Causes of atrial septal defect
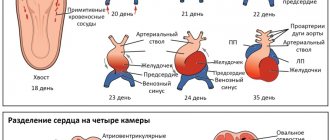
The formation of an atrial septal defect is based on a violation of the development of the primary or secondary septum in the embryonic period.
- The primary defect is located in the lower part of the interatrial septum next to the fibrous rings of the atrioventricular valves (mitral and tricuspid); in fact, its lower edge is the fibrous ring itself.
- The secondary defect is located in the central part of the interatrial septum, and all its edges are represented by the septum itself.
- A venous sinus defect is a defect located in the upper part of the interatrial septum. This defect is often accompanied by abnormal drainage of the pulmonary veins (part of the pulmonary veins flows not into the left atrium, but into the superior vena cava).
Material and methods
Based on the material of the pathological-anatomical department of the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky" in 2015, 41 cases (24 men and 17 women) of idiopathic cystic medianecrosis of the ascending aorta in patients aged 17-73 years were studied.
Material from the Bureau of Forensic Medicine K.Z. Moscow, obtained in 2010-2014, served as the basis for a study of 17 cases (16 corpses of males and 1 female) of sudden death due to aortic rupture in young people from 19 to 39 years old. Death in 78% of cases occurred before the arrival of the ambulance team; in the remaining cases, biological death was ascertained during the examination of the patient. Autopsies were performed 18-24 hours after death.
During a forensic chemical study, ethyl alcohol and narcotic drugs were not found in the organs and tissues of the corpses. In all cases, the immediate cause of death was hemorrhagic shock due to rupture of an aortic aneurysm localized within the ascending aorta.
The control group included 3 cases of death of men aged 25-32 years who died as a result of accidents. Sections of the ascending section of the macroscopically unchanged aorta were examined.
For histological and histochemical studies of the aortic wall, sections were stained with hematoxylin and eosin, picrofuchsin according to van Gieson, fuchselin according to Weigert, Alcian blue, azan according to Heidenhain; Azur-II-eosin staining was used to differentiate cellular elements. For the study of media and microvasculature vasa vasorum
silver impregnation was used.
An immunohistochemical study of sections from paraffin blocks containing surgical material from aneurysms of the ascending aorta was performed automatically in an immunohistosteiner (Bond-Max, Leica) with the following primary antibodies: to smooth muscle actin (SMA) (clone 1A4, Dako), elastin (clone BA-4, Abcam), type I collagen (clone 3G3, Abcam), type III collagen (clone Col-29, Abcam), common leukocyte antigen CD45 (clone 2B11+PD7/26, "Dako"), marker of T-lymphocytes CD3 (clone F7.2.38, "Dako"), B-lymphocytes CD20 (clone L26, "Dako"), macrophages CD68 (clone 514H12, "Leica"), apoptosis marker p53 (clone DO-7, Dako), tumor necrosis factor-α (TNFα) (clone 4E1, Santa Cruz Biotechnology), intercellular adhesion molecule-1 ICAM-1 (clone G-5, Santa Cruz Biotechnology).
The obtained data were processed statistically using the Student-Fisher method with a 95% level of statistical significance using contingency tables and the χ2 test.
Hemodynamics
The meaning of the defect is the discharge of arterial blood from the systemic circulation (left atrium) into the pulmonary circulation (right atrium), which leads to overload of the pulmonary circulation with an excess volume of blood, primarily affecting the lungs. An extreme form of damage is the formation of pulmonary hypertension (high pressure in the vessels of the lungs). Pulmonary hypertension due to atrial septal defect is malignant, leading to severe heart failure and death of the patient.
Symptoms
The first symptoms of the disease occur in the form of shortness of breath during physical exertion, frequent colds, and a feeling of interruptions in the functioning of the heart. At the same time, the symptoms are varied and depend on the location and size of the defect, its combination with other heart defects. Small defects do not have a characteristic clinical picture. Patients do not actively complain, their physical activity is not limited - the defect is discovered by chance. With large, hemodynamically significant defects, patients experience shortness of breath, increased fatigue, and exercise intolerance. After exercise, a cough may occur, sometimes accompanied by hemoptysis. Such patients are characterized by frequent pneumonia and bronchitis.
What are the external manifestations of the disease?
With a congenital aneurysm of the interatrial septum in children, when there are no additional heart defects in the baby, the disease does not affect the physical or mental development of the baby and is not expressed by any symptoms. It’s another matter if the pathology is combined with other congenital heart diseases. In such cases, the child exhibits signs such as:
- increased heart rate;
- bluish skin in the nasolabial triangle;
- the presence of shortness of breath in the baby during breastfeeding;
- tearfulness, anxiety;
- sleep disorders.
Older children may experience signs of tachycardia, pain in the chest from the heart, increased fatigue, weakness, dizziness, loss of appetite, headaches, drowsiness, etc.
