What kind of care is provided to a patient in intensive care?
A patient diagnosed by an ambulance with acute coronary syndrome is immediately taken to the intensive care unit.
Often, large cardiology clinics have separate specialized infarction intensive care units. Resuscitation during a heart attack primarily consists of providing the damaged heart muscle with oxygen, stopping the developed life-threatening arrhythmias, and correcting hemodynamic disorders and thrombus formation.
To do this, the following procedures are used:
- oxygen therapy - the patient is connected to a ventilator to combat hypoxia;
- infusion therapy - indicated to restore normal blood supply to tissues, water and electrolyte balance, and is used to provide parenteral (intravenous) nutrition;
- sedation – during a heart attack it is very important to calm the patient’s nervous system, for which appropriate medications are used;
- pain relief – ischemia of the heart muscle is accompanied by intense pain, which can lead to the development of shock, so it is relieved with the help of narcotic analgesics;
- prevention of thrombus formation or dissolution of a formed thrombus - it is very important to prevent a recurrent attack or to ensure access of oxygen to the ischemic area, for which anticoagulants such as heparin or warfarin are prescribed;
- strict bed rest is necessary to minimize physical activity and restore the body.
While in intensive care, the patient can be treated surgically:
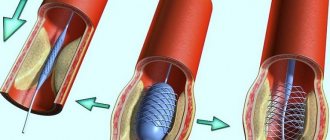
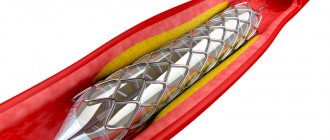
stenting of coronary arteries;- coronary artery bypass grafting;
- laser angioplasty;
- balloon dilatation of coronary vessels.
Patients are in intensive care after a heart attack under constant supervision of medical personnel. They are connected to equipment around the clock, which automatically takes an ECG, monitors blood pressure, respiration, heartbeat and other indicators. If the patient develops clinical death, he is urgently given cardiopulmonary resuscitation, which consists of the following actions:
- indirect cardiac massage;
- artificial ventilation;
- defibrillation;
- drug support for the patient.
Heart attacks are no joke
Prolonged chest pain is a serious reason to consult a doctor
Heart attack is a word with a scary connotation. We often think of it as something far away. Something that happens to others, but will never happen to you or those close to you. Unfortunately, this detachment and unwillingness to delve into the essence of the problem can sometimes be fatal.
Heart disease is the main reason why Ugra residents die or become disabled. Unfortunately, not everyone knows its symptoms and does not contact doctors at the right time.
Chest pain is serious
Myocardial infarction is an emergency condition most often caused by coronary artery thrombosis. Most often it affects people suffering from a lack of physical activity against the background of psycho-emotional overload. But it can also affect people with good physical fitness, even young people. Although the likelihood of developing a heart attack in people leading a sedentary lifestyle is several times greater than in people who are physically active. Most often, myocardial infarction occurs in men aged 45 to 65 years and women over 55 years of age.
The main reasons contributing to the occurrence of myocardial infarction are: overeating, unhealthy diet, excess animal fats in food, insufficient physical activity, hypertension, bad habits.
The heart is often thought of as a pump that pumps blood through itself. But the heart muscle itself is supplied with oxygen through blood vessels that approach it from the outside. As a result of various reasons, some part of these vessels is affected by atherosclerosis and can no longer pass enough blood. Coronary heart disease occurs. During a myocardial infarction, the blood supply to part of the heart muscle stops suddenly and completely due to complete blockage of the coronary artery. This is usually caused by the development of a blood clot on an atherosclerotic plaque, or less commonly by a spasm of the coronary artery. A section of the heart muscle that is deprived of nutrition dies.
“Symptoms of myocardial infarction are pressing, squeezing or burning pain behind the sternum, which can radiate under the shoulder blade, into the left arm, into the left shoulder, into the epigastric region (pain in the pit of the stomach) and even into the lower jaw.
Heart pain radiates through the plexus of nerve endings to the lower jaw. It feels like absolutely all the teeth in the lower jaw are hurting. There may also be numbness in the left arm. If this pain lasts longer than twenty minutes, then this indicates that the person has a prolonged anginal attack and the development of myocardial infarction is possible,” says Maria FRANZ , a cardiologist of the first qualification category of the cardiac surgery department of the District Clinical Hospital of Khanty-Mansiysk.
To the ambulance - without hesitation!
