Depending on age, the frequency of bowel movements, consistency and color of stool are different. In infants, the frequency of bowel movements can be up to 7-8 times a day and up to 1 time every 2-4 days, and this is the norm. In children of the 2nd year of life, the number of bowel movements is 1-2 times a day. The stool should be well-formed and of soft consistency, the number of bowel movements is determined by the child’s individual rhythm - the baby is healthy and there is no need to worry.
If the baby's stool is liquid or looks like "sheep" feces, it is advisable to consult a pediatrician and examine the child as planned.
The color of the stool may vary, mainly depending on what foods the child eats. But if the baby’s stool has become black and sticky, it may be bleeding (stomach or intestinal); if it has become colorless, it may be a liver or gallbladder disease.
URGENT CARE
Call an ambulance if:
- The child's stool has become black and sticky
- a child's stool is profusely mixed with scarlet blood (bleeding from the lower gastrointestinal tract, mainly the large intestine)
THE DOCTOR'S CONSULTATION
Contact your pediatrician if:
- the skin and mucous membranes turn yellow and the stool is discolored
- the child's stool is large, greasy and has an unpleasant odor (a sign of poor digestion)
ATTENTION!
If the stool is copious, greasy, or foul-smelling, this is a sign of poor digestion. A doctor's consultation is required .
| ASK YOURSELF A QUESTION | POSSIBLE REASON | WHAT TO DO |
| The general condition is good, there is a tendency to constipation, the child has pain when defecating, and a few minutes later there is blood on the toilet paper and a little in the stool | Anal fissure | Consultation with a pediatrician for examination and examination |
| Change in stool after taking medications (antibiotics), becoming more liquid | Side effects of drugs | Consultation with a doctor to discontinue the medication or reduce the dose and course of treatment |
| The child feels well but has dark-colored stools (is taking iron supplements, or has eaten blueberries or dark green vegetables) | Effect of medications or food on stool | The baby is fine, no need to worry |
| The baby's stools have become clayey and light in color, his urine has darkened, his skin has a yellowish tint, and his sclera (the whites of his eyes) have turned yellow. | Viral hepatitis (older children) Congenital liver disease or biliary atresia (newborns) | Call your pediatrician immediately, for examination and treatment, the child may be hospitalized. Before the doctor arrives, keep the baby calm. |
| The stool is faintly colored, smells unpleasant, is greasy and profuse | Insufficient digestion | Consultation with a pediatrician (or gastroenterologist ) for examination and treatment prescription |
| An increase in temperature, a violation of the general condition, an admixture of dark burgundy or scarlet blood in the stool | Inflammatory diseases of the gastrointestinal tract, bleeding from different parts of the intestine | Call emergency services immediately ; hospitalization for examination and treatment is possible. |
| Stools resemble coffee grounds or are black and sticky | Bleeding from the upper gastrointestinal tract (esophagus or stomach), called melena | Call emergency services immediately ; hospitalization for examination and treatment is possible. |
FOR INFORMATION
Stool color and consistency
The color and consistency of your child's stool may change from time to time - this is normal. However, traces of fresh blood or black, sticky stools may be signs of bleeding and require urgent evaluation. The sudden appearance of loose stools, with or without mucus, indicates diarrhea. If the stool is copious, greasy, smells bad, and is faintly colored, these are signs of poor digestion of food. In all these cases, an examination by a pediatrician is required. If your child's stool is light, clay-colored and his urine has become dark, viral hepatitis is possible - call your pediatrician immediately .
Minor changes in stool color are related to diet. In breastfed children, the stool is soft, almost liquid, reminiscent of light mustard. It may contain particles that look like seeds. With artificial feeding, the stool is yellowish-brown or yellow, denser, but still no denser than putty. If the stool is very hard and dry, this may be due to a lack of fluid or excess fluid loss, for example, with sweat due to an increase in temperature, etc. If the child has eaten a large portion of vegetables or other difficult-to-digest foods, digestion may slow down and the stool may be very dark colors. Beetroot or red-colored foods may cause your stool to become reddish (for the same reason, your urine may turn pink).
