The importance of blood can hardly be overestimated: it carries oxygen and nutrients to tissues, helps regulate the functioning of the body by transporting hormones and other active substances, helps regulate temperature and performs a host of other tasks.
Obviously, a decrease in blood volume has a negative impact on the overall functioning of the body.
However, nature provides a mechanism for protecting against excessive blood loss - the ability of blood to thicken and coagulate, covering the damaged area. The level of blood clotting is a kind of indicator of the body’s survival.
Coagulation indicators and their norm in children
Blood is not a homogeneous liquid, but a suspension of many cells in a water-protein solution - plasma.
There are many types of blood cells, which (to simplify somewhat) can be divided into three groups.
- The first is erythrocytes, also known as red blood cells, which transport oxygen to tissues.
- The second is leukocytes, white blood cells that absorb and neutralize foreign objects (viruses, bacteria, etc.).
- The third is platelets, the cells responsible for the ability of blood to clot.
When the integrity of the vessel wall is damaged, special substances are released from the damaged tissues, the so-called coagulation factors (mainly proteins).
They activate platelets and cause them to stick to the edges of the wound and connect with each other, forming a dense clot that covers the damaged area.
In turn, platelets also secrete a special substance that activates the fibrinogen protein dissolved in the plasma.
It begins to transform into the protein fibrin, which is capable of forming long elastic cords in which red and white blood cells “get stuck.” Thanks to this, the clot covering the wound becomes denser, and its edges begin to tighten.
The blood clotting process is characterized by many indicators.
- Platelet level is the number of cells responsible for the blood clotting process.
- The duration of bleeding is the time that passes from the moment the integrity of the vessel is damaged until a blood clot forms.
- Clotting time is the duration of formation of a blood clot.
- Prothrombin time is the rate of activation of a certain factor (namely factor VII, proconvertin) involved in the “launch” of the coagulation process in the early stages. This factor activates the formation of thrombin, a substance that promotes the conversion of fibrinogen into fibrin. In other words, this is the rate of formation of a blood clot after exposure to substances from the tissues of a damaged vessel.
- Thrombin time is the rate at which fibrinogen is converted into fibrin.
- Activated partial thromboplastin time (aPTT) is the duration of the formation of a blood clot without the participation of external factors, i.e., without damage to the vascular walls and the release of corresponding substances, solely due to factors initially present in the blood in an inactive state.
- Fibrinogen level is the amount of fibrinogen protein that can be converted into fibrin.
- Antithrombin III level is the level of antithrombin III protein in the blood, which prevents blood clotting. This protein is needed in the blood so that coagulation processes, relatively speaking, do not start without a serious reason. Increased blood clotting is no less dangerous than decreased blood clotting - it often causes the formation of blood clots and blockage of blood vessels.
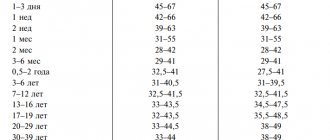
The values of these indicators for children aged 3 to 14 years are almost the same:
- number of platelets in thousands per 1 cubic milliliter of blood – 180-320; in girls in adolescence, at the onset of menstrual bleeding, the platelet count may decrease to 75-220;
- duration of bleeding - can be determined in accordance with different methods: according to Duke, the norm is 2-4 minutes, according to Ivey and Lee-White - less than 8 minutes, according to Sukharev less than 5 minutes;
- clotting time – from 2 to 5 minutes;
- prothrombin time – 11-15 s;
- thrombin time – 15-18 s;
- APTT – within 24-35 s; specific indicators may vary significantly depending on the determination method and the reagents used;
- fibrinogen level – 2-4 g/l;
- antithrombin level - 101-131% - in children from one to 6 years old, 95-134% - in children from 6 to 11 years old, 96-126% - in adolescents under 16 years old.
The importance of these indicators and their role in the blood clotting process should be considered separately.
Blood clotting
Many people begin to fear blood clots after, when donating blood from a vein, the nurse reports that it is too viscous. Those who have too thin blood that successfully fills the test tube hope that they are protected from thrombosis. But viscosity and coagulability are two completely different concepts, and one does not always determine the other.
