Many parents begin to worry if the mysterious abbreviation MARS (or minor anomalies of cardiac development) appears on their child’s chart. Such anomalies have always existed; these are not newly emerging diseases. From time immemorial, various abnormalities in the structure of internal organs, including the heart, have been identified - unfortunately, usually posthumously. Today, MARS is detected in children almost from birth, which allows for a fairly simple, informative and painless method of examination - cardiac ultrasound.
There is practically no popular literature about this syndrome that explains in an accessible form what it is, how dangerous it is and what to do with such a diagnosis. Close study of the syndrome began relatively recently - about 30 years ago, and many of the patterns of its development still raise a number of questions. But the occurrence of this phenomenon has increased with the development of medical technology; more precisely, the number of diagnosed cases of this pathology has increased. Now let's try to understand this problem and clarify the situation a little.
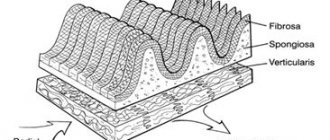
A little anatomy
The framework of all the internal organs of the child consists of special connective tissue - it is formed in utero. Connective tissue gives the organ its characteristic shape, helps it perform functions and prevents it from stretching and deforming under impacts. Connective tissue can be presented in two types - coarse fibrous, an example is cartilage, and soft fibrous - this is a kind of sponge, inside of which there are specific cells of a particular organ.
In the structure of the heart, this same connective tissue forms the valves and the heart frame itself, between the fibers of which muscle cells - cardiomyocytes - are located. Due to this, the heart tissue is elastic, but quite strong. In addition, connective tissue also forms the walls of large vessels - the aorta, pulmonary trunk, pulmonary veins and their valves (see figure). Minor cardiac anomalies (or MARS) are one of the manifestations of a condition such as dysplasia (not quite correct development) of this very connective tissue. In this condition, the connective tissue is either too weak or is formed in excess, not in the places where it should normally be. As a result, minor anatomical formations of internal organs, including the heart, appear.
Causes and mechanisms of development
Minor anomalies in the development of the heart are considered to be the presence of anatomical congenital changes in the heart and its large vessels - that is, a disorder in the structure of the heart itself that forms in the fetus. However, these changes are either insignificant or located in such a way that they do not disrupt the function of the cardiovascular system - the delivery of oxygen to the tissues.
Many MARS are temporary and disappear as the child grows - for example, due to the growth of the heart, prolapse (sagging) of the valves (MVP), pectineal muscles can be normalized, or the oval window can close, the length of the chords and the diameter of the heart vessels can be normalized. Basically, in modern conditions, MARS is detected in the vast majority of cases already in the first 2-3 years of life and has no tendency to progress.
It is believed that the development of MARS is caused by a combination of many factors. There are two large groups - external and internal factors. External factors include environmental influences, the pregnant woman’s diet, her illnesses and medications, radiation, smoking, alcohol intake, stress, etc. Internal factors include genetic, chromosomal abnormalities, and heredity.
Typically, such anomalies in the heart appear at conception (inherited), during pregnancy (congenital), and very rarely at the birth of a child.
The heart is formed in the earliest stages of intrauterine development. At about 5-6 weeks, the main division into chambers is formed and it begins to beat. Around this time and up to 10-12 weeks, the impact of various factors on the expectant mother (and many at this time still do not know about their situation) leads to anomalies. Exposure of a pregnant woman to alcohol, nicotine, toxins, poisons, heavy metal salts, viruses and bacteria in the first trimester can result in the formation of defects or minor anomalies in the development of the heart, because the placenta is still forming, and these substances can more easily penetrate to the fetus.
Congenital aortic stenosis
Cardiologists diagnose two types of narrowing of this vessel: subvalvular and valvular. The disorder is a minor congenital heart defect that occurs during fetal development.
The narrowed valve has a characteristic structure: the valve leaflets fuse together, forming a funnel with a hole directed towards the aorta.
The subvalvular narrowing has a different structure: it is a roll of muscle tissue located under the valves in the area of the left ventricle.
The clinical picture depends on the severity of the load on this part of the heart, as well as the degree of stenosis. Severe – leads to LV hypertrophy, in the final stage of the disease heart failure develops.
What are they?
