Against the background of coronavirus infection, blood oxygen saturation may drop sharply, and serious health problems will begin. In case of lack of oxygen, doctors often talk about hypoxemia. What is it?
Hypoxemia is a word derived from the ancient Greek “hypo” (a prefix denoting weakness) and the New Latin oxygenium - oxygen. In fact, this term, experts note, hides a decrease in the oxygen content in human blood. The causes of this condition can be various options - from circulatory disorders to a decrease in hemoglobin. With hypoxemia, pressure often decreases, and saturation also drops below normal values.
Why is it developing?
Doctors identify several main reasons for the development of hypoxemia, as well as a number of provoking conditions. Among the causes of lack of oxygen in the blood are:
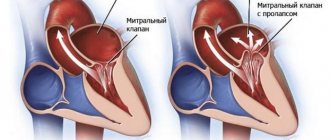
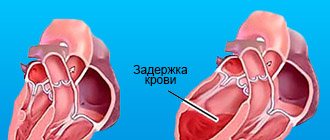
- Atypical blood shunting - this situation can occur against the background of heart defects, when venous blood begins to flow into the aorta - in this case, hemoglobin loses its ability to attach oxygen.
- Problems with insufficient ventilation in the lungs - this happens when the frequency of exhalations and inhalations slows down, as a result of which, naturally, the supply of oxygen to the body decreases. Here they usually talk about a whole list of problems, including chest injuries, obstruction in the bronchi, inflammatory processes, such as pneumonia, collapse of part of the lung, etc.
- Anemia - when the level of hemoglobin decreases, the level of oxygen transported to the tissues begins to decrease.
- Diffusion disorders - due to increased physical activity, blood circulation begins to accelerate, as a result of which the amount of time required for hemoglobin to contact with oxygen decreases.
Also, a lack of oxygen in the blood can develop against the background of such a bad habit as smoking, with lung diseases, overweight and obesity, with changes in atmospheric pressure and with a decrease in the concentration of oxygen in the air.
How to measure blood oxygen levels at home? More details
RESPIRATORY FAILURE AND ARTERIAL HYPOXEMIA
The main function of the external respiration system is to absorb oxygen from the external environment and remove carbon dioxide from the internal environment.
Respiratory failure is a condition of the body due to the inability of the external respiratory system to provide:
« absorption by the lungs O? and the level of its tension in arterial blood (PaOj), sufficient to saturate hemoglobin with oxygen adequate to the body’s needs;
» removal of carbon dioxide from the body, allowing the body to maintain the concentration of protons in the extracellular fluid and blood plasma ([H+]) in the range of normal changes. In addition, respiratory failure should be understood as the inability of the external respiratory system to respond by increasing the absorption of oxygen by the lungs and excreting carbon dioxide in response to an increase in the body's need for oxygen (an increase in the body's consumption of O2 and to an increased need for the excretion of carbon dioxide (increased release of carbon dioxide in during metabolism into the internal environment of the body).
A decrease in oxygen tension in arterial blood and an increase in carbon dioxide tension (PaCO2) in it may be a consequence of an increase in oxygen consumption by the body (PO) and the formation of carbon dioxide in it during physical activity, fever, sepsis, and during nonspecific compensatory processes (“stress reaction” ), with thyrotoxicosis, as well as with other pathological conditions and adaptive reactions. Moreover, during certain periods of illness and pathological process, gas tensions in the blood, as the body’s utilization of free energy decreases, return to “normal” limits. This does not mean that respiratory failure is eliminated by therapy. It remains hidden and manifests itself as arterial hypoxemia and hypercapnia with subsequent increases in oxygen consumption and carbon dioxide formation during the course of the disease.
Pulmonary gas exchange occurs at the level of the terminal respiratory units (TRE) of the lungs. TPE (respiron) is a part of the lungs distal to the terminal non-respiratory bronchiole, which is washed by mixed venous blood entering through a branch of the pulmonary artery (pulmonary arteriole) parallel to this terminal non-respiratory bronchiole.
