients with dementia is less than 1%, then in the age group after 80 years it reaches 20%. Therefore, the classification of dementias that occur at a late age is especially important. There are three types of dementia that are most common in presenile and senile (presenile and senile) ages: 1. Alzheimer's (atrophic) type of dementia, which is based on primary degenerative processes in nerve cells. 2. Vascular type of dementia, in which degeneration of the central nervous system develops secondarily, as a result of severe circulatory disorders in the vessels of the brain. 3. Mixed type, which is characterized by both mechanisms of disease development. Clinical course and prognosis
The clinical course and prognosis of dementia depend on the cause that caused the organic defect of the central nervous system. In cases where the underlying pathology is not prone to development (for example, with post-traumatic dementia), with adequate treatment, significant improvement is possible due to the development of compensatory reactions (other areas of the cerebral cortex take on part of the functions of the affected area). However, the most common types of dementia - Alzheimer's disease and vascular dementia - have a tendency to progress, therefore, when they talk about treatment, for these diseases we are only talking about slowing down the process, social and personal adaptation of the patient, prolonging his life, relieving unpleasant symptoms, etc. .P. And finally, in cases where the disease that causes dementia progresses rapidly, the prognosis is extremely unfavorable: the patient’s death occurs several years or even months after the first signs of the disease appear. The cause of death, as a rule, is various concomitant diseases (pneumonia, sepsis), developing against the background of disturbances in the central regulation of all organs and systems of the body. Severity (stage) of dementia
In accordance with the patient’s social adaptation capabilities, three degrees of dementia are distinguished. In cases where the disease that causes dementia has a steadily progressive course, we often speak of the stage of dementia. Mild degree
With mild dementia, despite significant impairments in the intellectual sphere, the patient remains critical of his own condition. So the patient can easily live independently, performing familiar household activities (cleaning, cooking, etc.). Moderate degree
With moderate dementia, there are more severe intellectual impairments and a reduced critical perception of the disease. At the same time, patients experience difficulties in using ordinary household appliances (stove, washing machine, TV), as well as telephones, door locks and latches, so in no case should the patient be completely left to his own devices. Severe dementia
In severe dementia, a complete breakdown of the personality occurs. Such patients often cannot eat on their own, observe basic hygiene rules, etc. Therefore, in the case of severe dementia, hourly monitoring of the patient is necessary (at home or in a specialized institution). Diagnostics
To date, clear criteria for diagnosing dementia have been developed: 1. Signs of memory impairment - both long-term and short-term (subjective data from a survey of the patient and his relatives are supplemented by objective research). 2. The presence of at least one of the following disorders characteristic of organic dementia:
vsigns of decreased ability for abstract thinking (according to objective research);
vsymptoms of decreased criticality of perception (discovered when making real plans for the next period of life in relation to oneself and others);
v syndrome three "A":
· aphasia – various kinds of disorders of already formed speech;
· apraxia (literally “inactivity”) – difficulties in performing purposeful actions while maintaining the ability to move;
· agnosia – various disturbances of perception while maintaining consciousness and sensitivity.
For example, the patient hears sounds, but does not understand the speech addressed to him (auditory-verbal agnosia), or ignores a part of the body (does not wash or put on one foot - somatoagnosia), or does not recognize certain objects or faces of people with intact vision (visual agnosia). and so on.;
vpersonal changes (rudeness, irritability, disappearance of shame, sense of duty, unmotivated attacks of aggression, etc.).
3. Violation of social interactions in the family and at work.
4. Absence of manifestations of delirious changes in consciousness at the time of diagnosis (there are no signs of hallucinations, the patient is oriented in time, space and his own personality, as far as his condition allows).
