Analysis number in the Science database: 131.
Alkaline phosphatase (ALP) is an enzyme belonging to the class of hydrolases that catalyzes the dephosphorylation reaction of many types of molecules, such as nucleotides, proteins and alkaloids. In humans, ALP is present in small quantities in all tissues, but especially high concentrations in the liver, bile duct, kidneys, bones and placenta. Other isoenzymes are also found:
- ALPI - intestinal,
- ALPL - nonspecific in liver, bone and kidney tissues;
- ALPP - placental.
Description
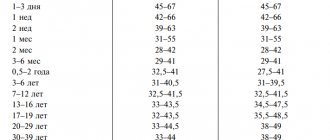
Alkaline phosphatase is present in high concentrations in the liver, bone tissue, placenta and intestinal epithelium. Each of these tissues contains specific ALP isoenzymes. A pathological increase in alkaline phosphatase activity is observed most often in cholestatic liver disease and bone diseases in which the activity of osteoblasts increases, such as Paget's disease and osteomalacia. A physiological increase in ALP activity is observed during pregnancy (due to the placental isoform of the enzyme) and in childhood, when bone growth occurs (due to the bone isoenzyme). Plasma concentrations of the enzyme are high at birth but fall rapidly thereafter. However, during childhood it remains 2–3 times higher than normal adult levels. Enzyme activity increases again during adolescence before declining to adult levels as bone growth ceases (Figure 1).
Rice. 1 — Dependence of alkaline phosphatase activity in blood serum on the age of the child. Average values shown; Peaks between 10 and 16 years of age correspond to accelerated growth during maturation and may be more than 3 times the upper normal limit for adults
The activity of alkaline phosphatase in the blood plasma of practically healthy elderly people is slightly higher than normal. This may be explained by the high incidence of mild subclinical Paget's disease in older people. ALP concentrations greater than 10 times the upper limit of normal may occur in severe Paget's disease, rickets and osteomalacia, and occasionally in cholestatic liver disease. However, these conditions are more characterized by a smaller increase in activity. ALP activity does not increase in osteoporosis unless the condition is complicated by bone collapse or fracture.
The concentration of ALP in the blood plasma usually increases with the development of malignant neoplasms of bone or liver origin, and can be associated with both primary and secondary tumors localized in these tissues. A number of tumor-specific forms of ALP, which are secreted by the tumor cells themselves, have also been described. The best known of these is the Regan isoenzyme, which is similar in thermostability to placental ALP and is found in some patients with bronchial carcinoma.
ALP activity is often measured as part of a “biochemical profile” and is often found to be elevated in the absence of clinical evidence of bone or liver disease or other biochemical abnormalities. To determine the cause of this increase, an attempt should be made to identify the tissue whose damage led to the release of the enzyme into the bloodstream. This can be done by measuring the levels of tissue-specific ALP isoenzymes, for example using electrophoresis and differential heat inactivation. A simpler but less reliable alternative is to measure the activity of γ-glutamyltransferase in plasma, an enzyme found in the liver but absent in bone tissue. Its increased activity in plasma often (but not always) coincides with an excess of hepatic alkaline phosphatase in the plasma.
What does alkaline phosphatase show?
The content of the article
Many biochemical processes occur in the human body, including the dephosphorylation reaction. In this case, phosphoric acid is separated from organic ester compounds, participating in calcium-phosphorus metabolism. This process occurs in the presence of the enzyme alkaline phosphatase.
Alkaline phosphatase is an enzyme found in many tissues of the body. But it is mainly concentrated in liver cells, bones, and placenta. The main volume is in the intestinal mucosa.
Alkaline phosphatase is represented in the body by 11 isoenzymes. To determine the cause of elevated alkaline phosphatase, it is also necessary to determine its tissue-specific isoenzymes:
- α2 – liver fraction;
- β1 – bone fraction;
- β2 – intestinal fraction.
Alkaline phosphatase is produced by the upper layer of the intestinal mucosa, but only participates secondarily in the digestive processes. The main function of alkaline phosphatase is dephosphorylation, that is, the separation of phosphoric acid from phosphorus-containing compounds. This enzyme also helps transport phosphorus throughout the body.