The pulmonary arteriole splits into a capillary network that envelops the alveoli and forms pulmonary venules located at the periphery of the TPE. This structure of TPE structurally ensures the movement of mixed venous blood strictly from arterioles through the pulmonary capillaries into the venules and its oxygenation at the level of the alveoli.
For the most complete oxygenation of mixed venous blood at the level of one respirator and its release from carbon dioxide (pulmonary gas exchange), the presence and coincidence in time of two conditions is necessary:
1. Sufficient supply of oxygen from the external environment to the composition of the alveolar gas mixture, that is, a certain level of minute alveolar ventilation (MAV) with a respiratory mixture of gases with a sufficient oxygen content in it. In addition, sufficient MAV is a necessary condition for adequate excretion of carbon dioxide during external respiration from mixed venous blood and alveolar gas mixture into the external environment.
2. Optimal supply of mixed venous blood to Respiron. If at the level of one respiron MAV begins to predominate over
blood flow, that is, it becomes excessive, then pathogenic changes in the tension of oxygen and carbon dioxide in the blood contained in the venules of a given respirator will not occur. However, an increase in the MAV of some respirators, one set of structural and functional units of the lungs, leads to a decrease in the ventilation of others, and therefore to a disruption of pulmonary gas exchange in them. The cause of disturbances in gas exchange in the lungs may also be the predominance of the supply of mixed venous blood to some respirators at the expense of others.
Respiratory failure is always a consequence of violations of the compliance of the MAV of the structural and functional units of the lungs, their departments and parts, of all lungs with the volumetric velocity of blood flow, that is, disorders of ventilation-perfusion relations.
Under physiological conditions, there is always normal variability in the ventilation-perfusion ratios of respiratory organs and parts of the lungs, which does not lead to respiratory failure at the level of all lungs. In respiratory failure, physiological variability transforms into pathological variability. As a result, pulmonary gas exchange is disrupted at the level of the entire external respiration system. Due to the greater diffusivity of carbon dioxide on
/
disruptions in pulmonary gas exchange often first lead to a pathogenic drop in oxygenation of mixed venous blood, that is, they cause arterial hypoxemia (Table 2.1).
Severity of arterial hypoxemia
Table 2.1
| Severity | Oxygen tension in arterial blood when breathing air not enriched with oxygen, mm Hg. Art. | Mandatory • therapeutic measures |
| Lightweight | 80-62 | |
| Moderate | 61-51 | Oxygen insufflation during spontaneous breathing of the patient and |
| O2 content in the inhaled gas mixture (FiO2) within 30-40% | ||
| Heavy | 50-40 | Artificial ventilation with FiO2 not less than 50% |
| Extremely heavy | <40 | Artificial ventilation of the lungs with pure oxygen |
Arterial hypoxemia
Arterial hypoxemia is understood as a pathologically low level of oxygenation of mixed venous blood, as a result of which the transport of oxygen from the lungs to the periphery becomes so low that respiratory hypoxia occurs.
Arterial hypoxemia most often results from:
» disturbances in the physiological variability of ventilation-perfusion ratios (VPR) of respirons and parts of the lungs;
» pathological intrapulmonary shunting of blood from right to left, that is, an increase in the volume of unoxygenated mixed venous blood that passes through the lungs into arterial blood without participating in pulmonary gas exchange;
“reducing the partial pressure of oxygen in the inhaled gas mixture;
“drop in oxygen tension in mixed venous blood (Pv02);
“impaired diffusion of gases through the alveolo-capillary membrane;
“low MAV, that is, hypoventilation.
The severity of arterial hypoxemia is assessed depending on the level of oxygen tension in the arterial blood (Table 2.1).
Pathological variability of ventilation-perfusion
relations and shunting of mixed venous blood in the lungs
as a cause of arterial hypoxemia
The total area of the pulmonary membrane through which diffusion of free oxygen and carbon dioxide molecules occurs varies from 160 to 200 m2 in healthy people. This area is the sum of the gas exchange surface (pulmonary membrane) of about 100,000 respirators (TRE) and several million alveoli. Mass transfer of oxygen and carbon dioxide from the alveolar gas mixture to mixed venous blood and in the opposite direction can be sufficient only if there is an unimpeded blood supply to a certain number of optimally ventilated respirators.