There are a lot of minor anomalies in the development of the heart and sometimes they are difficult to distinguish from heart defects with minor changes in blood circulation at an early stage. Therefore, a cardiologist must decide whether they require surgical correction and whether they belong to a defect or to MARS, after a detailed examination. There are borderline conditions in which the classification of a defect into one group or another depends on the size and clinical data.
Minor anomalies are considered to be:
- Heart valve prolapse of the minimal, first degree is a state of pathological sagging, sagging of the valves due to their excessive extensibility or weakness.
- Abnormal (not in the places where it is needed) location of the chords of the heart - peculiar cartilaginous threads that give strength to the heart.
- Disturbances in the structure of special cardiac muscles - papillary muscles.
- Changed number or size of heart valves, their serration.
- Rudimentary sinus valves.
- Small-sized holes in the interatrial or interventricular septum that do not close in the first year and a half of life.
- An open oval window is small in size, up to 2-3 mm.
- A slight increase in the diameter of the outgoing vessels.
- Small aneurysms of the heart septum.
- “Fluttering” or false chords.
Patent foramen ovale
The anomaly refers to minor heart defects and is most often normal. The defect does not require treatment, except in cases where there is a pathological discharge of the shunted blood flow from the RA to the left.
The anomaly is eliminated surgically; during the operation, X-ray endovascular occlusion is performed, and the OO is closed using an occluder.
The most dangerous complication of an unoperated large foramen ovale is paradoxical embolism.
Air bubbles travel through the blood vessels to the brain, causing a stroke, so a hole that does not close for a long time and is large in size must be eliminated.
How are they detected?
Most often, MARS is detected during a routine examination by a pediatrician. Usually, the baby has a heart murmur with a generally satisfactory condition and no complaints. Usually, the doctor at the clinic limits himself to writing on the card - functional cardiopathy, which does not entirely accurately reflect the essence of the phenomena occurring with the baby. By and large, this is not a diagnosis, but simply a statement of fact - there are some minimal deviations from the norm in the heart that cannot be attributed to a specific, more serious diagnosis.
The detected phenomena do not affect the child’s condition, however, to clarify the picture, a full examination and clarification of the clinical diagnosis are required - this is necessary to develop measures for monitoring the baby and his rehabilitation. To do this, you should go to an examination by a pediatric cardiologist - a specialist in heart and vascular diseases.
The doctor will ask you questions. You will tell us how the baby eats, whether he gets tired when he sucks, whether there is any blueness, attacks of shortness of breath, how weight gain occurs. And if the baby can already talk, does he have pain in his heart, is he dizzy, is there a feeling of heartbeat, have he fainted or not?
Then he will carefully examine the baby to see if he has perioral cyanosis (blueness of the nasolabial triangle), count the heart rate and breathing to determine if there is tachycardia and shortness of breath. He will examine the tips of the fingers and nails, the shape of the chest, and percussion (tapping) the borders of the heart to determine its size. The doctor will palpate the abdomen - the area of the liver and spleen, large vessels, pulse.
Then he will begin to listen (auscultate) the heart. The first thing that is usually detected when listening to a baby’s heart is the so-called functional systolic murmur. The word “functional” indicates that the murmur is not caused by some serious heart pathology, such as a defect. The doctor will find out where the noise is coming from, what heart sounds are associated with it, and listen to the baby in front and behind.
Based on all this, he will make a conclusion whether or not the child has a circulatory disorder; with MARS, usually no changes are noted other than noise. Your examination will not end there; you will also have to undergo instrumental examination using various devices.
Let's go to research
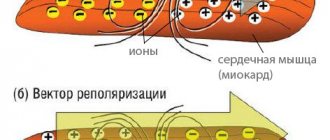
To confirm MARS in a child, it is necessary to conduct a number of studies, and the first of them will be an ECG - recording the electrical signals of the heart on a special film. This method can determine the presence of disturbances in heart rhythm, its conductivity and signs of excessive load on different parts. Typically, with MARS, all changes are minimal or do not go beyond age norms.
In addition, it is necessary to conduct a parallel study of noise, called PKG - phonocardiogram. This is a graphic reflection of pathological noise on paper, in parallel with an ECG recording. This study will allow us to differentiate functional noises from organic ones that arise from defects.
The most basic thing in diagnosing MARS is, of course, an ultrasound examination of the heart - ultrasound. This method allows you to visually see both the anomaly itself and the degree of disruption of blood flow that it causes. In addition, ultrasound is very easy to determine whether a given phenomenon relates to a defect or not.