In addition to pain, a person may feel short of breath, experience weakness and sweating. If the heart does not have enough oxygen, this means that the vessel is clogged, blood does not flow into the heart muscle, and therefore the contractility of the heart muscle decreases. The amount of oxygenated blood decreases. As a result, a person feels as if he is short of air.
With the symptoms of a heart attack, if you feel them for the first time in your life, the main thing is not to panic. You need to chew 250 milligrams of aspirin - that's half a tablet. Place nitroglycerin under your tongue or take Isoket. Next, call an ambulance immediately!
At the Khanty-Mansiysk Regional Clinical Hospital, the patient immediately undergoes emergency coronary angiography - an examination of the blood vessels of the heart. The patient goes from the emergency room to the X-ray surgery department, where doctors look at the patency of the coronary arteries, looking for blood clots that close the vessels of the heart, interfering with normal blood flow.
Next, doctors perform coronary angioplasty to restore normal blood circulation. The prognosis after such an intervention is usually favorable: a heart attack is certainly not a death sentence or a disability. “The sooner we start working with the patient, the better for him and his health. It will be possible to avoid many complications caused by a heart attack. And soon there is a very high probability of returning to normal life,” says the cardiologist.
"Golden" 90 minutes
If you feel symptoms similar to those voiced in this article, call an ambulance without hesitation! It’s better to make a mistake than to suffer a heart attack on your feet.
In Khanty-Mansiysk, about 150-160 heart attacks occur per year. Unfortunately, some patients do not call an ambulance, thinking that the cause of the pain is, say, heartburn. The fact is that the heart is located close to the stomach; they are separated only by the diaphragm. If a heart attack develops along the back wall of the heart, the one that is directed towards the stomach, then the person will experience pain in the stomach during a heart attack. Pain impulses from the heart travel to the spinal cord and then to the head. Due to the close proximity of the heart and stomach, the brain often cannot distinguish which of these two organs the pain signal comes from.
But the time from the moment a symptom occurs to the moment medical care is provided is very important. “Often a patient comes to our cardiac surgery department who has already had a heart attack. We see this with electrocardiography. We see scars - zones of impaired contractility of the heart. In this case, the patient does not even know that he suffered a heart attack. But this does not mean at all that everything has passed without a trace for the body: The consequence may be a decrease in cardiac contractility and the development of heart failure. Or an aneurysm of the left ventricle of the heart, which requires more complex intervention. And there are situations when medicine is powerless - the consequences are so serious, says Maria Franz.
From the time the patient reaches the doctors until normal blood flow in the coronary artery is restored by medical means, no more than 90 minutes should pass. Ideally, a person should get to the hospital within the first hour, which doctors call the “golden hour.” The sooner the necessary measures are taken, the less damage will be caused to health, and the smaller the area affected by a heart attack. In other cases, it is possible to help the patient so quickly that a heart attack may not develop, doctors say.
Take care of your heart
In conclusion, I would just like to remind you that health is a priceless gift that should be valued and protected. Doing this is not so difficult, and with the advent of the habit of a healthy lifestyle, taking care of your body will begin to bring joy. Don’t “deprive” yourself of physical activity, eat right, give up cigarettes. And smile more often: a positive emotional attitude can also be safely attributed to the prevention of cardiovascular diseases.
Ilya Yurukin,
public relations editor
article from the site https://cmphmao.ru/node/30146
Length of patient's stay in intensive care after a heart attack
In modern medicine, they try to reduce the time a patient spends in a hospital in order to optimize costs and reduce prices for treatment. If previously a patient with a heart attack could stay in the hospital for almost a whole month, now this period has been significantly reduced.
With an uncomplicated course of the disease, the patient remains in intensive care for an average of three days. During this time, a full standard examination is carried out, vital signs are stabilized and appropriate treatment is prescribed. In most cases, surgical intervention becomes necessary. In such a situation, the duration of the patient's stay in the intensive care unit is supplemented by the pre- and postoperative period. But the total period usually does not exceed 7-10 days.
After this, the patient is transferred to a cardiology hospital or discharged home.
What determines the length of a person's stay in the intensive care unit?
The length of time a patient is kept in intensive care after a heart attack is determined by the following factors:
- localization and size of ischemic necrosis;
- the presence of complications (shock, reperfusion syndrome, coma);
- the presence of concomitant diseases (hypertension, diabetes mellitus);
- the age of the patient and his general condition;
- volume of surgical intervention.
