In addition to varicose veins, there are a number of other diseases that can cause narrowing of the blood vessels in the legs. As a result, the vessels can narrow to a critical point and stop carrying nutrients to the tissues.
To restore normal blood flow, a phlebologist surgeon performs vascular bypass surgery. A shunt (part of a vessel) is inserted to bypass the damaged section of the vein, allowing blood flow to normalize in the tissue and return them to the necessary nutrition.
The method of shunt insertion depends on the area of vessel damage. Areas of vein damage:
- Femoral part. An incision is made in the groin area, the edge of the shunt is installed in the abdominal aorta, the second part of the shunt is approached to a healthy section of the vein on the thigh.
- Thigh and popliteal part. In this case, the groin area and the back of the knee are cut. The shunt connects a healthy vein in the thigh and an artery running under the knee.
- Femoral-tibial region. Here, one’s own vein is used by connecting the great saphenous vein to the arterial bloodstream. To do this, make a small incision in the groin and lower leg area.
- Method of floor bypass. If in the affected area all vessels have partial blood flow. Then the doctor, to normalize blood flow, introduces a shunt into healthy areas of several veins.
- Foot area. It is carried out to restore blood circulation to the toes. A portion of the great saphenous vein is used as a shunt.
There are two types of shunts:
- Biological (natural) shunts. The biological shunt is very durable: it can restrain the flow of arterial blood. In medicine, the introduction of a biological shunt is often carried out, since the native tissues of the body take root better. The material for making the shunt is taken from the patient's saphenous femoral veins.
- Mechanical or synthetic shunts. Used for extensive vascular lesions. Made from safe polymers. Used in bypass surgery of large vessels.
Briefly about the treatment method
Vascular bypass (Bypass) is an operation to create a bypass when a vessel is blocked by atherosclerotic plaques or blood clots.
Arterial bypass surgery is used for severe forms of arterial circulatory insufficiency. Bypass surgery allows you to save a limb in case of gangrene. A shunt is placed from the artery above the blockage to the artery below the lesion, completely restoring blood supply to the affected organ. Most often, to bypass the arteries of the lower extremities, the patient's own saphenous veins are used, which are treated in such a way as to carry blood to the leg, and not back.
Cause of illness
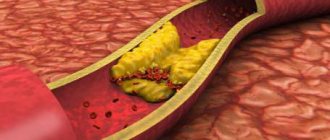
The cause of the disease is the formation of atherosclerotic plaques on the inner wall of the arteries and the gradual layering of salts, cholesterol, fibrin and small blood clots on them. This leads first to a narrowing of the vascular lumen, and then to complete blockage of the artery. The development of the disease can lead to:
- smoking;
- errors in nutrition;
- passion for alcohol;
- overweight, obesity;
- some endocrine disorders - diabetes mellitus, hypothyroidism;
- hereditary predisposition to hyperlipidemia (increased levels of low-density lipoproteins);
- hypertonic disease;
- constant stress and psycho-emotional overload;
- middle and old age;
- insufficient physical activity.
Obliterating atherosclerosis is a serious pathology that needs to be treated, as it can significantly reduce the quality of life. Men suffer from it more often, however, timely consultation with a doctor and correct diagnosis will help maintain health and avoid severe consequences of the disease, such as amputation or death.
Advantages of treatment at the ISC
The Innovative Vascular Center is the only clinic in our country where unique microsurgical, endovascular and plastic methods are comprehensively used to treat patients with incipient gangrene and diabetic foot. Vascular surgeons at our clinic successfully use the method of restoring blood circulation in the limb using a microscope, developed at the University Hospital of Aachen (Germany), for patients with damage to the small arteries of the leg and foot. This is a microsurgical bypass of the arteries of the leg and foot using the patient’s own saphenous vein. Microsurgery allows the successful connection of vein grafts and the smallest vessels with high quality. This allows doctors at our clinic to save limbs for patients already sentenced to amputation.
Since 2011, our clinic has been a leader in Russia in the use of bypass surgery of the arteries of the leg and foot and has the best results in preserving limbs against the background of atherosclerosis of small arteries.