5. A certain organic defect (results of special studies in the patient’s medical history).
- It should be noted that in order to make a reliable diagnosis of dementia, it is necessary that all of the above symptoms be observed for at least 6 months. Otherwise, we can only talk about a presumptive diagnosis. Alzheimer's type dementia
Dementia of the Alzheimer's type (Alzheimer's disease) received its name from the name of the doctor who first described the pathology clinic in a 56-year-old woman. The doctor was alerted by the early manifestation of signs of senile dementia. A post-mortem examination showed peculiar degenerative changes in the cells of the patient’s cerebral cortex. Subsequently, this kind of violation was discovered in cases where the disease manifested itself much later. This was a revolution in views on the nature of senile dementia - previously it was believed that senile dementia was a consequence of atherosclerotic damage to the blood vessels of the brain. Dementia of the Alzheimer's type is the most common type of senile dementia today, and, according to various sources, accounts for 35 to 60% of all cases of organic dementia. Risk factors for developing the disease
There are the following risk factors for developing dementia of the Alzheimer's type (arranged in descending order of importance):
· age (the most dangerous limit is 80 years);
· the presence of relatives suffering from Alzheimer's disease (the risk increases many times if the relatives develop the pathology before the age of 65);
· hypertonic disease;
· atherosclerosis;
· increased levels of lipids in the blood plasma;
· diabetes;
· obesity;
· sedentary lifestyle;
· diseases occurring with chronic hypoxia (respiratory failure, severe anemia, etc.);
· traumatic brain injuries;
· low level of education;
· lack of active intellectual activity throughout life;
· female.
First signs
It should be noted that degenerative processes in Alzheimer's disease begin years and even decades before the first clinical manifestations. The first signs of Alzheimer's type dementia are very characteristic: patients begin to notice a sharp decline in memory for recent events. At the same time, a critical perception of their condition persists for a long time, so that patients often feel understandable anxiety and confusion, and consult a doctor. Memory impairment in dementia of the Alzheimer's type is characterized by the so-called Ribot's law: first short-term memory is impaired, then recent events are gradually erased from memory. Memories from distant times (childhood, adolescence) are retained the longest. Characteristics of the advanced stage of progressive dementia of the Alzheimer's type
At the advanced stage of dementia of the Alzheimer's type, memory impairment progresses, so that in some cases only the most significant events are remembered. Gaps in memory are often replaced by fictitious events (so-called confabulations - false memories). The criticality of perception of one's own state is gradually lost. At the advanced stage of progressive dementia, disorders of the emotional-volitional sphere begin to appear. The following disorders are most characteristic of senile dementia of the Alzheimer's type:
· egocentrism;
· grouchiness;
· suspicion;
· conflict.
These signs are called senile (senile) personality restructuring. In the future, against this background, delusions of harm, which are very specific to dementia of the Alzheimer’s type, may develop: the patient accuses relatives and neighbors of constantly robbing him, wishing for his death, etc. Other types of disturbances in normal behavior often develop:
· sexual incontinence;
· gluttony with a special penchant for sweets;
· craving for vagrancy;
· fussy, disorderly activity (walking from corner to corner, shifting things, etc.).
At the stage of severe dementia , the delusional system disintegrates, and behavioral disorders disappear due to extreme weakness of mental activity. Patients plunge into complete apathy and do not experience hunger or thirst. Movement disorders soon develop, so that patients cannot walk or chew food normally. Death occurs from complications due to complete immobility, or from concomitant diseases. Diagnosis of Alzheimer's type dementia
The diagnosis of dementia of the Alzheimer's type is made on the basis of the characteristic clinical picture of the disease, and is always probabilistic. Differential diagnosis between Alzheimer's disease and vascular dementia is quite difficult, so often a final diagnosis can only be made posthumously. Treatment
Treatment of Alzheimer's type dementia is aimed at stabilizing the process and reducing the severity of existing symptoms. It should be comprehensive and include therapy for diseases that aggravate dementia (hypertension, atherosclerosis, diabetes, obesity). Forecast
Dementia of the Alzheimer's type is a steadily progressive disease that inevitably leads to severe disability and death of the patient. The process of disease development, from the appearance of the first symptoms to the development of senile insanity, usually takes about 10 years. The earlier Alzheimer's disease develops, the faster dementia progresses. In patients under 65 years of age (senile dementia or presenile dementia), neurological disorders (apraxia, agnosia, aphasia) develop early. Vascular dementia
Dementia due to cerebral vascular lesions
Dementia of vascular origin ranks second in prevalence after dementia of the Alzheimer's type, and accounts for about 20% of all types of dementia. In this case, as a rule, dementia that develops after vascular accidents, such as: 1. Hemorrhagic stroke (vascular rupture), is considered separately. 2. Ischemic stroke (blockage of a vessel with cessation or deterioration of blood circulation in a certain area). In such cases, massive death of brain cells occurs, and the so-called focal symptoms, depending on the location of the affected area (spastic paralysis, aphasia, agnosia, apraxia, etc.), come to the fore. So the clinical picture of post-stroke dementia is very heterogeneous, and depends on the degree of damage to the vessel, the area of the brain supplied with blood, the compensatory capabilities of the body, as well as the timeliness and adequacy of medical care provided in case of a vascular accident. Dementias that occur with chronic circulatory failure develop, as a rule, in old age and demonstrate a more homogeneous clinical picture. What disease can cause vascular type dementia?