The combination of these circumstances creates a wide time frame: some are discharged within a week, others are kept for a month or more. It is necessary to understand that patients with coronary artery disease are always at high risk of recurrent heart attacks, therefore you should strictly follow the doctor’s instructions and not stop the treatment process ahead of time.
A person is discharged if the following criteria are met:
- restoration of normal heart rhythm;
- absence of life-threatening complications;
- absence of disturbances of consciousness.
As well as the length of hospital stay, the time spent in bed rest after discharge was significantly reduced. It was found that a long stay in a supine position increases the risk of complications such as thrombosis, embolism, and bedsores. In most cases, patients can begin to walk fully within 3-4 weeks of the acute episode.
After discharge, the rehabilitation stage begins, which lasts several months (up to a year) and plays a very important role in the further prognosis for the patient.
Behind the doors of the intensive care unit: “there is a struggle for life there”
Reanimation and intensive care units, according to many, have long been a “closed” area to the public, which constantly caused public outcry.
Now the situation has changed, and the issue of admitting relatives has been resolved at the legislative level .
However, intensive care remains a special department where patients are on the verge of life and death.
Anesthesiologist-resuscitator, head of the department of resuscitation and intensive care for burn injuries, head of the anesthesiology and resuscitation service of the Novosibirsk Regional Hospital Igor Samatov spoke about the specifics of the work of intensive care units, the peculiarities of patient management and visiting rules.
– Igor Yuryevich, how does the intensive care unit differ from all others? What are the indications for hospitalization of patients in the intensive care unit?
– The intensive care unit differs from all others in that the patient is admitted to this department if his life is in danger as a result of illness, injury or accident. This occurs when body functions are lost, partially or completely. We call this condition multiple organ failure syndrome. And the task of an anesthesiologist-resuscitator is to provide prosthetics for impaired or lost vital functions, up to their direct replacement. For example, we replace the function of external respiration using artificial pulmonary ventilation, and replace renal function in case of renal failure by carrying out renal replacement therapy in various options - hemodialysis, hemofiltration, hemodiafiltration.
Removing from a state of shock and combating other critical conditions is the task of a resuscitator. For this purpose, intensive therapy is carried out, which is reflected in the name of the department. Monitoring of vital functions, drug therapy, correction of water-electrolyte and metabolic disorders can be carried out over a period of hours, days, weeks. Many drugs, for example, to maintain vascular tone and ensure cardiac output, are administered continuously through special devices - syringe dispensers (infusion pumps), artificial parenteral nutrition is carried out using volumetric dispensers.
Accordingly, the indications for placing patients in intensive care units are the threat of loss or the already occurring loss of vital body functions during the development of any critical condition.
There is also such a thing as intensive surveillance. It may be required, for example, in the postoperative period after major operations.
– What equipment should the intensive care unit be equipped with?
– The resuscitation and intensive care units are equipped with modern technological equipment in accordance with the currently existing procedures for providing medical care in the “anesthesiology-reanimatology” profile (such procedures exist for both adults and children).
Each intensive care bed is equipped with a life support system: a supply of necessary gases, electricity, a breathing apparatus, a monitor that provides constant monitoring of vital functions, drug dispensers, patient heating devices, a defibrillator and many other complex equipment.
– Are there “specialized” intensive care units?
- Yes, sure. For example, in the Regional Clinical Hospital, the anesthesiology and resuscitation service includes nine structural units, of which seven are specialized intensive care and intensive care units (surgical, purulent-septic, burn, therapeutic, obstetric, pediatric and neonatal), as well as an anesthesiology department - intensive care unit and blood transfusion department, gravitational surgery and hemodialysis.
– Which doctor is considered the attending physician of a patient in the intensive care unit?
– Any patient who is in the ICU has two attending physicians. One attending physician - always according to the profile of the underlying disease, for example, a surgeon (vascular, thoracic, abdominal, and so on), a therapist (cardiologist, neurologist, pulmonologist, etc.), obstetrician-gynecologist, pediatrician, neonatologist... And the second attending physician is a doctor anesthesiologist-resuscitator. Additionally, if necessary, consultant doctors of other specialties may be involved.
– Often, a doctor, when communicating with relatives, characterizes the patient’s condition in intensive care as “stable, severe,” “extremely severe.” What do these terms mean?