Indications and contraindications for the treatment method
Patients who are in good general condition are selected for bypass surgery. Therefore, a detailed assessment of comorbidities, obesity and other life-threatening factors is carried out. Only an immediate threat to life is a reason for risk in patients with severe concomitant diseases.
It is necessary to evaluate the vascular bed in detail using diagnostic ultrasound and angiography in order to formulate a clear concept for the operation.
A careful assessment of the saphenous veins is necessary, since the success of bypass surgery and the duration of the bypass operation depend on their quality. The use of artificial prostheses as shunts is an operation of despair, since such shunts close in half of the cases within 2 years.
Cost of surgeon's services
The prices indicated in the price list may differ from the actual prices. Please check the current cost by calling +7 495 104 8605 (24 hours a day) or at the GMS Hospital clinic at the address: Moscow, st. Kalanchevskaya, 45.
| Name | Price |
| Brief consultation with a leading surgeon/traumatologist/orthopedist | RUB 4,641 |
| Brief consultation with a surgeon/traumatologist/orthopedist | RUB 3,248 |
| Initial consultation with a leading surgeon/traumatologist/orthopedist | RUB 9,566 |
| Initial appointment with a surgeon/traumatologist/orthopedist | RUR 6,696 |
| Repeated consultation with leading surgeon/traumatologist/orthopedist | RUB 8,131 |
| Repeated appointment with a surgeon/traumatologist/orthopedist | RUB 5,691 |
| Extended consultation with a leading surgeon/traumatologist/orthopedist | RUB 17,224 |
Dear Clients! Each case is individual and the final cost of your treatment can only be found out after an in-person visit to a GMS Hospital doctor. Prices for the most popular services are indicated with a 30% discount, which is valid when paying in cash or by credit card. You can be served under a VHI policy, pay separately for each visit, sign an agreement for an annual medical program, or make a deposit and receive services at a discount. On weekends and holidays, the clinic reserves the right to charge additional payments according to the current price list. Services are provided on the basis of a concluded contract.
Plastic cards MasterCard, VISA, Maestro, MIR are accepted for payment. Contactless payment with Apple Pay, Google Pay and Android Pay cards is also available.
Fast healing and short rehabilitation period
The highest level of personnel qualifications
100% sterile
Modern medical equipment and advanced diagnostic and treatment methods
Make an appointment We will be happy to answer any questions Coordinator Oksana
Preparing for treatment
To determine the indications for femoral-tibial bypass surgery, the patient must be examined in terms of vascular lesions and general health.
The following methods are used to diagnose vascular lesions:
- Ultrasound of the arteries of the lower extremities with pressure measurement at the ankles
- Multislice computed tomography with contrast of the aorta and arteries of the lower extremities
- X-ray contrast angiography - most often used to accurately determine the possibility of angioplasty, instead of bypass surgery
- Duplex scanning of saphenous veins - to determine their suitability as a bypass
General diagnosis of the patient includes:
- General blood and urine tests
- Blood chemistry
- Blood tests for syphilis, HIV and hepatitis
- Electrocardiogram (ECG)
- Ultrasound of the heart (echocardiography)
- Ultrasound of the carotid arteries
- EGDS (gastroscopy of the stomach)
- Chest X-ray
The actual preparation for surgery is to reduce the swelling of the affected leg. To do this, the patient is first given prolonged epidural anesthesia (so that he can lie down). Before surgery, a catheter is inserted into the bladder to monitor urine output. For the purpose of administering medications, an intravenous catheter is installed in the subclavian vein.
On the eve of the operation, the patient is given sedatives, which are supplemented with premedication immediately before the patient is taken to the operating room.
Main types of angioplasty
Depending on the symptoms and degree of damage to the large arteries, an effective and safe surgical method for humans is selected:
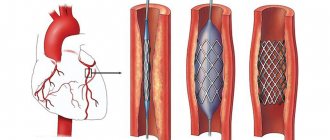
- Transluminal angioplasty - a special balloon is used that is inflated, preventing stenosis. It compresses the plaques on the walls, but after removal there remains a risk of relapse.