Treatment
If a child is diagnosed with MARS in cardiology, then immediate treatment is required in order to avoid adverse consequences.
Doctors prescribe:
- balanced and proper nutrition;
- full compliance with sleep and rest patterns;
- no load;
- physical therapy classes.
Experts insist that parents completely eliminate the possibility of stress in their child. As for serious physical activities, in most frequent cases they are prohibited.
So how do MARS manifest itself?
In most cases, MARS does not manifest itself in any way, and children are no different from their peers. Less often, the main complaints of children will be intermittent pain in the heart area, arrhythmias, feelings of interruptions in the heart, and surges in blood pressure.
Often heart anomalies are combined with structural anomalies of the nervous, urinary, digestive system, vision, breathing, skeleton or skin; there may be some structural features of other organs - liver, gall bladder, kidneys.
At the beginning of the material, we said that MARS refers to connective tissue dysplasia, and connective tissue is present in all organs and systems in greater or lesser quantities. Therefore, the manifestations will be so-called systemic, that is, at the level of the entire organism. They can range from very minimal to quite pronounced.
A careful examination of the skeleton can reveal elongation of the limbs relative to the body, depression of the sternum, scoliosis (curvature) of the lower thoracic spine, various forms of flat feet, hypermobility (excessive mobility) of the joints. The most common combinations with MARS are polycystic kidney disease, gastroesophageal reflux (reflux of stomach contents into the esophagus), kinking of the gallbladder, megaureter (dilation of the ureter).
In addition, MARS is often accompanied by so-called neurovegetative disorders - the peripheral and central nervous systems work unbalanced. This can manifest itself as enuresis, speech defects, vegetative-vascular dystonia, and behavioral disorders. However, all these combinations in no case lead to severe dysfunction of organs and systems and do not worsen the overall functioning of the baby’s body.
Characteristic symptoms
Minor anomalies of heart development in children rarely appear; in most cases, the child has no complaints. In rare cases, parents may notice the following symptoms:
- pain in the heart area;
- interruptions in the functioning of the heart muscle;
- unstable blood pressure readings;
- manifestation of arrhythmia on indicators from the electrocardiogram.
In the vast majority of cases, MARS is combined with other diseases associated with the development of connective tissue. Problems may be associated with the organs of vision, skeletal body, skin, kidneys and gall bladder. Due to this circumstance, the symptoms are systemic in nature, in other words, they affect the entire body. Such manifestations can be minor or significant; each case is individual.
There are many combinations of MARS with other diseases; we cannot list them all. Let’s just try to highlight the main and most common ones.
- scoliosis, flat feet and joint hypermobility;
- gastroesophageal reflex, which is manifested by the reverse reflux of food from the stomach into the esophagus, inflection of the gallbladder and an enlarged shape of the ureter;
- neurovegetative disorders consist of unbalanced functioning of the peripheral and central nervous system.
Could there be complications?
Not always, but in some cases, MARS can be accompanied by cardiac rhythm disturbances, impulse conduction disturbances, which can manifest as minor changes in the ECG and periodic heart pain and palpitations. This requires additional examination by a cardiologist and is quite simply treated by prescribing medications that support heart function. Typically, these disorders are characteristic of mitral valve prolapse. Rhythm disturbances can result from abnormally located chords and trabeculae of the heart, an aneurysm of the interatrial septum, or an enlarged Eustachian valve.
Some MARS may be accompanied by impaired exercise tolerance; such babies have a slightly higher risk of developing infective endocarditis - inflammation of the inner lining of the heart as a complication of ARVI or other infections.
What kind of fabric is this
False left ventricular chord (LVCH) are cords of muscular-connective tissue, usually located inside the left cardiac ventricle, not connected to the valve leaflets. They were first discovered in the cavity of the human heart during autopsy in 1893. Although the author called them an anomaly, he recognized them as a possibility of the norm. A detailed classification of chords appeared already in 1970, where false ones were clearly separated from true ones. In particular, the bias was made on the location of the threads.
Over the course of many years of numerous studies, medical scientists have found that:
- about 20% of cases with the detection of atypical tissues may be accompanied by pathological changes in the functioning of the organ;
- in 19% of cases rheumatic heart disorder was observed;
- the same number of patients had atherosclerotic lesions;
- 12% of those examined were found to have mitral valve disease;
- in 5% of cases cardiomyopathy was detected;
- was present in the same number of patients.