– To objectively assess the severity of a patient’s condition in intensive care, there are various scales and indices; they are necessary in everyday clinical practice. But in simple language the above terms are quite usable. The most important semantic load in this case falls on the word “stable”.
The fact is that the condition of a patient in intensive care cannot, by definition, be easy. The patient is placed in the intensive care unit only for absolute reasons, when his condition is really serious or extremely serious. If it is said that the condition is stable and serious, this is good. Stable in this case means that the resuscitator controls the clinical situation.
Of course, the patient’s recovery is still far away, but changes in the condition are predictable, correction of disorders and prosthetics of lost body functions are completely under control. It’s worse when multiple organ failure syndrome progresses despite intensive therapy - then we can talk about an unstable condition and progression of negative dynamics.
It happens that patients are in serious condition for a long time, and relatives do not understand why it lasts so long. For example, burn patients or septic patients. Treatment can last weeks, sometimes months, and while the patient’s condition is serious, he will be in intensive care. In such a situation, most questions are resolved after a visit to the patient by relatives and a detailed personal conversation with the doctor. We cannot provide information over the phone; this is a reasonable legal restriction.
– Please explain what a medically induced coma is.
– Sometimes intensive therapy is accompanied by immersing the patient in a state of medicated sleep; this is an important component of intensive care. The patient must “sleep through” the critical condition. The fact is that, being in a critical condition, the patient is simply “burning” and it is very important to lower the metabolic rate in order to preserve the body’s reserves and resources.
– Can the patient or his relatives refuse resuscitation?
– Neither the patient himself nor his relatives can refuse resuscitation measures. In our country, the patient’s right to euthanasia is not prescribed by law. From my point of view, this is correct. We always fight for the patient's life to the last.
– Under what conditions is a patient transferred from the intensive care unit?
– The patient is transferred from the ICU to a specialized department when a state of clinical stability is achieved, when there is no need for round-the-clock intensive monitoring of the patient’s condition. This always happens in agreement with the attending physician and the head of the specialized department.
– How much does it cost, on average, for a patient to stay in intensive care? From what sources is it financed?
– A patient’s stay in the intensive care unit is very expensive. All over the world, intensive care units are, by definition, unprofitable. Modern intensive care technologies are financially expensive, and our country and our hospital are no exception. And despite this, the patient is treated as much as necessary. There are no rules regulating the maximum stay in the ICU, and there cannot be. The main source of financing is compulsory health insurance and the state guarantee program.
– What is the procedure for visiting patients in intensive care today? What could be the reasons for refusal?
– We have an internal order “On the rules for visiting a patient in the ICU.” This order regulates visiting hours and a number of other important points, in particular, a ban on photography and video recording, and the requirement to turn off all electronic devices. The degree of relationship is necessarily the first line, that is, husband, wife, children, parents. Visitors who are not close relatives are admitted only if accompanied by them. Visiting conscious patients is possible only with their consent. The visiting rules in the form of a memo are posted on the information stand in front of the entrance to each intensive care unit, as well as on the hospital’s external website.
The reasons for refusal are also regulated. In particular, the presence of an acute infectious disease, most often ARVI. And this, first of all, is in the interests of patients, since many of them have weakened immune systems. Visitors in a state of alcoholic or other intoxication, children under the age of 14 are not allowed.
In addition, if invasive procedures or resuscitation measures are being performed in the ward, at this time, of course, a visit is temporarily not possible. In this situation, relatives who were already in the intensive care unit may be asked to urgently leave the intensive care unit, which should be taken with understanding and adequately. After reading the “Visiting Rules,” the visitor signs and the document is saved in the medical history.
The main thing when visiting the intensive care unit is to understand that there is a minute-by-minute struggle for life, doctors and nurses are doing their far from simple work, and it is necessary to understand the peculiarities of the work of this intensive care unit.
Duration of sick leave for myocardial infarction
After discharge, the patient is given a sick leave, which is drawn up by the attending physician. If it is necessary to extend its validity, a special medical commission is appointed. The specific duration of sick leave for incapacity for work after a heart attack depends on the severity of the pathology:
- small focal infarction without complications – 60 days;
- extensive large-focal and transmural – 60-90 days;
- complicated heart attack – 3-4 months.
If the following conditions are present, the patient is referred to a medical and rehabilitation expert commission to determine the fact of permanent disability:
- repeated (recurrent) heart attack;
- the presence of severe heart rhythm disturbances;
- chronic heart failure.