The stool turns blue, purple, or another shade if the child tastes crayons. In this case, as soon as the colored substance is released from the intestines, the stool returns to its normal color. If the child's condition worsens, call the pediatrician immediately - poisoning is possible.
Causes of bloody diarrhea in a child
Loose stools with blood in a child are not an independent disease, but a set of symptoms that accompany the course of various pathological processes. In this situation, diarrhea, which has a number of age-related characteristics, may vary in the frequency of bowel movements and the volume of feces. This is primarily determined by the nature of the disease that caused it and the localization of intestinal bleeding.
The most common causes of bloody diarrhea in a child include:
- acute intestinal infections (dysentery, salmonellosis, escherichiosis, Proteus/staphylococcal/rotavirus infection, etc.);
- parasitic diseases (amoebiasis, giardiasis, helminthiasis);
- intolerance to cow's milk, soy (can develop in formula-fed infants);
- reaction to certain medications;
- internal hemorrhoids (a consequence of congenital dilatation of hemorrhoidal veins, prolonged sitting on a potty, strong prolonged crying, etc.);
- juvenile polyps (benign neoplasms). Identified at the age of 4–7 years. When introduced into the intestinal lumen, they can cause mild diarrhea with blood in a child;
- Crohn's disease (chronic inflammatory bowel disease);
- ulcerative colitis (inflammation of the colon mucosa). Usually occurs in school and adolescence, less often in children of the first year of life;
- systemic lupus erythematosus (autoimmune pathology of connective tissue and blood vessels). In some cases, it may be accompanied by diarrhea streaked with blood.
Expert opinion
Anorectal fissure in a child is a relatively favorable condition compared to adults. If you seek specialized help in a timely manner, the problem can be eliminated conservatively in a short time. Due to the good ability to restore the mucous membrane in children, therapy can take only 4-5 days. The main thing is not to ignore the first signs of the disease. Otherwise, an acute crack becomes chronic, becomes a cause of daily discomfort for the patient, and requires surgical intervention.
Associated symptoms
If a child develops loose stool mixed with blood, it is necessary to determine other accompanying symptoms. This will help in the future to describe to the doctor a complete picture of the baby’s condition and provide him with full assistance.
Body temperature
If a child’s usual stool is replaced by diarrhea with blood without fever, this may be evidence of:
- allergic reaction;
- indigestion after overeating;
- a sudden change in the usual diet;
- early incorrect introduction of complementary foods;
- severe stress, fear;
- mild food poisoning.
However, such a disorder can also be caused by more serious reasons. Therefore, the appearance of even minor blood impurities in the stool is a good reason to consult a doctor.
Vomiting and diarrhea with blood in a child with a fever is the first sign of an acute intestinal infection. Such symptoms are usually accompanied by weakness, dizziness, body aches, pain, rumbling and cramps in the abdomen, and a false urge to defecate.
Change in color of stool, presence of mucus
If the disorder develops, you should take a very close look at the stool. Sometimes parents mistake incompletely digested red foods (tomatoes, beets, paprika, blueberries, currants, etc.) for blood streaks.
The most dangerous condition that requires immediate medical attention is red diarrhea in children. The appearance of scarlet blood can mean rapid massive hemorrhage in the colon or other parts of the intestine.
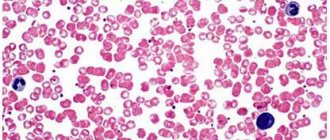
The presence of liquid stool that is dark brown or black in color (so-called melena) indicates the presence of a source of bleeding in the upper gastrointestinal tract or inflammatory changes in the walls of the small intestine.
Foamy yellow-green, greenish, light brown and other colors of diarrhea in a child with streaks of blood and mucus usually develops against the background of an acute intestinal infection.