The total volume of blood contained in the pulmonary capillaries is 100 ml. This volume of blood “stretches” to the thinnest film on the surface of the pulmonary membrane within all the lungs, which, structurally and functionally, provides the most optimal conditions for normal pulmonary gas exchange. The criteria for compliance of pulmonary gas exchange with the needs of the body are the partial pressures and tensions of gases in the alveolar gas mixture, arterial and mixed venous blood (Table 2.2).
Table 2.2
Partial pressures (tensions) of oxygen and carbon dioxide in the alveolar gas mixture, mixed venous and arterial blood under conditions of relative rest in a healthy young man at sea level
| Partial pressures and | Alveoli | Mixed | Arterial |
| gas voltage | deoxygenated blood | blood | |
| P02 | |||
| PCO2 |
The ventilation-perfusion ratio (VPR) at the level of all lungs represents the average value of the VPR of their respirators, sections of lung tissue and sections of the lungs. A HPO of all lungs of a healthy person under conditions of relative rest equal to 0.8 may indicate physiological variability of HPO within the entire pulmonary parenchyma. With physiological variability of HPR , the gas exchange respiratory coefficient, the ratio of the release of carbon dioxide to oxygen consumption by the body (PO^ is equal to the metabolic respiratory coefficient, that is, the ratio of the formation of carbon dioxide during metabolism to PO^ and they are both at a level close to 0.8.
In the lungs of a healthy person there is no pathological variability in the ventilation-perfusion ratios of respirons, areas of the pulmonary parenchyma and sections of the lungs, despite the constant effect of a number of factors of physiological variability of HPO:
» greater stretching of the underlying and peripheral parts of the lungs at the height of inspiration, causing a preferential distribution of tidal volume to these parts of the lungs;
» exposure of the pulmonary blood flow to influences from the force of gravity, which lead to the predominance of blood supply to the underlying respirators;
“dependence of the volumetric velocity of pulmonary blood flow in different parts of the lungs on the tidal volume:
Then, when, as a result of a pathological process (pneumonia, hemopneumothorax, extreme stage of adult respiratory distress syndrome, pulmonary contusion, wound pulmonitis, etc.), lung respirators lose both alveoli and pulmonary microvessels to the same extent, pathological variability of pulmonary respirators may not develop. . In this case, arterial hypoxemia under conditions of relative rest does not occur until the lungs lose 70-80% of respirators.
If the flow of mixed venous blood into any respiratory system or part of the lungs is reduced or blocked, then the part of the tidal volume that reaches the alveoli increases, but does not participate in pulmonary gas exchange. This reduces oxygen uptake by the entire lungs, which causes a drop in arterial oxygen tension and arterial hypoxemia. When the increase in ventilation of part of the alveoli is not accompanied by an adequate increase in blood flow through the capillaries, then all lungs absorb less oxygen from the alveolar gas mixture. It also increases the fraction of tidal volume not used for pulmonary gas exchange and reduces oxygen uptake by the lungs. The result of both variants of pathological variability of respiron HPO can be arterial hypoxemia. If two described variants of HPE disorders occur simultaneously in the lungs, then at the level of the entire external respiration system this leads to a decrease in the physiological area of the pulmonary membrane. The physiological area of the pulmonary membrane is that part of it through which diffusion of oxygen and carbon dioxide leads to complete, that is, limited only by partial pressure (stress) gradients, absorption of oxygen from the alveolar gas mixture, oxygenation of mixed venous blood and its release from carbon dioxide.
A decrease in the physiological area of the pulmonary membrane to a certain level leads to arterial hypoxemia.