Based on the data obtained, it was concluded that LVHL, as a result of a congenital defect, in particular cases can lead to the development of dysplastic syndrome. Disturbances in the structure of the left cardiac ventricle of this type are more common among the male population of the planet. Appearing during the embryonic development of the fetus, false threads can subsequently be transformed into additional pathways of circulation and impulse conduction. The risk of such formation is especially high when the body is intoxicated, the psycho-emotional state is unstable, and physical exertion is feasible.
Where to start therapy?
In order for MARS syndrome to manifest itself minimally or not at all, you need to choose an optimal daily routine, an appropriate load for your age and condition, alternating activities and rest. Many parents believe that a child with MARS needs to sharply limit exercise, which is fundamentally wrong. After consulting with a doctor, for the most part, you can not limit the baby’s movement at all. The heart develops correctly when it is given adequate stress. There is no need for restrictions in activity or excessive effort. If the baby expresses a desire to engage in any kind of sport, first consult with a cardiologist to see if the level of stress that sports activities will provide is possible for him. But ordinary daily activities - walking outside, cycling, running - are quite enough for proper development.
For a child with MARS syndrome, it is important to follow a daily routine, get enough sleep, eat properly, and receive all the nutrients and vitamins required by age. It is important to initially prepare yourself for long-term breastfeeding; this will help the baby get sick less and reduce the risk of heart complications at an early age to a minimum. In addition, it is necessary to introduce complementary foods into the child’s diet correctly and in a timely manner, and subsequently monitor the intake of sufficient amounts of protein foods and foods rich in calcium and magnesium.
Children who have neurological problems and are emotionally unstable benefit from working with a psychologist and sedative therapy. Physiotherapy - various baths, spa therapy, massages - also have a calming and restorative effect.
Such babies are monitored jointly by a pediatrician and a pediatric cardiologist. The timing of inspections is selected individually, depending on the type of MARS and the presence or absence of associated violations. Usually, for most children, non-drug measures or infrequent courses of cardiotrophic (supporting the proper functioning of the heart) drugs are sufficient.
Only isolated cases of MARS may require surgical correction. In such cases, the baby will be referred to a cardiac surgeon to decide on the volume and timing of the operation. There is no need to be afraid of this - open heart surgery is very rarely performed for MARS. Usually these are so-called endoscopic operations - an instrument is inserted into the heart cavity through small punctures or through large vessels and the defect is corrected. Usually, babies stay in the clinic for a short time and after discharge they lead the lifestyle of ordinary children.
What if you need pills?
Sometimes there are situations when the doctor will recommend a course of certain medications. The main therapeutic effects are magnesium preparations. This trace element is a component of connective tissue and therefore improves its structure and heart function. The choice of magnesium preparations depends on the age of the patient. There are liquid and tablet forms. Particularly popular are “Magnerot” - in addition it also contains orotic acid, which promotes the absorption and more complete absorption of magnesium, “Magne B6” in the form of syrup or tablets, and “Potassium Orotate”. Usually 1-2 courses per year are recommended.
The second direction of therapy is cardiotrophic - nourishing the heart muscle. These are drugs that improve blood supply and nutrition to the tissue of the heart and other organs, affect metabolism in the body and are active antioxidants. Usually prescribed are “Elkar”, “Ubiquinone” or “Coenzyme Q10”, “Kudesan”, “Cyto-mac”. In addition to these drugs, some vitamins have a similar effect - PP, B2, B1, citric and succinic acids (the drug "Limontar"), biotin. They are prescribed as a multivitamin complex or each separately in courses of 10-14 days twice a year.
In case of infections, the baby is recommended to take preventive courses of antibiotic therapy to prevent heart complications such as endocarditis.
Regular examinations by an ENT specialist and a dentist are indicated to sanitize foci of chronic infection - carious teeth, tonsils, adenoids.
In the presence of arrhythmias, antiarrhythmic therapy is indicated, but it is selected individually in the hospital under the supervision of a physician.
Courses of sedatives are conducted that normalize the functioning of the nervous system, relieve anxiety, increased nervous excitability and treat neuroses.
A little about specific types
The most well-known and common MARS is mitral valve prolapse . This is the sagging of the bicuspid valve at the moment of contraction (systole) of the heart into the cavity of the left ventricle, due to which a slight turbulence of the blood flow in the heart occurs. This turbulence produces systolic murmurs, which the doctor can hear with a phonendoscope. Only the first degree of prolapse is classified as MARS. All other degrees are accompanied by severe circulatory disorders and should be considered heart defects.