The enzyme is called "alkaline" because it is most active in an alkaline environment with a pH ranging from 8.6 to 10.1.
Alkaline phosphatase levels reflect the metabolic efficiency of phosphorus and calcium in the body.
Reference values (norm)
| Age | Reference values |
| Less than 4 years | 104—345 U/l |
| 4-7 years | 93—309 U/l |
| 7-10 years | 86—315 U/l |
| 10-13 years | 42—362 U/l |
| 13-16 years old | 74—390 U/l |
| 16-18 years old | 52—171 U/l |
| Over 18 years old | 30—120 U/l |
Alkaline phosphatase in adults - the norm, reasons for deviation from the norm
A test to determine the level of enzyme in the blood is carried out in the following cases:
- routine inspection;
- preparation for surgery;
- performing a set of biochemical tests - liver tests to detect liver diseases;
- diagnosis of bone tissue and bone damage;
- if patients complain of heaviness and pain in the right side under the ribs, nausea, loss of appetite and chronic fatigue.
Norm for women
After the age of sixteen, the amount of alkaline phosphatase begins to decline. But the range of its normal concentration is still quite wide.
With the onset of mature and advanced age, the level of enzymes increases again and should be (units/l):
| Woman's age | Phosphatase norm |
| 20-30 years | 85-105 units/l |
| 30-45 years | 95 – 115 units/l |
| 45-55 years | 100 – 125 units/l |
| 55-70 years | 130 – 145 units/l |
| over 70 years old | 165 – 190 units/l |
Norm for men
In adults, the amount of alkaline phosphatase varies slightly depending on gender; for men the norm is 20-25 units/l higher than for women of the same age:
| Man's age | Phosphatase norm |
| 20 – 30 years | 100-115 units/l |
| 30 – 45 years | 135 – 145 units/l |
| 45 – 55 years | 135 – 150 units/l |
| 55 – 70 years | 135 – 160 units/l |
| over 70 years old | 145 – 190 units/l |
How the biomaterial is collected
In inpatient conditions, a laboratory assistant comes to the department and draws blood in a treatment room. Patients arrive at the clinic at the appointed time in the early morning, where they are collected material for research on a first-come, first-served basis.
The laboratory assistant places up to 15 ml of the patient’s venous blood into a dry, clean test tube. The vein puncture site is treated with an antiseptic swab, which is then disposed of.
Complications without treatment
Changes in the biochemical blood test themselves do not pose a threat to human life. Diseases that cause an increase or decrease in alkaline phosphatase are dangerous.
Bone tumors can be aggressive. Early detection and initiation of specific treatment minimizes early disability and mortality in these cases and provides a chance for a high five-year survival rate. Identification of the primary site within metastasis also allows timely initiation of therapy and achievement of a favorable prognosis.
Hepatitis is dangerous and can lead to cirrhosis. This applies to viral hepatitis C, which goes unnoticed for a long time.
Cirrhosis is complicated by loss of liver function, development of bleeding, decreased protein levels, and failure of heart function.
Bone tumors are dangerous due to skeletal deformation. If metastases occur, complications depend on their location. Foci in the brain and liver are especially dangerous.
Alkaline phosphatase is not a specific marker for any disease. But this indicator indicates to specialists in which direction to look for pathology. It is important to understand that the norms differ for men and women of different ages. An additional examination is ordered to find the cause. As a result, the causative factor is identified and its specific treatment begins.
Article design: Vladimir the Great
When is a blood test for alkaline phosphatase performed?
In clinical practice, alkaline phosphatase levels acquire important diagnostic value only in combination with other laboratory and instrumental studies. Therefore, patients are usually given a biochemical blood test, which includes alkaline phosphatase.
This study is indicated for all outpatient and inpatient patients with impaired liver, kidney, digestive and endocrine system function. Currently, in most cases they are limited to determining the total level of alkaline phosphatase, since fractional analysis, although more informative, is very expensive and is carried out only in specialized laboratories.
What to do if your alkaline phosphatase level is abnormal?
When treating, the etiological direction should be indicated. If you have liver or biliary tract diseases, you should consult a gastroenterologist. The presence of cholestasis, pancreatitis, alcoholic hepatitis or cirrhosis of the liver requires appropriate medical correction, the extent of which is determined only by a doctor. Self-medication in this case can aggravate the underlying disease.