Anal itching
If bloody diarrhea in a child is accompanied by itching in the anus, this may be evidence of injury to the internal hemorrhoid.
Causes of anal fissure
The pathogenetic basis for the development of anal fissure in children is a violation of the integrity of the anal mucosa. The cause of such a defect may be:
- Tear of tissue due to the passage of too thick stool.
- Incorrect placement of cleansing enemas or gas exhaust tubes when the mucous membrane is injured by hard elements of medical products.
- Incorrectly performed surgical interventions in the anorectal area.
It is important to understand that a violation of the integrity of the mucous membrane in the described situations does not always occur. The risk of developing the problem is increased by provoking factors:
- Genetic predisposition or the presence of congenital malformations of the anorectal region or the entire gastrointestinal tract (GIT).
- Chronic intestinal infections accompanied by diarrhea. In such cases, the mucous membrane becomes thinner and becomes more vulnerable to the mechanical impact of thick feces.
The situation is further aggravated by the presence of a local inflammatory process.
- Proctitis and other diseases of the rectum, which directly reduce tissue resistance.
- Metabolic disorders. Diabetes mellitus and pathology of absorption of individual food components create conditions for defecation disorders and changes in the normal architecture of tissues.
- Traumatic injuries to the anorectal area - falls, blows, scratching of the anal area against the background of helminthic infestation.
First aid for bloody diarrhea
What to do if a child has bloody diarrhea? First of all, you need to call a doctor or ambulance. Before their arrival, to alleviate the condition and prevent dehydration, older children should alternately be given a little sweet tea and salted water every 5-10 minutes. Infants need to be put to the breast more often. It is also important to limit your food intake until further instructions from your doctor.
* Among products based on Loperamide. Based on sales in money for February 2021 - January 2021, according to IQVIA (from English IQVIA).
Calculation of fluid volume for healthy children
Children under 1 year of age
should drink at least 100 ml of water per day.
For healthy children weighing from 10 to 20 kg
Water demand is calculated using the formula:
100 ml (volume of water for children under 1 year) + 50 ml per kg for body weight over 10 kg.
For example, with a weight of 12 kg: 100 ml + 2 x 50 ml = 200 ml.
A child weighing 20 kg should drink water: 100 ml + 50 x 10 = 600 ml
For children weighing over 20 kg
The following formula for calculation is proposed:
600 ml (volume of water for a child weighing 20 kg) + 20 ml for each kg with a weight over 20 kg.
For children over 3-5 years old
you can use the calculation of the amount of water: 30ml / kg weight
What if the complaints disappeared during the diet, but doubts remained?
It is possible to reintroduce the allergen protein: the previous complaints have reappeared - doubts have been resolved.
Important: this should not be done in case of acute and severe allergic conditions; anaphylactic shock is possible!
But proctocolitis is not an acute, not serious condition, so the experiment is possible.
The prognosis for non-IgE conditions is usually good.
Complaints will disappear even if you do nothing at all... but it’s better not to do that!
Often, when discussing complaints from a baby, parents remember that older children also had blood in the stool in the first months of life, but then disappeared on their own. With hindsight we understand that most likely they also had allergic proctocolitis.
In most children with proctocolitis, complaints disappear before the age of one year, with FPE between the ages of 1 and 3 years, with FPIES between the ages of 1 and 5 years.
Very rarely, allergic proctocolitis persists into older age or occurs for the first time in older children or adults.
In these cases, it is very difficult to exclude a certain trigger food product; drug treatment is often required - corticosteroids, aminosalicylates. The range of conditions for a differential diagnosis by a doctor is also different.
5, total, today
Questions
- Which doctor treats anal fissure in children?
A pediatric proctologist or surgeon is involved in identifying and treating anal fissure. - Is it possible to cure anal fissure with folk remedies?