The commission determines the severity of the patient's condition and assigns him to one of the functional classes. Depending on the class, doctors decide the future fate of the patient - extend his sick leave, or give him a disability group.
There are four functional classes:
- I – ability to work is preserved, but patients are removed from night shifts, additional workloads, and business trips. In this case, it is recommended to change heavy physical work to lighter work;
- II – only light work is allowed, without significant physical exertion;
- III – patients are recognized as disabled if their activities are associated with physical work or psycho-emotional stress;
- IV – patients are considered absolutely unable to work, they are given a disability group.
Further rehabilitation
A heart attack is not a diagnosis, but a way of life. After the patient leaves the hospital bed, he will have a long period of rehabilitation, during which he will restore his health and performance.
A specific program is prescribed by a cardiologist and physiotherapist. In addition to drug therapy, it includes:
- Spa treatment;
- physical therapy – in accordance with the functional class of the disease;
- dieting and weight control - avoidance of flour and fatty foods, split meals;
- quitting smoking and alcohol, which can significantly reduce the risk of relapse;
- avoiding stress, including psychological training or meditation;
- constant independent monitoring of blood pressure and pulse.
It is also necessary to periodically undergo preventive examinations according to the following scheme:
- first month - every week;
- the first six months - once every two weeks;
- the next six months - once a month;
- in the future – once a quarter.
Rubric “Conversation with a specialist” Acute myocardial infarction - symptoms and first aid
The joint article was prepared by three specialists at once - cardiologist, anesthesiologist-resuscitator of Health Academy LLC Konstantin Nikolaevich Bozhesku, functional diagnostics specialist of Health Academy LLC (formerly an employee of the Nizhny Tagil emergency medical service team), Gennady Andreevich Puzanov and paramedic of the highest category of the team intensive care of the State Budgetary Healthcare Institution SO "City Emergency Medical Care Station of Nizhny Tagil" by Dmitry Vasilievich Subbotin.
Timely pre-medical and emergency medical care during an attack of myocardial infarction in most cases is the key to the patient’s successful recovery. It is the absence of such activities that often becomes the cause of death even for young people who have encountered this acute cardiac pathology. Cardiologists recommend that all patients with coronary artery disease know the first signs of myocardial infarction and the rules for providing first aid. It is also important to know what treatment the patient will be prescribed in the hospital in order to prepare for a conversation with the attending physician and ask him the necessary and important questions.
When is it necessary to start performing first aid? The answer to this question is always clear – immediately. That is, already when the patient began to show the first signs of myocardial infarction. Its onset is signaled by the following typical symptoms:
intense chest pain; irradiation of pain to the left arm, shoulder blade, teeth or neck area; severe weakness; fear of death and severe anxiety; cold clammy sweat; nausea. With atypical forms of heart attack, the patient may experience other symptoms:
stomach ache; digestive disorders; vomit; dyspnea; suffocation, etc. First aid in such situations should begin with calling an ambulance. When talking with the dispatcher of this service, you must:
report the symptoms observed in the patient; express your assumption about the possibility of myocardial infarction; ask to send a team of cardiologists or resuscitators. After this, you can begin to carry out those activities that can be performed outside the medical institution.
First aid The patient must be carefully placed on his back and given the most comfortable position (semi-sitting or a cushion placed under the back of his head).
Ensure a flow of fresh air and the most comfortable temperature conditions. Remove clothing that interferes with free breathing (tie, belt, etc.).
Convince the patient to remain calm (especially if the patient exhibits signs of motor agitation). Talk to the victim in a calm and even tone, do not panic or make sudden movements.
Give the patient a Nitroglycerin tablet under the tongue and a sedative (Corvalol, motherwort tincture or valerian).
Measure blood pressure. If the pressure is not more than 130 mm. rt. Art., then it is advisable to re-take Nitroglycerin every five minutes. Before the doctors arrive, you can give 2-3 tablets of this drug. If the first dose of Nitroglycerin caused a severe throbbing headache, then the dosage should be reduced to ½ tablet. When using this drug in the form of a spray, its single dose should be 0.4 mg. If the patient's first dose of Nitroglycerin caused a sharp decrease in blood pressure, then this drug should not be used further.
Give the patient a crushed Aspirin tablet (to thin the blood).