Changes in enzyme levels, including alkaline phosphatase, may occur in heart failure, cancer and serious kidney problems, as well as diabetes, so consult a cardiologist, nephrologist or endocrinologist. The doctor determines treatment tactics depending on the clinical picture.
By eliminating etiological factors, alkaline phosphatase activity is normalized. When prescribing therapy, it should be taken into account that, for example, a physiological increase in this indicator is possible with fractures, active skeletal growth and pregnancy. This does not require medical intervention. Interpretation of laboratory test results should be carried out comprehensively, taking into account other biochemical indicators and patient complaints.
Clinical observation 2
Boy G., born 04/18/2007. The mother's pregnancy was uneventful, and delivery occurred at the 39th week. The child’s height at birth was 51 cm, weight was 3800 g. Severe hypotension was noted from birth; he began sitting at 7 months and walking at 1 year and 7 months. At 6 months a decrease in weight gain and a delay in growth dynamics were recorded. From 7–8 months. The irregular shape of the head, like a “tower” skull, began to attract attention. At 1 year: height 70 cm (standard deviation coefficient (SD) -2.33), weight 7.6 kg (SD -2.58); at 2 years: height 77 cm (SD -2.69), weight 8.2 kg (SD -4.04). Taking into account the pronounced growth retardation at 2 years, after consultation with an endocrinologist, a diagnosis was made: somatogenic growth retardation. At the same age, the front milk teeth began to fall out by the roots. Due to a gait disorder (waddling, “duck-like”), the patient was consulted by an orthopedist, the conclusion was hip dysplasia. At 3 years of age, radiography of the forearm bones and a CT scan of the brain were performed. X-ray of the hands: bone age 2 years, low bone density of the metaphyses of the ulnas. CT scan of the brain: signs of craniostenosis, mild asymmetric ventriculomegaly. A consultation with a neurosurgeon was scheduled, and the diagnosis was made: craniostenosis, oxycephaly. At the age of 4–5 years, attacks of vomiting were noted that were not associated with food intake and self-limited. Due to growth retardation, a somatotropic hormone (GH) stimulation test with clonidine was performed. The maximum level of growth hormone during the test was 16.1 ng/ml, which made it possible to exclude the diagnosis of somatogenic growth retardation.
At the age of 4, for further examination and clarification of the diagnosis, the patient was sent to the Federal State Budgetary Institution "National Medical Research Center of Endocrinology" of the Russian Ministry of Health (Moscow). During hospitalization: height - 91.3 cm (height SD -2.66), weight - 11.3 kg. The results of a biochemical study revealed a significant decrease in alkaline phosphatase activity - 64-68 U/l (normal: 150-550 U/l) with normal calcium levels - 2.4 mmol/l (normal: 2.2-2.7 mmol/l ) and phosphorus - 2.02 mmol/l (normal: 1.68–2.1 mmol/l). Based on the anamnesis (growth and development delay, hypotonia, gait disturbance, early loss of primary teeth, the presence of craniosynostosis), laboratory data (low level of alkaline phosphatase), instrumental examination (areas of bone loss, according to radiography of the hands and forearm bones), a diagnosis was made : hypophosphatasia, childhood form. A molecular genetic study revealed compound heterozygous mutations (p.A37T and p.Glu191Lys) in the ALPL
.
During the observation period, growth retardation persisted, and deformities of the lower extremities and spine occurred. An orthopedist was consulted, the conclusion was: flat-valgus alignment of the feet, valgus deformity of the knee joints, scoliotic alignment of the spine, increased lordosis of the lumbar spine. Joint hypermobility syndrome.
In November 2015, taking into account the progression of the symptoms of the disease, severe retardation of growth and development, and damage to the musculoskeletal system, enzyme replacement therapy with the drug asfotase alfa was initiated at a dose of 2 mg per 1 kg of body weight 3 times a week.
As a result of the therapy, the child’s general well-being improved, growth dynamics increased significantly, tolerance to physical activity increased, and gait disturbances were leveled out. On control radiographs in dynamics: improvement in bone tissue mineralization. The patient continues treatment according to the prescribed regimen.