Mitral valve prolapse is usually detected by ultrasound or when visiting a doctor with complaints of intermittent pain in the heart. Typically, such babies have periodic heartbeats, poor tolerance to active physical activity, fatigue, asthenia, dizziness, and psycho-emotional instability. Such children have difficulty adapting to a team; they are constrained, shy, and whiny.
False chords in the left ventricle are quite common . This is MARS, which manifests itself in the presence inside the ventricular cavity of additional strands of connective tissue or muscles attached to the walls of the ventricle or interventricular septum. Normally, they should be attached to the leaflets of the atrioventricular valve. This is more often found in boys; false chords can be single or multiple, occurring both separately and in combination with other anomalies. Their location can be along the blood flow, across it or diagonally - the severity of the murmur in the heart will depend on this.
These chords can cause cardiac arrhythmias, so patients require special monitoring by a cardiologist.
The third common MARS is patent foramen ovale (PFO) . A variant of the norm is the presence of a minor defect of up to 2-3 mm under the age of one year. Usually after this age the window closes on its own. But when it is present at an older age, in some cases we are talking about a developmental anomaly (when the size of the defect is up to 5 mm), in others – about a heart defect (when the defect is pronounced and there is a circulatory disorder).
OOO is manifested by pronounced psycho-emotional instability - children are capricious, whiny, they do not adapt well to the team. Babies do not tolerate intense stress well, get tired quickly, they may experience dizziness, interruptions in heart function, and occasionally pain in the heart. On examination, a heart murmur is noted. The diagnosis is usually confirmed by ultrasound.
Symptoms
Mitral heart defects: types, causes, diagnosis and treatment
In most cases, the additional chord of the left ventricle does not bear any functional load on the heart and does not interfere with its normal functioning. For many years, this minor anomaly may not be detected, because it is not accompanied by any special symptoms. A pediatrician can listen to a systolic heart murmur in a newborn, which is detected between the third and fourth ribs to the left of the sternum and does not in any way affect the functioning of the heart.
During intensive development, when the rapid growth of the musculoskeletal system significantly outstrips the growth rate of internal organs, the load on the heart increases, and the additional chord may make itself felt for the first time. Your child may experience the following symptoms:
- dizziness;
- rapid or unmotivated fatigue;
- psycho-emotional lability;
- cardiopalmus;
The same clinical manifestations can be observed with multiple abnormal chords of the left ventricle. Most often, such symptoms appear during adolescence. In the future, they can completely disappear on their own, but sometimes they remain in adulthood.
When symptoms appear, the child must be prescribed ECHO-CG, ECG, etc. These studies will allow the doctor to determine the presence or absence of hemodynamic disturbances. If the additional chord is “hemodynamically insignificant,” then the anomaly is considered safe, and the child only requires follow-up with a cardiologist. With a “hemodynamically significant” diagnosis, the patient is advised to observe, adhere to certain restrictions and, if necessary, treatment.
Summarize
MARS syndrome is not a death sentence, it is a special condition of the child that requires only observation and minor correction. For mothers and fathers, the presence of such a diagnosis is not a reason to limit the child and panic, it is just a reason to change their lifestyle, adjusting it to the capabilities of the baby. Most MARS do not cause any harm to the baby, and his life is no different from his peers. There is no need to treat such a child as a sick person, much less a disabled person - this is groundless. The main thing that parents need to remember is the doctor’s conclusion: “no hemodynamic disturbances are detected.” This suggests that MARS does not interfere with the baby in any way.
Diagnostics
Aortic heart defects: causes, diagnosis and treatment
There are few advanced methods for diagnosing LVHL. Ultrasound examination allows you to see, and echocardiography allows you to hear and monitor whether the LVE chord is interfering with the functioning of the organ. The Doppler diagnostic method is used to measure the size, determine the density and nature of LVHL.
For a newborn baby 1 month old, only echocardiography is applicable, since it is still difficult to see anything in the cavity of the heart, much less measure it. Note that for a child, detection of LVHL is much more typical than for an adult. With proper growth and development of the baby, the anomalies can eliminate themselves.
For an atypical chord, the standard formulation of the examination results is (minor anomaly of cardiac development).