How viscous you are
Increased blood viscosity, due to which it becomes less fluid, most often occurs due to the predominance of its formed elements over liquid ones. This happens due to too strict adherence to the recommendations “do not eat 12 hours before taking the test” and because of the decision to add one more restriction to this – not to drink. Just to be sure. The end result is worse - and the blood flows poorly into the test tube, and some indicators (for example, hemoglobin, hematocrit, total number of red blood cells, white blood cells and platelets) turn out to be artificially high. Therefore, it is important to remember: before taking blood tests, you should not limit yourself to fluids.
Another common cause of increased viscosity is increased levels of red blood cells and hemoglobin, characteristic of smokers. After all, the more smoke and less air a person inhales, the greater the concentration of oxygen carriers required. Their compensatory increase is formed. Therefore, visually, the blood of smokers often appears more viscous.
According to hematologists, true diseases (thrombocytosis, erythrocytosis, etc.) associated with increased blood viscosity account for a small number of all cases of “viscous blood”. And this is clearly visible from a routine general blood test - the doctor will immediately notice that the number of red blood cells or platelets is too high.
Normally, the content of red blood cells is 3.7-5.1, platelets - 180-320.
Viscosity and coagulability - what's the difference?
The most important indicator is blood clotting. Unfortunately, it can be difficult to obtain accurate information about coagulation, even despite the level of development of medicine. On the one hand, obvious diseases with clotting disorders, such as hemophilia, have long been known. On the other hand, there is a lot of hidden pathology, which may not show itself for a long time, but once manifested, it can quickly lead to serious consequences.
Only in recent decades have researchers learned to identify these problems using high-tech genetic tests. Considering that, according to statistics, more than 1-3% of the world's population has a congenital pathology of the blood coagulation system, it is likely that in the future these tests will be carried out in the maternity hospital for every newborn. And absolutely for those who need to be prescribed certain medications that can increase the risk of blood clots.
Protection or danger?
For example, this is very important to do before prescribing hormonal contraceptives. Their ability to enhance blood clotting and occasionally lead to thrombosis (as it turns out, this almost always occurs in women who have a hidden clotting disorder) has been known for several decades. Due to the widespread use of this method of protection against unwanted pregnancy these days, the incidence of thrombosis in young, apparently healthy women has increased. At the same time, when prescribing COCs, gynecologists rarely focus their patients’ attention on this danger. They can be understood - the complication is infrequent in general, and I don’t want to once again intimidate patients, as if pushing them into an unwanted pregnancy. Meanwhile, the most advanced Western colleagues have already included a full blood clotting test in the mandatory examination algorithm before prescribing hormonal contraceptives.
What will the analysis show?
What tests need to be done to check blood clotting? The most common and familiar analysis to many, a coagulogram, may not answer all questions, especially in the prevention of thrombosis.
However, a classic coagulogram is the first stage of a screening examination of the coagulation system. If it reveals abnormalities, the next step will be more detailed studies of hemostasis - thromboelastography or thromboelastometry. A separate story is the determination of D-dimer , Leiden mutation and other genetic clotting disorders - tests that reveal a tendency to form blood clots in the future. What is necessary and in what cases?
The most common standard coagulogram today includes five components: PTI (prothrombin index); INR (International Normalized Ratio. Reflects the ratio of the patient’s blood clotting time to the blood clotting time of a healthy patient; APTT (activated partial thromboplastin time. Estimates the time it takes for a blood clot to form after special reagents are added to the plasma), FIBROGEN and PLATELET LEVEL.
At the same time, APTT is informative only in people undergoing treatment with heparin, and INR is important only for people constantly taking blood-thinning drugs from the neodicoumarin group (warfarin).
It turns out that two out of five indicators are not so important for screening. The total number of platelets is also not always indicative, because with most coagulopathies it is not their number that changes, but primarily the functional activity.
Therefore, the most informative method, which allows one to evaluate several stages of blood coagulation at once, is thromboelastography. This is a kind of detailed observation of the formation of a blood clot, and its subsequent dissolution (lysis) with the construction of graphs of each of the stages. Thromboelastometry is another version of this study, which is considered even more informative. Unfortunately, the instruments for conducting these studies are expensive and require special training of personnel, so not every laboratory can offer thromboelastography services.