The most common causes of vascular type dementia are hypertension and atherosclerosis - common pathologies characterized by the development of chronic cerebrovascular insufficiency. The second large group of diseases leading to chronic hypoxia of brain cells is vascular damage in diabetes mellitus (diabetic angiopathy) and systemic vasculitis, as well as congenital disorders of the structure of cerebral vessels. Acute cerebral circulatory failure can develop due to thrombosis or embolism (blockage) of a vessel, which often occurs with atrial fibrillation, heart defects, and diseases with an increased tendency to thrombus formation. Risk factors
The most significant risk factors for the development of dementia of vascular origin:
· hypertension, or symptomatic arterial hypertension;
· increased levels of lipids in the blood plasma;
· systemic atherosclerosis;
· smoking;
· cardiac pathologies (coronary heart disease, arrhythmias, heart valve damage);
· sedentary lifestyle;
· overweight;
· diabetes;
· tendency to thrombosis;
Systemic vasculitis (vascular diseases).
Symptoms and course of senile vascular dementia
The first warning signs of vascular dementia are difficulty concentrating. Patients complain of fatigue and have difficulty concentrating for long periods of time. At the same time, it is difficult for them to switch from one type of activity to another. Another harbinger of developing vascular dementia is slowness of intellectual activity, so for the early diagnosis of cerebral circulatory disorders, tests for the speed of performing simple tasks are used. Early signs of developed dementia of vascular origin include violations of goal setting - patients complain of difficulties in organizing elementary activities (making plans, etc.). In addition, already in the early stages, patients experience difficulties in analyzing information: it is difficult for them to identify the main and secondary, to find the common and different between similar concepts. Unlike dementia of the Alzheimer's type, memory impairment in dementia of vascular origin is not as pronounced. They are associated with difficulties in reproducing perceived and accumulated information, so that the patient easily remembers “forgotten” when asking leading questions, or chooses the correct answer from several alternative ones. At the same time, memory for important events is retained for quite a long time. For vascular dementia, disturbances in the emotional sphere are specific in the form of a general decrease in mood, up to the development of depression, which occurs in 25-30% of patients, and pronounced emotional lability, so that patients can cry bitterly, and a minute later move on to quite sincere fun. Signs of vascular dementia include the presence of characteristic neurological symptoms, such as: 1. Pseudobulbar syndrome, which includes impaired articulation (dysarthria), changes in voice timbre (dysphonia), less often - impaired swallowing (dysphagia), violent laughter and crying. 2. Gait disturbances (shuffling, mincing gait, “skier’s gait”, etc.). 3. Decreased motor activity, so-called “vascular parkinsonism” (poor facial expressions and gestures, slowness of movements). Vascular dementia, which develops as a result of chronic circulatory failure, usually progresses gradually, so the prognosis largely depends on the cause of the disease (hypertension, systemic atherosclerosis, diabetes mellitus, etc.). Treatment
Treatment of vascular dementia is primarily aimed at improving cerebral circulation - and, consequently, at stabilizing the process that caused dementia (hypertension, atherosclerosis, diabetes, etc.). Senile dementia with Lewy bodies
Senile dementia with Lewy bodies is an atrophic-degenerative process with the accumulation of specific intracellular inclusions – Lewy bodies – in the cortex and subcortical structures of the brain. The causes and mechanisms of development of senile dementia with Lewy bodies are not fully understood. Just as with Alzheimer's disease, the hereditary factor is of great importance. According to theoretical data, senile dementia with Lewy bodies ranks second in prevalence, and accounts for about 15-20% of all senile dementias. However, during life such a diagnosis is made relatively rarely. Typically, such patients are misdiagnosed as having vascular dementia or Parkinson's disease with dementia. The fact is that many symptoms of dementia with Lewy bodies are similar to the listed diseases. Just as with the vascular form, the first symptoms of this pathology are a decrease in the ability to concentrate, slowness and weakness of intellectual activity. Subsequently, depression, decreased motor activity similar to parkinsonism, and walking disorders develop. At the advanced stage, the clinical picture of dementia with Lewy bodies is in many ways reminiscent of Alzheimer's disease, since delusions of damage, delusions of persecution, and