Diagnostics
- Examination of the patient with auscultation (listening) of the heart reveals a heart murmur.
- An ECG reveals right ventricular myocardial hypertrophy, right bundle branch block, arrhythmias of varying severity, and a sharp deviation of the electrical axis of the heart to the left.
- X-ray of the chest organs reveals dilation of the pulmonary artery trunk, enlargement of the heart, and increased pulmonary pattern.
- Transthoracic echocardiography allows not only to visualize the atrial septal defect and clarify its nature (primary, secondary, venous sinus defect), but also to assess the direction of blood discharge through the defect and its hemodynamic significance (Qp/Qs).
- Transesophageal echocardiography in adults allows one to obtain detailed information about the edges of the defect, which is important for choosing a method of surgical treatment.
- Probing of the heart chambers and atriography is used when there is insufficient information from the research methods described above or as part of surgical treatment.
What is an aneurysm of the bladder?
Atrial aneurysm is a small anomaly of the heart, which is a protrusion of the vessel wall. In this case, blood circulation is disrupted, and the neoplasm puts pressure on the walls of the atrium. The disease is less common in adults than in children. There are several different forms:
- Protrusion from the left to the right atrium;
- Bulging of the septum of the heart to the left;
- Fusiform pathology, when the upper part protrudes in one direction, the right part in the other.
An aneurysm of the bladder in a newborn and in adults is dangerous not only because of a possible rupture - this happens infrequently. The danger is that if blood flow is disrupted in the acute form of the disease, deviations in the oxygen supply to the brain are likely. Blood clots, clots, and anomalies associated with defects in blood vessels and arteries appear, and a stroke is likely.
Treatment of atrial septal defect
There are currently two types of surgical treatment:
- 1. Open heart surgery under artificial circulation with suturing of the defect or its plastic surgery with a patch from the pericardium.
- 2. Elimination of atrial septal defect using special devices (occluders) in the X-ray operating room through arterial punctures without sternotomy.
- It is necessary to understand that not every defect can be eliminated surgically, there are contraindications to surgery (small-diameter defects, severe pulmonary hypertension, right-left discharge through the defect), and not every defect can be eliminated using occluders (a combination of a defect with abnormal drainage pulmonary veins, primary defects with missing lower edge, large defects, combination of defect with another
- heart pathologies are an indication for open surgery).
- You can learn more about a specific case of the disease, indications and contraindications during a consultation with a cardiovascular surgeon (at an outpatient appointment).
Information for patients. Abdominal aortic aneurysm: Endovascular treatment
Back forward
Preface
This leaflet contains general information for patients. Your healthcare provider can answer any questions you may have.
What is an aneurysm?
An aneurysm is an expansion of weakened artery walls, much like a chamber bulging out of a damaged car tire. The artery wall becomes thinner, loses elastic fibers, and the artery may rupture (burst) under the influence of blood pressure. The largest and busiest artery in the body, the aorta, is most often affected (Fig. 1, 2).
Many thousands of people suffer from abdominal aortic rupture every year. Most of them are men over 60 years old. Aneurysm rupture is a very serious complication with a poor prognosis. Smoking and high blood pressure increase the risk.
How is an abdominal aortic aneurysm diagnosed?
In many patients, an aneurysm is discovered incidentally while they are being evaluated for other conditions (such as kidney or gallbladder problems). Sometimes patients may feel a pulsation in the abdomen. If the aneurysm grows, pain may occur in the spine or in the lower back. If an aneurysm is suspected, your doctor should refer you to a vascular surgeon for consultation; or will immediately send you for an ultrasound. Ultrasound examination is painless and takes very little time. It allows you to identify the presence or absence of an aneurysm. A more precise x-ray called a computed tomography (CT) scan will reveal the exact location and size of the aneurysm.
Risk group
It is known that men over 60 years of age, younger men whose close relatives had aneurysms, or men with other diseases of the cardiovascular system (coronary artery disease, atherosclerosis, hypertension) are at risk.
Is surgery necessary?
Not all cases of aneurysm require surgery. The risk of rupture, and therefore the need for surgery, depends on the size of the aneurysm. It is generally accepted that for large aneurysms (more than 5 centimeters in diameter), it may be safer to perform surgery rather than leave everything as is. This will protect the aorta from rupture. Patients with smaller aneurysms must be examined every 6-12 months to check for enlargement of the aneurysm. On average, an aneurysm grows 0.5 cm per year, so surgery may be required at a later stage. Your vascular surgeon will give you clear recommendations for your case.
What does the operation consist of?