Another important indicator is D-DIMER (this is a breakdown product of fibrin, a small fragment of protein present in the blood after the destruction of a blood clot).
It is actively used to determine the risk of blood clots. Those with even slightly elevated D-dimer are at much greater risk of developing blood clots than others. It is necessary to monitor D-dimer in case of venous diseases (thrombophlebitis), after surgical interventions and upon discharge from the hospital if you have been bedridden for a long time. Monitoring D-dimer levels is useful during pregnancy and when taking hormonal contraceptives (the risk of blood clots in the presence of the Leiden mutation while taking birth control pills increases almost 9 times). And now during COVID-19 and several weeks after recovery.
Today, in addition to D-dimer testing, genetic tests for congenital bleeding disorders are emerging. The most common of these is the Leiden mutation, which occurs in 2–6% of Europeans. The presence of a defective gene increases the likelihood of venous blood clots 6–8 times, and the risk of heart attack and stroke increases significantly. But other mutations, of which there are more than ten today, are no less dangerous. At the same time, timely prevention of thrombosis (mainly the constant use of anticoagulants, the exclusion of certain foods and medications, wearing compression stockings when flying and working on your feet, etc.) reduces the risk of dangerous complications tenfold.
Flickering problem
If everything is in order with the coagulation system, a possible cause of increased coagulation may be arrhythmia, namely atrial fibrillation. According to statistics, 2% of the planet's population suffers from paroxysmal (occurring in attacks) or permanent form of atrial fibrillation. This problem usually appears after thirty. The basis for the disorder is the appearance of pathological turbulence of the electrical impulse in the atria, which gives the myocardium extraordinary electrical stimuli. In medical language, this is called the “re-entry” or re-entry mechanism. As a result, the atria become a churn that churns blood into clots like milk into butter. The situation worsens even more in the case where the person initially had the same clotting disorders. Blood clots can form within 48 hours after the onset of an attack and “fly away” into the arteries of the brain, causing an ischemic stroke, into the intestines, leading to mesenteric thrombosis, into the arteries of the extremities, provoking their acute ischemia.
Von Willebrand factor and COVID -19.
Severe COVID-19 may be associated with elevated levels of one of the blood coagulation factors, von Willebrand factor. Anna Aksenova, a senior researcher at the Laboratory of Amyloid Biology at St. Petersburg State University . Her scientific article was published in the journal Ecological Genetics. It has already been proven that the SARS-Cov-2 virus can have a direct damaging effect on the inner wall of blood vessels. In response to damage, the body strives to “patch” the hole as quickly as possible, and the leading role in this is played by the von Willebrand factor, which is involved in the activation of platelets and, in fact, triggers the process of local thrombus formation. In the course of research, it turned out that some people are characterized by an increased concentration of this factor in their cells, so, as a rule, it is higher in people with blood group II. An individual characteristic of the body is also possible. As a result, in response to massive microdamage to blood vessels, massive microthrombosis occurs, which causes the appearance of larger and more dangerous blood clots.
Genetic mutations of the coagulation system identified during tests:
MUTATION OF COAGULATION FACTOR V OF BLOOD CLOTTING (LEIDEN FACTOR)
PLASMINOGEN ACTIVATOR INHIBITOR 1
MUTATION OF COAGULATION FACTOR II (MUTATION OF PROTHROMBIN)
MUTATION OF METHYLENETETRAHYDROPOLATE REDUCTASE (MTHFR C677T)
MUTATION OF COAGULATION FACTOR VII OF BLOOD CLOTTING (F7 ARG353GLN)
POLYMORPHISM OF THE METHIONINE SYNTHASE REDUCTASE GENE (MTRR A66G)
FIBRINOGEN MUTATION, BETA (FGB G-455A)
MUTATION OF THE PROMOTER OF THE COAGULATION FACTOR GENE FVII (-312 INS 10BP)
INSERTATION/DELETION OF ALU ELEMENT IN THE ANGIOTENSIN CONVERTING ENZYME GENE (ALU INS/DEL)
PLATELET GLYCOPROTEIN 1B ALPHA SUBUNIT MUTATION
PLATELET ADP RECEPTOR MUTATION (P2RY12 H1/H2)
MUTATION A1298C OF METHYLENETETRAFOLATE REDUCTASE GENE
D-dimer is significantly elevated in most patients with moderate to severe COVID-19. Therefore, all patients receive therapeutic doses of anticoagulants.