Count the patient's pulse. If the heart rate is no more than 70 beats/minute and the patient does not suffer from bronchial asthma, then he can be given one of the beta blockers (for example, Atenolol 25-50 mg).
You can put a mustard plaster on the area where the pain is located (remember to keep an eye on it so that there is no burn).
During the provision of first aid, the patient’s condition may be complicated by the following conditions:
fainting; heart failure. If fainting occurs, it is necessary to remain calm and ensure the normal functioning of the respiratory system. The patient must be placed in a horizontal position, a cushion placed under his shoulders and dentures (if any) removed from the mouth. The patient's head should be in a tilted position, and if there are signs of vomiting, it should be turned to the side.
In case of cardiac arrest, artificial respiration and chest compressions must be performed before the medical team arrives. The frequency of compressions on the midline of the chest (heart area) should be 75-80 per minute, and the frequency of blowing air into the airways (mouth or nose) should be about 2 breaths every 30 compressions on the chest.
Emergency medical care and principles of treatment in a hospital Emergency medical care for myocardial infarction begins with the relief of acute pain. For this, various analgesics (Analgin) and narcotic drugs (Promedol, Morphine, Omnopon) in combination with Atropine and antihistamines (Diphenhydramine, Pipolfen, etc.) can be used. For a faster effect, painkillers are administered intravenously. Seduxen or Relanium is also used to eliminate the patient's anxiety.
Then, to assess the severity of the heart attack, the patient is given an electrocardiogram. If hospitalization is possible within half an hour, the patient is immediately transported to a medical facility. If it is impossible to transport the patient to the hospital within 30 minutes, thrombolytics (Alteplase, Purolase, Tenecteplase) are administered to restore coronary blood flow.
A stretcher is used to transfer the patient to the ambulance, and during transportation to the intensive care unit, humidified oxygen is inhaled. All these measures are aimed at reducing the load on the heart muscle and preventing complications.
After arrival at the intensive care unit, to eliminate pain and agitation, the patient is given neuroleptanalgesia with Talamonal or a mixture of Fentanyl and Droperidol. In case of a prolonged angioedema attack, the patient can be given inhalation anesthesia using a gaseous mixture of nitrous oxide and oxygen.
Next, the patient is prescribed the following medications:
Nitroglycerin, Isosorbide dinitrate, Isoket - in the acute period of a heart attack, these drugs are used to reduce the myocardial oxygen demand, first they are administered intravenously, and after stabilizing the patient's condition - orally and sublingually.
Beta blockers (Anaprilin, Inderal, Obzidan, Propranolol) - help slow the heart rate and reduce the load on the heart.
Antiplatelet agents (Aspirin) thin the blood and prevent the development of a new heart attack.
Anticoagulants (Heparin) - used to prevent recurrent heart attacks and reduce blood clotting.
ACE inhibitors (Ramipril, Captopril, Enalapril, etc.) are used to lower blood pressure and reduce the load on the heart.
Sedative and hypnotic drugs (Diazepam, Oxazepam, Triazolam, Temazepam, etc.) are used when it is necessary to limit the patient’s activity and for sleep disorders.
Antiarrhythmic drugs (Novocainamide, Rytmilen, Lidocaine, Difenin, Amiodarone, etc.) are used for cardiac arrhythmias to stabilize cardiac activity and reduce the load on the myocardium.
Other pharmacological drugs can be used to treat myocardial infarction, since the tactics of drug treatment of the patient depends on the general condition of the patient and the presence of other pathologies (diseases of the kidneys, blood vessels, liver, etc.).
Also, for the treatment of myocardial infarction, modern medicine uses various instrumental, highly effective techniques to restore coronary blood flow:
balloon angioplasty; coronary artery bypass grafting. Such surgical techniques allow patients with severe forms of myocardial infarction to avoid serious complications and prevent the high risk of mortality from this cardiac pathology.
Motor activity of a patient with myocardial infarction All patients with myocardial infarction are advised to limit their physical activity, since this regime contributes to a more rapid replacement of the infarction area with scar tissue. In the first days, the patient must observe strict bed rest, and from 2-3 days, in the absence of complications and signs of heart failure, his motor regimen begins to gradually expand. Initially, he is allowed to sit on a bedside chair 1-2 times a day and sit on it for about 15-30 minutes (the frequency and duration of these actions is determined by the doctor).
These days the patient can eat on his own. He also needs to be washed and cleaned, and he must use a bedpan to defecate (the use of a bedside toilet seat is permissible only with the permission of a doctor and only for patients with a stable heart rhythm).