The operation consists of inserting a new sealed inner wall into the aorta (like a tube in a tire), made of a very durable material - polyester. This new wall can be introduced in two ways: open or endovascular surgery. Open surgical treatment necessarily involves a large incision in the abdominal wall to create access to the aorta and replacement of the affected area with a polyester prosthesis. Endovascular treatment is performed through two small incisions, one on the right and the other on the left thigh. A reinforced polyester tube called a stent graft, packaged in a special delivery system, is passed through these small incisions, through the femoral and iliac arteries into the aorta, into the aneurysm cavity. In the aorta, the stent graft is deployed, isolating the aneurysm cavity from blood from the main stream.
Operation efficiency
With early intervention, there is every chance of successful correction of the disease and normal life expectancy. However, you should discuss the pros and cons of surgery in your specific case with your doctor.
How can I help myself?
If you have an aneurysm, there is nothing you can do on your own. However, health promotion under the supervision of a doctor, regular exercise, losing excess weight and quitting smoking will help reduce the likelihood of complications during and after surgery.
Why do I need surgery?
Because the wall of the largest artery - the aorta - is thinned and weakened due to the aneurysm. The operation will help avoid rupture, as well as other complications - compression of neighboring organs, vessels and nerves by the aneurysm, thrombosis, etc.
Before surgery
Before the operation, you need to take tests and undergo examinations in order to find out whether you can have the operation. The examination includes blood tests, urine tests, an ultrasound of the abdomen and an x-ray of the arteries (arteriography), if this has not already been done. With the results of tests and examinations ready, hospitalization is usually carried out the day before the operation
Hospitalization
Please remember to take any medications you take regularly with you. Before surgery, you will have a number of tests if they have not already been done, including an ECG, chest x-ray and blood tests. You will be visited by the surgeon who will perform the operation, as well as an anesthesiologist. If you have questions regarding surgery, please ask your doctor.
Operation
You will be taken to the operating room where anesthetic procedures will be performed first. Depending on the medical indications and your wishes, the operation can be performed either under anesthesia or under anesthesia, during which you will sleep, or under local or spinal anesthesia, so that you are awake during the operation but do not feel pain. A catheter may be placed in the bladder to drain urine. An arterial catheter may also be placed in the arm to quickly monitor blood pressure, and a catheter may be placed in a vein in the arm or neck to administer fluids during and after surgery. In the operating room, the surgeon will make two small incisions on the right and left thigh (see Figure 3).
The surgeon implants an endoprosthesis (stent graft) into the affected area of the aorta. This is done by inserting a guide wire (steel wire) through the incision and into the artery into the aorta. The stent graft is delivered via a guidewire and deployed into the aorta (see Fig. 4). The design of the stent-graft perfectly fixes it on the inner wall of the artery, preventing blood leakage into the aneurysm cavity. After implanting the stent graft and removing the catheters, guidewires, and delivery systems, your physician will suture the incisions on your thighs (see Figure 4). The entire operation is carried out under X-ray television control, so the doctor controls the correct and accurate installation of the endoprosthesis in the aorta.
After operation
You may be taken to the recovery room or to your room where your condition will be monitored. You may be given oxygen through a mask or tube, and you may also need a blood transfusion. You can start eating and drinking as soon as you feel well enough. Pain relief will be given through injections, tablets or through a catheter in the back (epidural). In the next 1-2 days, as the condition improves, various tubes and catheters will be removed.
Discharge home
If absorbable sutures were used, there is no need to remove sutures. If non-absorbable threads or staples were used, they can be removed in the hospital or by a local surgeon. You may feel weak in the first days after surgery, but this should gradually improve over time. Regular exercise, such as short walks combined with other activities, is recommended for the first few weeks after surgery, followed by a gradual return to normal activity.
- Driving : Generally permitted 4 weeks after surgery. If in doubt, consult your doctor.
- Bathing : If the stitches are dry, you can take a bath/shower normally.
- Work : You can return to work 1-3 months after surgery. If in doubt, consult your doctor.
- Exercise : Heavy lifting or straining (including straining, severe coughing) should be avoided for 6 weeks after surgery.
Complications
As with any surgical procedure, there is a possibility of complications occurring during and after the procedure. Doctors and nurses will do their best to ensure that complications do not arise and are prepared to deal with any surprises if they occur.
In the area of the sutures, discomfort and moderate pain in the area of surgical wounds are possible. Sometimes wound healing is complicated by inflammation. This is usually treated successfully with antibiotics. It is also possible that a colorless liquid, lymph, may accumulate in the wound and leak out between the stitches of the suture. This usually goes away with time.
To ensure early detection of post-operative complications, it is very important that you visit your doctor regularly. As a rule, you need to visit your doctor regularly during the first year after surgery, then annually. Tests may include ultrasound, x-rays, and CT scans to make sure the stent graft is working properly.
Regime and lifestyle
If you have been a smoker before, you must make a sincere and determined effort to completely quit the habit. Continuing to smoke will cause further damage to your arteries and your stent graft will likely stop working. Weight loss, diet and regular exercise are also important.