Conservative treatment of anal fissure in children is aimed at stabilizing stool and rapid healing of damaged tissue. In some cases, this effect was achieved using traditional medicine - chamomile baths, sea buckthorn suppositories and other local remedies in combination with diet. However, in any case, you must first consult with a specialist. Anal fissures are often a consequence of other proctological diseases, which can progress without adequate treatment. - Does my child need surgery for anal fissure?
In 90% of cases, if the patient seeks help in a timely manner, surgical intervention is not required. Timely initiation of conservative therapy promotes complete healing of the mucosal defect without subsequent relapses. The exception is advanced cases when dense scar tissue forms along the edges of the crack, which interferes with healing. As part of the surgical intervention, it is excised and the defect is sutured, after which standard medications are prescribed to speed up healing. - How to independently identify an anal fissure in a child?
Pain during bowel movements and red blood in the stool are sure signs of a problem. You can also examine your child's anal area yourself. In 50-60% of cases, the mucosal defect is visible without the use of additional instruments. However, such a self-diagnosis complex does not replace consultation with a specialist. Only a comprehensive examination and personalized treatment can radically solve the problem of anal fissure in childhood.
Diagnosis of anal fissure
Anal fissure is diagnosed by a pediatric proctologist or surgeon.
Even when parents first contact a doctor, a specialist may suspect the presence of this disease. The doctor pays attention to the child’s characteristic complaints, the influence of provoking factors, and the history of the development of the pathological process. A digital rectal examination is required to make a definitive diagnosis. However, in order not to cause psycho-emotional discomfort in the presence of severe pain, the doctor may first limit himself to a simple examination of the anal area. Sometimes the defect can be identified immediately.
If a rectal examination is not performed immediately, it will be postponed to the next visit. The fact is that anal fissures are often a consequence of other proctological diseases, which may not be diagnosed without a full examination. This means that the pathology of the rectum will steadily progress.
To comprehensively assess the patient’s condition, the following tests are performed:
- General blood and urine analysis. Allows you to identify concomitant diseases, primarily anemia, inflammation.
- Coprogram is a microscopic analysis of feces, which is especially important if dysfunction of other parts of the gastrointestinal tract is suspected.
- Blood chemistry. Detects metabolic changes in the body.
- Ultrasound of the abdominal organs. Detects abnormalities in the development of internal organs.
If a concomitant pathology is identified, its treatment is carried out in parallel, which helps to avoid recurrence of the anal fissure.
Treatment of anal fissure
Anal fissure in children is a disease that in the early stages of its development responds well to conservative treatment. Surgery may be indicated only if drug therapy is ineffective or the process is long-term and chronic, when a ridge of dense scar tissue forms around the crack, interfering with healing.
Conservative treatment
A key aspect of effective treatment of anal fissure in children at an early stage of the disease is the correction of diet and water balance.
This allows you to soften the stool and prevent re-traumatization of the mucous membrane. It is recommended to temporarily exclude fatty and fried foods from the diet and reduce the amount of meat consumed. It is worth increasing the amount of fruits and vegetables that are rich in fiber. Coarse fiber attracts liquid, increases the volume of stool and thereby helps normalize stool. In addition to diet correction, the proctologist prescribes the following groups of medications:
- Mild laxatives (if constipated).
- Healing ointments and creams, suppositories.
- Anti-inflammatory suppositories.
To cleanse the intestines and eliminate the local inflammatory process, it is recommended that the child take baths with chamomile decoction for 2-5 days. The water temperature is about 37°C. If a child has anemia due to minor bleeding, the doctor prescribes iron supplements, vitamin B 12, and folic acid.
Surgery
Surgical excision of anal fissure in children is performed when conservative treatment methods are ineffective.
It is indicated for the chronic form of the disease and is practiced mainly in adolescence, when the process has turned from acute to chronic. The essence of the operation is the excision of pathological scar tissue and the crack itself with further suturing of the defect. After this, the patient receives standard conservative therapy aimed at stabilizing the stool and healing the postoperative wound.