Starting from 3-4 days, the patient is allowed to sit on a chair for about 30-60 minutes twice a day. In case of an uncomplicated heart attack, the patient is allowed to start walking between 3-5 days (this time is determined by the doctor). The time of such walking and the distances over which the patient moves increase gradually.
In an uncomplicated form of myocardial infarction, the patient is discharged from the hospital on days 7-12, and in complicated cases it can take place only after 3 weeks or more. In the future, the patient must undergo a course of rehabilitation, which can be performed in specialized institutions or at home. During this period, the intensity and duration of physical activity gradually increases depending on health indicators.
Nutrition of the patient during myocardial infarction In the first week after myocardial infarction, the patient is recommended to have a low-calorie diet with limited salt, animal fats, liquids, foods with nitrogenous substances, excessively coarse fiber and cholesterol. The diet should include foods that are rich in lipotropic substances, vitamin C and potassium salts.
In the first 7-8 days, all dishes should be pureed. Food is taken in small portions 6-7 times a day.
The diet may include the following foods and dishes:
wheat bread crackers; semolina, oatmeal, buckwheat and rice cereals; lean veal; low-fat varieties of fish; chicken meat; protein steam omelette; low-fat cheese; fermented milk drinks; butter; salad of fresh grated carrots and apples; vegetable soups; boiled beets and cauliflower; pureed fruit; compotes and fruit drinks; rosehip decoction; weak tea; honey. During this period, the following foods and dishes are prohibited:
dough products (pancakes, donuts, cakes, pies); smoked and marinated dishes; pickles; fried foods; sausages; fatty dairy products; salty and spicy cheeses; caviar; fat meat; boiled and fried eggs; fish and mushroom broths; pasta; cooking fat; mushrooms; legumes; sorrel; turnip; grape; tomato juice; spices; chocolate; natural coffe. 2-3 weeks after a heart attack, the patient is recommended the same set of products and list of restrictions, but the food may no longer be pureed, prepared without adding salt and taken about 5 times a day. Subsequently, the patient's diet expands.
Remember! Myocardial infarction is a serious and dangerous pathology that can cause many serious complications and even death of the patient. Be sure to follow all the rules for providing first aid during an attack of this acute condition, call an ambulance in a timely manner and follow all the doctor’s recommendations during treatment in a hospital.
You can make an appointment with a cardiologist, as well as undergo an electrocardiogram at our Medical Center. Make an appointment by phone 8(3435) 230-500
We care about you!
Always yours, Medical
conclusions
Myocardial infarction is a dangerous emergency condition that requires emergency measures to save life. The earlier resuscitation measures are started, the greater the chances of a successful recovery.
During the first three to seven days, the patient is placed in the anesthesiology and intensive care unit, where there are all the necessary conditions for maintaining life and treating the early stages of a heart attack. Subsequently, the patient is transferred to a cardiology hospital. The timing of discharge from the intensive care unit depends on the specific situation. The duration of sick leave also varies according to the severity of each individual patient.
The problem of lung damage during a viral infection caused by COVID-19 is a challenge for the entire medical community, and especially for anesthesiologists and resuscitators. This is due to the fact that patients in need of resuscitation due to developing respiratory failure have a number of specific characteristics. Patients admitted to the ICU with severe respiratory failure, usually over 65 years of age, suffer from concomitant somatic pathology (diabetes, coronary heart disease, cerebrovascular disease, neurological pathology, hypertension, oncological diseases, hematological diseases, chronic viral diseases, disorders in the blood clotting). All these factors indicate that patients admitted to the intensive care unit according to indications belong to the category of severe or extremely severe patients. In fact, such patients have mild to severe ARDS.
In patients with respiratory failure, it is customary to use respiratory therapy. Currently, there are many options for respiratory therapy: oxygen inhalation (low flow - up to 15 l/min, high flow - up to 60 l/min), artificial ventilation (non-invasive - NIMVL or invasive mechanical ventilation, high-frequency ventilation).
In the treatment of classic ARDS, it is customary to use a stepwise approach to the choice of respiratory therapy. A simple scheme is as follows: low-flow oxygen therapy - high-flow oxygen therapy or NIMVL - invasive mechanical ventilation. The choice of a particular respiratory therapy method is based on the severity of ARDS. There are many validated scales for assessing the severity of ARDS. In our opinion, the “Berlin definition of ARDS” can be considered convenient and applicable in clinical practice.