delusions of doubles develop. As the disease progresses, delusional symptoms disappear due to complete exhaustion of mental activity. However, senile dementia with Lewy bodies has some specific symptoms. It is characterized by so-called small and large fluctuations - sharp, partially reversible disturbances in intellectual activity. With small fluctuations, patients complain of temporary impairments in the ability to concentrate and perform some task. With large fluctuations, patients note impaired recognition of objects, people, terrain, etc. Often the disorders reach the point of complete spatial disorientation and even confusion. Another characteristic feature of dementia with Lewy bodies is the presence of visual illusions and hallucinations. Illusions are associated with a violation of orientation in space and intensify at night, when patients often mistake inanimate objects for people. A specific feature of visual hallucinations in dementia with Lewy bodies is their disappearance when the patient tries to interact with them. Visual hallucinations are often accompanied by auditory hallucinations (speaking hallucinations), but auditory hallucinations do not occur in their pure form. As a rule, visual hallucinations are accompanied by large fluctuations. Such attacks are often provoked by a general deterioration in the patient’s condition (infectious diseases, fatigue, etc.). When recovering from a large fluctuation, patients partially amnesize what happened, intellectual activity is partially restored, however, as a rule, the state of mental functions becomes worse than the original one. Another characteristic symptom of dementia with Lewy bodies is sleep behavior disorder: patients can make sudden movements, and even injure themselves or others. In addition, with this disease, as a rule, a complex of autonomic disorders develops:
Orthostatic hypotension (a sharp decrease in blood pressure when moving from a horizontal to a vertical position);
· fainting;
· arrhythmias;
· disruption of the digestive tract with a tendency to constipation;
· urinary retention, etc.
Treatment for senile dementia with Lewy bodies is similar to treatment for dementia of the Alzheimer's type. The course of dementia with Lewy bodies is rapidly and steadily progressive, so the prognosis is much more serious than for other types of senile dementia. The period from the appearance of the first signs of dementia to the development of complete insanity usually takes no more than four to five years. Alcoholic dementia
Alcohol-induced dementia develops as a result of long-term (15-20 years or more) toxic effects of alcohol on the brain. In addition to the direct influence of alcohol, indirect effects (endotoxin poisoning due to alcoholic liver damage, vascular disorders, etc.) take part in the development of organic pathology. Almost all alcoholics at the stage of development of alcoholic personality degradation (the third and final stage of alcoholism) exhibit atrophic changes in the brain (expansion of the cerebral ventricles and sulci of the cerebral cortex). Clinically, alcoholic dementia is a diffuse decrease in intellectual abilities (memory deterioration, concentration, ability for abstract thinking, etc.) against the background of personal degradation (coarsening of the emotional sphere, destruction of social connections, primitivism of thinking, complete loss of value orientations). At this stage of development of alcohol dependence, it is very difficult to find incentives to encourage the patient to treat the underlying disease. However, in cases where it is possible to achieve complete abstinence for 6-12 months, the signs of alcoholic dementia begin to regress. Moreover, instrumental studies also show some smoothing of the organic defect. Epileptic dementia
The development of epileptic (concentric) dementia is associated with a severe course of the underlying disease (frequent seizures with transition to status epilepticus). Indirect factors may be involved in the genesis of epileptic dementia (long-term use of antiepileptic drugs, injuries from falls during seizures, hypoxic damage to neurons during status epilepticus, etc.). Epileptic dementia is characterized by slowness of thought processes, the so-called viscosity of thinking (the patient cannot distinguish the main from the secondary, and gets fixated on describing unnecessary details), decreased memory, and impoverished vocabulary. A decrease in intellectual abilities occurs against the background of a specific change in personality traits. Such patients are characterized by extreme selfishness, malice, vindictiveness, hypocrisy, quarrelsomeness, suspiciousness, accuracy, even pedantry. The course of epileptic dementia is steadily progressive. With severe dementia, malice disappears, but hypocrisy and servility remain, and lethargy and indifference to the environment increases.
https://www.tiensmed.ru