- Stenting – a metal structure in the form of a spring creates a strong frame and prevents the artery from decreasing in diameter. After removing the balloon, the stent remains fixed and blocks the accumulation of atherosclerotic plaques. The shape and size of the device are selected individually.
- Laser angioplasty is the newest method in which a quartz thread is inserted into the vessel. Laser beams act on the skin through the skin and increase the temperature, melting cholesterol deposits.
For atherosclerosis of the lower extremities, stenting is most effective. During physical activity, the device supports blood vessels from the inside, controls stretching, blood pressure, and removes swelling in the ankles and cramps in the legs.
Types of angioplastic stenting of the lower extremities:
- Reconstruction of an artery in case of complete blockage by atherosclerotic plaques, installation of an artificial vessel. It starts the blood flow bypassing the affected area.
- An operation to strengthen the stretched artery wall. The stent forms a mesh that restores firmness and elasticity, prevents stenosis, spasms, and thrombosis.
- Standard balloon angioplasty of the iliac artery.
- Administration of drugs simultaneously with the stent for the treatment of atherosclerosis, inflammation, systemic lupus.
When choosing a method, the patient’s age, the presence of contraindications, and general health are taken into account.
Pain relief during treatment
Surgeries on the arteries of the lower extremities in our clinic are performed under epidural anesthesia. The latter involves the introduction of an anesthetic drug into the epidural space of the spine. This type of anesthesia can effectively eliminate pain during surgery and in the early postoperative period.
To monitor the state of the cardiovascular system, we use tracking monitors that are connected to the chest to take an ECG and to the upper arm to monitor blood pressure. In order to improve blood oxygen saturation, the patient is given an oxygen mask.
How the treatment method works
The patient is placed on his back in the operating room. A special cushion is placed under the knee of the operated leg.
The operation begins with a revision (assessment) of the arteries of the leg, to which the shunt should fit. To access the arteries of the leg, incisions 4-6 cm long are used in the groin area and on the lower leg (foot). The artery in the thigh is then accessed to assess its suitability as a donor for the bypass.
After assessing the arteries, the surgeon begins to prepare a venous bypass. Through small incisions, the saphenous vein is exposed on the lower leg, then on the thigh.
The first connection is made between the great saphenous vein and the femoral artery. After stitching the anastomosis, blood flow starts. Shunt pulsation is possible up to the first venous valve.
Then a special instrument with a valvulot is inserted into the venous shunt and the valves are excised. This is necessary so that blood flow can go through this vein from the femoral artery to the artery of the leg. Without cutting the valves, blood will not flow through the shunt.
After removing the valves, the surgeon evaluates the vein using ultrasound and finds blood discharge through the shunt into the side branches. These branches are ligated through separate small incisions. This is necessary so that the blood through the venous shunt moves in the direction of the foot, and does not go into the lateral branches.
When all the discharges along the venous shunt are tied, we begin suturing the shunt and artery on the leg or foot under a microscope. High magnification at this stage is necessary for success, since any error in this will result in failure of the entire bypass operation.
Then the blood flow is started and the operation of the shunt is checked using ultrasound. If blood circulation is restored, the operation ends with suturing of the wounds. If there is any doubt, control angiography is performed and, if necessary, angioplasty of the altered artery below the shunt.
Surgery
Bypass surgery of the blood vessels of the legs is a complex operation that requires high professionalism and certain experience from the surgeon. The operation is performed under general or local anesthesia, depending on medical indications and the general condition of the patients. Epidural anesthesia is considered a modern priority method of pain relief, significantly reducing surgical risk.
Bypass surgery is performed when the patency of arterial and venous trunks is impaired, if their obstruction is more than 50% of the diameter. During the operation, a bypass path is created using a graft from the beginning of the obstacle to its end. Correctly performed surgery ensures restoration of blood flow in the affected vessels.
Stages of the operation:
- A layer-by-layer dissection of the skin and underlying tissues is performed above and below the affected area.