The Leiden mutation is the most common hidden bleeding disorder, occurring in 2-6% of Europeans.
Published: January 19, 2021
Bleeding time
There are many methods for studying the duration of bleeding, differing in the method of blood sampling and the method of implementation.
Currently, three methods are especially widely used:
- Ivy:
- Duke;
- Sukhareva.
The duration of bleeding according to Ivey is determined as follows: a tonometer is fixed on the patient’s shoulder, with its help a pressure of 40 mm Hg is injected. st, then a small incision is made with a blade on the inside of the forearm. After this, the time is recorded on a stopwatch, and a special filter is applied to the incision every half a minute to absorb blood. When there are no traces of blood left on the filter, the bleeding is considered to have stopped.
This method can only be used with older children and adolescents - it is considered quite aggressive.
The Duke method is more popular and is considered more gentle. To test using this method, you do not need to use a tonometer or make an incision - a small puncture of your finger or earlobe with a special Frank needle is enough. A paper filter is also applied to the puncture site, but not every half a minute, but every 15 seconds. The blood clotting rate in the Duke study does not exceed 4 minutes.
This method is used more widely and is more often used in children.
Sukharev's method is as follows: a blood sample is taken from a finger, then placed in a test tube; The tube is tilted from side to side until the blood sample begins to thicken. The norm from start to finish of coagulation is no more than 5 minutes.
Prothrombin
Prothrombin is a protein that is converted into thrombin during blood clotting; thrombin, in turn, starts the process of converting fibrinogen into fibrin.
When analyzing blood, attention is paid to such an indicator as prothrombin time.
This is the time during which the blood, under the influence of tissue factors, forms a clot.
For children under 14 years of age, this time normally ranges from 11 to 15 s; in infants this figure may be slightly higher - from 14 to 16 s.
An increase in prothrombin time indicates disturbances in the synthesis of prothrombin or fibrinogen.
The reason for this may be:
- liver disease or increased load on the liver as a result of intoxication;
- deficiency of vitamin K, which promotes the production of prothrombin;
- calcium deficiency;
- a decrease in the number of platelets due to allergies, radiation sickness or other disorders;
- anemia;
- hemophilia;
- increased levels of heparin (a protein that prevents blood clotting).
A decrease in prothrombin time can be caused by:
- excess vitamin K;
- increased platelet levels;
- genetic failures that disrupt the production of certain coagulation factors.
Thrombin time
Thrombin time is the time it takes fibrinogen to convert to fibrin during the final stages of the coagulation process.
Normally, in children under 14 years of age and adults, the thrombin time is 15-18 s; in infants, this figure may be slightly higher.
An increase in thrombin time may indicate serious disorders, such as:
- liver diseases;
- DIC syndrome (disseminated intravascular coagulation);
- acute leukemia;
- severe intoxication.
However, a relatively harmless lack of vitamin C can also cause an increase in thrombin time.
A decrease in thrombin time can be caused by reasons such as:
- the presence of malignant tumors;
- acute form of an infectious disease (influenza, tuberculosis, pneumonia);
- DIC syndrome in the initial stage.
Thrombin time may also decrease after serious injuries or burns.
Fibrinogen
From all of the above, it can be understood that fibrinogen - the protein from which fibrin is formed - is extremely important for the normal process of blood clotting. The fibrinogen level for children under 14 years of age is from 2 to 4 grams per liter of blood, in infants - from 1.5 to 3 grams per liter.
A decrease in fibrinogen levels can be caused by:
- DIC syndrome;
- serious liver dysfunction; severe intoxication;
- lack of vitamins C and B;
- genetic disorders.
An increase can be caused by:
- acute infectious diseases;
- the presence of malignant tumors;
- diabetes.
Scope of the study
A hemostasiogram is performed several times during pregnancy for the timely detection and correction of violations of the coordinated functioning of the coagulation and anticoagulation systems of the blood. It is necessary to prescribe additional analysis if:
- A history of several missed pregnancies or miscarriages.