Global practice indicates an extremely high percentage of deaths associated with a viral infection caused by COVID-19 when using invasive mechanical ventilation (up to 85-90%). In our opinion, this fact is associated not with the method of artificial ventilation itself, but with the extremely serious condition of the patients and the characteristics of the course of the COVID-19 disease.
The severity of patients undergoing invasive mechanical ventilation is due to the large volume of damage to the lung tissue (usually more than 75%), as well as the resulting superinfection during prolonged artificial ventilation.
Our own experience shows that the process of repair of lung tissue during COVID occurs by the 10-14th day of the disease. This is associated with the need for long-term artificial ventilation. In anesthesiology and resuscitation, one of the criteria for transferring to spontaneous breathing and extubation is the persistent maintenance of an oxygenation index of more than 200 mm Hg. Art. provided that low values of PEEP are used (no more than 5-6 cm water column), low values of maintenance inspiratory pressure (no more than 15 cm water column), stable indicators of lung tissue compliance are maintained (static compliance more than 50 ml/mbar), there is sufficient inspiratory effort of the patient ( p 0.1 more than 2.)
Achieving adequate parameters of gas exchange, pulmonary mechanics and adequate spontaneous breathing is a difficult task, given the limited respiratory surface of the lungs.
At the same time, the task of maintaining adequate ventilation parameters is aggravated by the addition of a secondary bacterial infection of the lungs, which increases the extent of damage to the lung tissue. It is known that when performing invasive mechanical ventilation for more than 2 days, there is an extremely high risk of nosocomial pneumonia. In addition, in patients with COVID and “cytokine storm”, interleukin inhibitors are used, which are pronounced immunosuppressants, which increases the risk of secondary bacterial pneumonia several times.
In conditions of subtotal or total damage to the respiratory surface of the lungs, the success rate of treatment for respiratory failure is extremely low.
Our own experience shows that the survival rate of patients on invasive mechanical ventilation is 15.3% at the current time.
The algorithm for the safety and success of mechanical ventilation includes:
- Consistent use of respiratory therapy techniques.
- Hand treatment of staff before and after patient manipulation.
- Change bacterial filters every 12 hours.
- The use of closed systems for sanitation of the tracheobronchial tree and adequate regular sanitation of the tracheobronchial tree.
- Prevention of leaks in the breathing circuit.
- Using systems for warming and humidifying the respiratory mixture.
- Use of protective parameters of artificial lung ventilation.
- Regular use of prone positions and changes in body position.
- Adequate oral care and regular measurement of endotracheal or tracheostomy tube cuff pressure.
- Adequate selection of antibacterial therapy regimens taking into account the sensitivity of the pathogen.
- Restrictive infusion therapy strategy (CVP no more than 9 mm Hg)
- Timely use of extracorporeal blood purification methods.
- Regular laboratory monitoring of gas exchange parameters (arterial blood acid base level) - at least 4 times a day.
- Regular monitoring of mechanical ventilation parameters and regular assessment of pulmonary mechanics parameters.
- Good patient tolerance of mechanical ventilation (sedation, muscle relaxation, selection of parameters and trigger sensitivity, provided that the patient is conscious and has his own breathing attempts)
Due to the fact that the survival rate of patients using invasive mechanical ventilation remains extremely low, interest in the use of non-invasive artificial ventilation is increasing. According to modern concepts, it is advisable to use non-invasive mechanical ventilation for mild ARDS. In a pandemic and a shortage of intensive care beds, the percentage of patients with severe ARDS prevails over the mild form.
However, in our clinical practice, in 23% of ICU patients, non-invasive mask ventilation (NIMV) was used as initial therapy for DN and ARDS. There are a number of restrictions on the use of NIMVL: the patient must be in clear consciousness and must cooperate with the staff. It is acceptable to use light sedation to ensure maximum patient comfort.
Criteria for the ineffectiveness of NIMVL are maintaining the oxygenation index below 100 mmHg, lack of tightness of the respiratory circuit, agitation and disorientation of the patient, inability to synchronize the patient with the respirator, head and neck injuries, lack of consciousness, lack of own breathing. Respiratory rate more than 35/min.
In our practice, the success rate of NIMVL was 11.1%. Head OAIR: Ph.D. Gruzdev K.A.