Stenosis, obstruction of the pulmonary artery or its branches, as well as multiple embolism of pulmonary microvessels (disseminated intravascular coagulation, fat embolism, thrombosis by microclots of transfused blood, aggregates of activated platelets and neutrophils in traumatic shock and sepsis) lead to the formation of alveolar dead spaces, that is alveoli ventilated, but not washed by mixed venous blood.
The result is a difference between PaCO2 and the partial pressure of carbon dioxide in the final part of the exhaled air, which is considered equivalent to the partial pressure of carbon dioxide in the alveolar gas mixture, PACO2. This is the result of a complete cessation in respirators with only dead alveolar spaces of the transfer of carbon dioxide across the pulmonary membrane. Mixed venous blood from such respirators rushes through collaterals into the pulmonary venules of other TPEs without releasing carbon dioxide into the alveolar gas mixture. As a result, shunting of mixed venous blood in the lungs increases, which causes:
“decrease in the difference between the carbon dioxide tension in mixed venous blood and PaCO2;
“increasing difference between PaCO2 and PACO2.
Initially for widespread microembolization syndrome in the lungs
compensatory hyperventilation in response to an increase in PaCO2 through an increase in carbon dioxide excretion prevents
hypercapnia, that is, pathologically high PaCO2.
If, as a result of obstruction of the pulmonary microvessels, the absorption of oxygen by the lungs decreases to such an extent that arterial hypoxemia occurs, then the decrease in the oxygen capacity of the blood and the decrease in PaO2 in it have a negative inotropic effect on the heart. A decrease in cardiac contractility can lead to a decrease in minute volume of blood circulation (MCV).
The drop in minute volume of blood circulation in this case occurs not only due to arterial hypoxemia. IOC decreases due to an increase in total pulmonary vascular resistance as a cause of right ventricular heart failure. Compensatory hyperventilation in response to arterial hypoxemia increases PO2, which accelerates the development of circulatory hypoxia. Circulatory hypoxia in the syndrome of widespread microembolization in the lungs is the result of pulmonary arterial hypertension, right ventricular heart failure and the associated drop in IOC with high oxygen demand of the whole body due to increased energy consumption in the external respiratory system.
The main symptoms of widespread microembolization syndrome in the lungs are shortness of breath and tachycardia, which occur and worsen even with a minimal increase in physical activity. If, during examination of such patients, no wheezing is heard over the lungs, X-ray examination does not reveal pathological changes in the lungs, and the anamnesis does not contain data indicating previous obvious or latent chronic heart failure, then widespread embolization of the pulmonary microvessels should be suspected. When, in addition, there are electrocardiographic signs of right ventricular hypertrophy, the development of the syndrome should not raise doubts.
Widespread microembolization in the lungs is not the only reason for the appearance of alveolar dead spaces in their parenchyma. The cause of alveolar dead spaces is pathological changes in the lungs during emphysema, which block the blood supply to the respirators through obliteration of microvessels.
If the ventilation of the respiran completely stops while mixed venous blood continues to flow into it (VPO = 0), then mixed venous blood begins to flow through the venules of such a respiran. This blood passes through the lungs without participating in pulmonary gas exchange and making up the volume (value) of true pathological intrapulmonary shunting
mixed venous blood.
The volume of true pathological intrapulmonary shunting is that part of the mixed venous blood that enters the lungs, which is mixed with the arterial blood, passing through the capillaries and venules of completely unventilated respirators.
If the ventilation of respirators, areas and sections of the lungs decreases without an adequate reduction in the volumetric velocity of blood flow in them, then pulmonary gas exchange in them does not stop, but only part of the mixed venous blood that enters them continues to be oxygenated. The remaining part is the physiological shunt value,
which, together with the volume of true pathological intrapulmonary shunting, constitutes in patients the value
of pathological intrapulmonary shunting of mixed venous blood.
Obstructive disorders of alveolar ventilation, causing its unevenness, sharply increase the number of respirators in which, due to low ventilation relative to the supply of mixed venous blood, physiological shunting of mixed venous blood occurs. In this way, the main link in the pathogenesis of arterial hypoxemia is formed in patients with obstructive external respiration disorders due to bronchial asthma and status asthmaticus.