- The vessel is isolated, inspected and its suitability for the upcoming bypass is determined.
- The vessel is incised below the lesion, a shunt is sewn in, and then fixed from above.
- Check the integrity of the implant.
- After assessing the state of blood flow and pulsation of the arteries, deep tissues and skin are sutured.
There are several options for bypass surgery. The choice of each is determined by the localization of the affected area. Immediately after the operation, patients are put on an oxygen mask and given intravenous drips of painkillers.
For the first two days after surgery, patients are prescribed bed rest. Patients are then allowed to walk around the room and hallway. Cold compresses applied for 20 minutes will help relieve pain and reduce swelling of injured tissues during the first 24 hours. All patients are advised to wear compression stockings and socks to prevent blood clots. An incentive spirometer should be used to improve lung function. Doctors examine the incisions daily for possible infection. For 10 days after the operation, specialists conduct dynamic monitoring of the patient, examining indicators of the body’s basic vital functions.
Vascular bypass does not eliminate the etiological factor of the pathology, but only facilitates its course and the condition of the patients. Complex treatment of the underlying disease includes not only surgery, but also lifestyle changes that prevent further development of the pathological process.
Possible complications during treatment
In situ femoral-tibial bypass.
This method involves the use of the patient’s own great saphenous vein, which remains in its usual place, but with the help of special techniques, arterial blood flow is allowed through it into small arteries on the lower leg and foot. Femoro-tibial bypass is the mainstay of treatment for critical ischemia and impending gangrene. Success, with the correct indications for surgery, is achieved in 90% of patients with incipient arterial gangrene (necrosis of the fingers, arterial trophic ulcers). The ability to walk on your own leg is preserved. A venous bypass can be made from the veins of the legs or arms if the main saphenous vein is not preserved.
Peroneal artery bypass
The smallest artery of the leg is the least affected by the atherosclerotic process. However, its capacity is often not enough for the full operation of the autovenous shunt, which leads to thrombosis. The peculiarity of operations on the peroneal arteries is the need to clearly assess the volume of blood flow. To unload the artery, special techniques are often used - unloading fistulas with veins far from the anastomosis.
Multi-storey "jumping" shunts
Patients are often denied leg preservation due to the lack of a good length and patent artery in the lower leg, however, we often see individual sections and branches of arteries with preserved blood flow. Our leading vascular surgeon I.M. Kalitko For such situations, a technique for multi-story bypass of the lower leg arteries has been developed. Often several short bypasses are performed to individual patent segments of the arteries. An important condition for the normal operation of such a complex reconstruction is a reliable assessment of the incoming and distributed blood volume. When shunts are overloaded, unloading fistulas can be used.
Prognosis after treatment method
General surgical complications:
- Bleeding during surgery is a rare occurrence; usually blood loss is 300-500 ml and does not require replacement.
- Suppuration of postoperative wounds - can be observed in weakened patients with diabetes and a purulent process on the foot. Most often the course is favorable, but it delays the patient’s recovery.
Specific complications:
- Reperfusion syndrome is a limb condition associated with the restoration of blood flow against the background of critical ischemia. It is characterized by severe swelling of the limb, pain, and hyperemia. Usually goes away within 2-3 weeks after surgery.
- Lymphorrhea is a prolonged leakage of lymph from incisions. A rare complication in our clinic, the cause of which is damage to enlarged lymph nodes in the groin area during surgical access to the femoral artery.
- The formation of false mycotic shunt aneurysms is a rare complication that occurs when an infection is associated with an autovenous shunt. This is a dangerous condition as it can lead to late shunt rupture or thrombosis.
- Thrombosis of an autovenous shunt can be early or late. Early thrombosis is associated with insufficient outflow through the shunt due to poor arteries below the shunt or high blood clotting. Late thrombosis is associated with the progression of atherosclerosis in the outflow or inflow arteries and scarring of the shunt itself. The use of anticoagulants and control angiography after bypass surgery can eliminate the causes of early thrombosis. To prevent later complications, observation by a vascular surgeon is necessary.