- When early and late gestosis appears, the symptoms of which are increased blood pressure values, the presence of edema and/or protein in the urine.
- With uterine hypertonicity (threat of miscarriage).
In addition to pregnancy, a coagulogram is prescribed:
- For coronary heart disease, heart attack.
- For varicose veins.
- For chronic liver diseases.
- For acute and chronic cerebral circulation disorders.
- For thrombosis and thromboembolism.
- In preparation for surgery and in the postoperative period.
- For hemophilia, thrombocytopenic formula, increased bleeding, numerous hematomas.
Antithrombin
Antithrombin III is an extremely important protein that regulates the level of blood clotting, preventing its excessive thickening and the formation of blood clots. To assess the general condition of the blood, it is necessary to know the level of antithrombin.
The content of antithrombin in the blood varies greatly depending on age: in infants it is the lowest - 60-90%, in children from one to six years old it reaches a maximum value - 101-131%, then gradually decreases, in adults reaching 66-124% .
An increase in antithrombin levels is observed when:
- acute inflammatory processes in the body;
- acute viral hepatitis;
- lack of vitamin K.
A decrease in antithrombin levels may accompany:
- liver diseases;
- DIC syndrome;
- sepsis;
- congenital disorders of antithrombin synthesis.
WHAT ARE COAGULATION DEVIATIONS ASSOCIATED WITH?
Any deviation from these standards is considered a violation and may pose a risk to humans. A bleeding disorder is associated with one or more of three factors:
- imbalance of the hemostasis mechanism;
- pathology of the walls of blood vessels;
- platelet functions.
The latter are the smallest particles of blood, the so-called red plates. They are destroyed during tissue injury, releasing serotonin and thromboplastin into the blood. The first narrows the walls of blood vessels, reducing blood flow, the second is involved in the formation of a blood clot.
Coagulation disorders—thickening of the blood—are commonly associated with a long series of diseases. Coagulability may decrease with age, after surgery, or taking certain medications.
What diseases provoke bleeding disorders?
Disorders associated with reduced blood clotting provoke pathologies such as:
- congenital blood diseases;
- cancer;
- jaundice when combined with a deficiency of vitamin D in the blood;
- hemorrhagic and hormonal disorders;
- most autoimmune diseases are accompanied by bleeding disorders;
- After transfusion, coagulation disorders are not uncommon with the slightest inaccuracy in the selection of donor blood.
Bacteremia and infection can lead to disruption of the natural defense system against blood loss. Often blood clotting decreases due to prolonged physical inactivity. Atherosclerosis and other pathologies of the vascular channels of the brain can provoke bleeding or a critical slowdown in blood flow. When dehydrated, there is often an elementary fluid deficiency, which increases blood clotting.
Often, pathologies associated with platelet deficiency or surplus are observed during invasive interventions. Long-term catheterization, frequent injections, operations with large volumes of plasma infusion (with blood loss) - all this can lead to disruption.
Blood gradually loses its ability to clot normally during the uncontrolled course of critical illnesses. Coagulation disorders are a common complication of diabetes, obesity, and hypertension. Increased clotting is observed in pregnant women, smokers, and cancer patients at the recession stage.
Reasons for deviation from the norm
The most common causes of changes in blood clotting parameters are disseminated intravascular coagulation syndrome, hemophilia, intoxication and acute inflammatory processes. These conditions are most often diagnosed based on the results of coagulation tests. However, we should not forget that changes in the composition of the blood can also reflect other pathological processes in the body.
The condition of the blood is influenced by many factors; it somehow “reflects” any violation of the normal state of the body. Therefore, it is necessary to pay attention to any non-standard test results, especially when it comes to the health of the child.
Why is it worth doing a blood clotting test at the State Scientific Research Center of PM?
The reason is simple - we take our work seriously. We have modern high-precision equipment for laboratory research. A staff of qualified and experienced specialists has been recruited.
In addition, if you need a coagulogram, the price of this analysis will be extremely low - we value our visitors and always try to meet them halfway!
Come - we don't have queues or rudeness. We do not lose or confuse tests and can, if necessary, immediately after receiving the results, refer you to a highly qualified doctor.
The page is for informational purposes only. Find out the exact list of services provided and the specifics of the procedures by calling.