Clinical observation 3
Boy P., born 02/23/2009. Born at 36 weeks. with signs of malnutrition: height - 51 cm, weight - 2850. Subsequently, when assessing height gains, a decrease in growth rates was noted starting from 1 year. In the period from 2 to 7 years, growth rates ranged from 3.5 to 7 cm, which corresponded to the 5th percentile for the observation period. From the age of 3–4 years, periodic complaints of pain in the arms and legs at rest, fatigue during normal physiological stress, headaches at rest and after emotional stress with a frequency of 1 time in 1–2 weeks, which were relieved with the help of non-steroidal anti-inflammatory drugs, were noted. .
At the age of 5 years and 3 months. We consulted a pediatric endocrinologist about short stature (height SD -2.37). Hospitalization was recommended for examination in a hospital, where primary idiopathic subclinical hypothyroidism was identified. According to laboratory data: thyroid-stimulating hormone 12 µIU/ml, free thyroxine 18.6 pmol/l. Ultrasound picture of the thyroid gland without pathology, the right lobe is 2.1 cm2, the left is 1.5 cm2, the isthmus is 1.6 mm. Therapy with sodium L-thyroxine at a dose of 25 mcg was initiated.
At 6 years and 9 months. during radiographic examination, the bone age corresponded to the biological age of 3.5 years. At 7 years of age, the growth rate is +6.4 cm/year, growth CO is -2.1. Indications for a stimulation test with clonidine were determined, but the mother refused the test.
At 6 years and 2 months. For the first time, a decrease in the level of alkaline phosphatase was registered - 88 U/l, with repeated measurements a year later - 108 U/l (normal: 150–550 U/l).
Taking into account the syndrome of short stature in combination with damage to the musculoskeletal system (pain in the extremities, poor posture, deformation of the chest), a significant delay in bone age according to radiography, and a persistent decrease in the level of alkaline phosphatase, the patient underwent a molecular genetic study and the mutation p.571 was identified. G>A in the ALPL
in a heterozygous state
.
A diagnosis was made: hypophosphatasia, childhood form.
From January 2021, after a consultation, taking into account the progressive nature of the disease, it was decided to initiate enzyme replacement therapy with the drug asfotase alfa at a dose of 2 mg per 1 kg of body weight, 3 times a week. subcutaneously
The beginning of therapy was accompanied by episodes of hyperthermia, with a reaction at the injection site (twice), however, after desensitizing therapy and following the recommendations for a hypoallergenic diet, the reactions were stopped, the patient continued to receive treatment.
During treatment, stable positive dynamics are observed: a significant increase in growth rates, an increase in muscle strength and tolerance to physical activity, and pain in the lower extremities has been relieved. The child continues the recommended treatment.
What indicators are considered normal?
An increase in test results does not always indicate the development of a disease - perhaps the child has a disturbance in the functioning of the body and it needs to be identified more quickly. Normal levels of alkaline phosphatase in a child’s blood include:
- immediately after birth, results will vary between 250 units per liter of blood;
- 5 days after birth they will drop to 231 units;
- up to the 6th month of the baby’s development, the norm will be considered to be 449 units per liter of blood;
- from 6 months to 1 year, the optimal level will be 462 units/l;
- up to 3 years, the indicators will decrease slightly to 281 units;
- from 4 to 6 years, the level of alkaline phosphatase in the blood will be 269 units/l;
- up to the age of 12, the norm is 300 units;
- upon reaching 17 years of age, the indicators increase again: for boys the norm is 390 units, for girls 187.
It is important to note that these indicators may “jump” slightly up and down, but not by more than 10 units. If the results are greatly increased, this may also indicate the research method or reagents used for analysis. However, in this case, it is better to talk to a doctor about the child’s well-being in order to promptly determine the development of dangerous diseases occurring latently in the body.
The table below shows the normal levels of alkaline phosphatase in the blood:
How is the alkaline phosphatase test performed?
To get the correct test result, you must follow these rules:
- the test may be performed in a laboratory, from which a healthcare professional takes a blood sample from the bloodstream and places it in a closed container for testing;
- Blood sampling is carried out in the morning from the ulnar vein in the amount of 5-10 ml;
- the test should be performed on an empty stomach and it is best not to eat for at least 12 hours before taking blood;
- the day before donating blood, you should not engage in heavy physical work or sports associated with severe stress;
- Avoid drinking alcohol and drugs that increase alkaline phosphatase levels.