How to recognize the problem?
Hypoxemia is represented by a number of symptoms that you should definitely pay attention to in order to consult a doctor in time. After all, a lack of oxygen can be an extremely dangerous condition that leads to an imbalance in the body as a whole.
So, hypoxemia will be indicated:
- increased heart rate and breathing;
- drowsiness;
- change in skin color towards pallor;
- weakness in general;
- dizziness.
If you ignore such signals from the body, later manifestations may develop, fraught with serious complications. For example, disruptions in the functioning of the heart, the development of severe swelling, problems with the functioning of the brain, as it does not receive enough nutrition. The skin may also take on a bluish tint. A person may experience anxiety, forgetfulness, and sleep problems. Potential complications include decreased blood pressure, stroke conditions, risks of developing pulmonary edema, convulsive effects, and heart rhythm disturbances.
Clinical symptoms
The insidiousness of the disease is that it does not manifest itself immediately. At the very beginning, when the body is still actively fighting, the following appears:
- Slight tachycardia
- Skin becomes slightly pale
- Blood pressure increases by several points
If measures are not taken, the disease begins to progress. And then its late signs appear:
- Cyanosis, that is, pronounced blueness of the skin, first on the earlobes, around the lips and fingertips, and then throughout the body
- The sweat becomes very sticky and cold
- The patient experiences persistent dizziness
- Motor restlessness, which gives way to stupor
- Serious neurological disorders
The outcome depends on the severity of the disease, on existing pathologies, and most importantly, on timely therapy. If hypoxemia is acute, its prognosis is very unfavorable. The list of complications includes:
- Severe arrhythmias, rapid drop in blood pressure, significant decrease in contractility of the heart muscle
- Strokes and encephalopathy
- Shortness of breath, disturbances in respiratory rhythm, pulmonary edema
How to identify the problem?
To identify heart problems, you should undergo a thorough examination by a specialist. He will take a medical history and conduct an examination. It is also recommended to use pulse oximetry to check the level of oxygen in the blood - today it is not a problem to carry it out even at home using a portable device. In addition, X-rays of the lungs and ultrasound of the heart are prescribed to exclude pathologies that can lead to a state of hypoxemia. It is recommended to take a blood test to check for a sufficient amount of hemoglobin and the absence of anemia.
How often should healthy people check their saturation? More details
Oxygen starvation in newborns
In newborns, breathing rhythm disturbances and short-term apnea are also sometimes observed during sleep. In mild cases, the pause lasts from 10 to 15 seconds, and then the child begins to breathe on his own. In more severe situations, there is no breathing for more than 20 seconds, which is very dangerous for the baby’s life.
In severe cases, signs of sleep apnea in children include blueness of the skin, lips and nails; these symptoms are associated with deterioration of cardiac function. Repeated, prolonged episodes of apnea lead to mental retardation. The violation threatens to increase the risk of sudden neonatal death syndrome and therefore requires immediate treatment.
Treatment of hypoxemia
Therapy for this condition depends on the root cause - after all, it is necessary to deal with it first. Also, if necessary, specialized therapy can be prescribed aimed at restoring redox reactions in the body, thinning the blood if necessary, reducing pressure in the corresponding circulatory system, etc. Naturally, it is performed exclusively as prescribed by a doctor based on existing symptoms and after assessing the patient's condition. Sometimes additional oxygen therapy is added.
Preventive actions
There are also a number of preventive measures that will reduce the risk of developing hypoxemia and prevent the development of serious complications. At the same time, they are quite simple and accessible to everyone. So, on the list of preventive measures:
- walks in the fresh air every day;
- physical activity, which should be moderate;
- practice breathing exercises (in consultation with a doctor);
- using vitamins and minerals in your diet;
- timely examinations by specialists to identify risks of developing cardiovascular and pulmonary diseases;
- rejection of bad habits.
Doctors note that hypoxemia is a preventable condition. The main thing is not to ignore signals from the body and correctly build your daily schedule.
There are contraindications, you should consult your doctor