Typically, test results are ready in 1–2 days.
Features of determining alkaline phosphatase
Blood serum is used for analysis. In most cases, the top layer formed in the separator tube is taken. The activity of this enzyme may vary slightly when blood samples are stored at room temperature. Hemolysis in vitro does not affect the test results.
Signs of diseases of internal organs
Advertising:
You can suspect that a child is developing some kind of pathology if you carefully monitor his general condition. An increase in alkaline phosphatase levels is not the only sign that indicates that all is not well with your baby:
- Pathologies of bone tissue
. In this case, the child often complains that his legs or arms hurt. He cannot play active games for a long time, run, jump, because he gets tired quickly and needs to constantly rest. In severe cases of the disease, even deformation of the limbs is possible. - Liver pathologies
. The baby becomes lethargic and apathetic. Refuses to eat. His body weight decreases. Nausea and vomiting may occur, and the color of the skin may change - it becomes yellow or brown. Certain diseases sometimes cause nosebleeds. If you conduct a blood test, then along with an increased level of alkaline phosphatase, you can find that the level of ALT is also abnormal. - Malignant neoplasms
. For a long time, the tumor does not manifest itself at all. The child still leads a normal life. His condition worsens sharply - he becomes lethargic, loses his appetite, loses weight, and gets tired quickly. To identify a neoplasm, it is necessary to conduct a thorough diagnosis, which will include both laboratory and instrumental techniques. - Infectious mononucleosis
. In this case, the first sign of the development of pathology is an increase in temperature. The baby himself becomes lethargic, capricious, and does not want to eat. In addition, he develops a cough and sneezes frequently. If you examine his throat, you will notice the appearance of white plaque on his tonsils. Certain groups of lymph nodes become enlarged. - Rickets
. Young children are more susceptible to this disease. It develops due to insufficient intake of vitamin D into the baby’s body. The first symptoms are increased sweating, hair loss in the occipital region of the head, hypotension of the muscles of the extremities. If appropriate treatment is not carried out in time, the skull and limbs will subsequently become deformed. - Acute intestinal infections
. This group includes a lot of diseases - rotavirus infection, salmonellosis, dysentery, yersiniosis and others. The symptoms are as follows: the temperature rises, the stomach hurts in all parts, nausea and vomiting, and diarrhea appear. Because the child loses a lot of fluid, the water balance is disturbed.
Advertising:
If you have these symptoms, it is recommended not to self-medicate, but to immediately go to a medical facility for help. In childhood, many diseases are more severe, and their consequences can be dangerous. The sooner a particular disease is detected, the easier it will be to cure it and return the baby to normal life.
Alkaline phosphatase levels are below normal
A decrease in enzyme content can signal the appearance or presence of dangerous diseases in the body.
Reasons for decreased enzyme levels:
- severe anemia;
- hypothyroidism – decreased levels of thyroid hormones;
- significant blood transfusions;
- fetal malformations, for example, placental insufficiency - a common complication of pregnancy;
- frequent use of oral contraceptives;
- hypophosphatasia is a rare but life-threatening disease;
- radioactive contamination - in this case, measuring blood parameters will show the accumulation of radioactive isotopes;
- malnutrition, lack of magnesium, zinc and vitamin C;
- Excess vitamin D can cause a change in the reagent when diagnosing certain diseases, for example, rickets.
Prevention
Advertising:
There is no specific prevention. You can prevent the development of various diseases of internal organs in a child if you follow simple recommendations:
- enrich the baby’s diet with vitamins and minerals;
- for the purpose of prevention, take vitamin D;
- physical activity should be standardized;
- the child should spend more time outdoors;
- make sure that the baby does not eat junk food - crackers, chips, fast food;
- do not self-medicate, do not give your child medications without consulting a doctor;
- teach hygiene rules.
It is impossible to protect a child from everything in the world. But parents are quite capable of reducing the likelihood that he will get any dangerous disease. The main thing is to devote more time to the baby and carefully monitor his health. If your health worsens, you must seek help from a medical facility.