Feel itchy on your feet? Is your skin red and flaky? Such symptoms are characteristic of a specific disease called varicose dermatitis. This is not the simple dermatitis that many of us imagine.
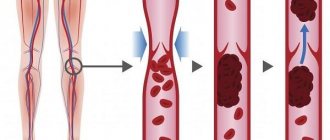
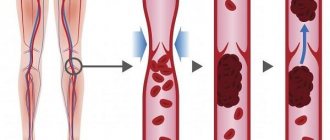
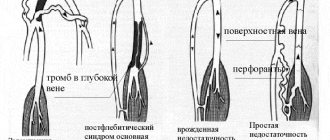
Varicose dermatitis is a skin lesion that occurs in places where the veins have ceased to fulfill their functional purposes. It is not an independent disease. Occurs as a result of vascular damage by varicose veins and thrombosis.
In case of damage to the extremities by varicose dermatitis, it is necessary to contact a phlebologist, since first of all it is necessary to treat the cause of the disease, and not the affected area.
Trophic venous eczema - what is it?
Trophic venous eczema is a pathological condition that occurs in the form of autoimmune dermatitis, that is, serous non-infectious inflammation of the skin (mostly the papillary layer of the dermis and epidermis), accompanied by symptoms of swelling, redness, itching and pain.
Trophic venous eczema
Venous eczema is a type and common form of eczema, which is caused by congestion in the skin due to impaired venous outflow. Venous eczema is also called varicose, congestive or gravitational. It most often has a chronic (recurrent) course. The pathology affects one or both lower extremities in combination with venous insufficiency. In the modern European, and most popular among leading experts, classification of chronic venous diseases - CEAP, this pathology is designated as C4a. This means quite severe tissue damage due to chronic venous edema.
Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Principles of treatment
Hemosiderosis of the skin (post-traumatic hemosiderosis, pigmentary capillaritis, hemorrhagic pigmentary dermatoses, pigmentary purpuric dermatoses) is a condition that occurs after an injury with blood entering the soft tissues (the appearance of a hematoma), or as a result of diseases, the common manifestation of which is the deposition of hemosiderin in the skin.
In our company you can purchase the following equipment for the treatment of skin hemosiderosis:
- M22 (Lumenis)
- IPL Quantum (Lumenis)
Hemosiderin is a dark yellow pigment composed of iron oxide. It is formed during the breakdown of two proteins - hemoglobin and ferritin, for example after blood enters the body's tissues. This can occur after an injury (bruise, injection), when a hematoma forms under the skin. Macrophages do not always have time to utilize the “subcutaneous” blood, as a result of which hemosiderin begins to accumulate in the area of damage. It forms rather persistent local discolorations, which can cause aesthetic discomfort in patients.
The following diseases are also hemosiderosis:
- Pigmented progressive dermatosis of Schamberg
- Annular telangiectatic purpura of Majocchi
- Lichenoid purpuric pigmentary dermatitis Gougerot-Blum
- Favre-Shay ocher dermatitis
- Touraine's arcuate telangiectatic purpura
- Eczematid-like purpura of Doukas-Kapetanakis
- Itchy Leventhal's purpura
- Pigmented purpuric and telangiectatic dermatitis (Purpura senilis)
- Orthostatic purpura
Below we will focus on the most common conditions and pathologies.
Why does trophic venous eczema occur?
Venous eczema is most often observed in middle-aged and elderly patients - according to leading European dermatologists, it affects up to 20% of patients over 70 years of age. This is due to the following reasons:
- Phlebeurysm.
- Previous deep vein thrombosis of the affected limb.
- The presence of venous trophic ulcers.
- Previous cellulitis on the affected limb.
- Chronic swelling of the lower leg, aggravated by hot weather and prolonged static position (standing).
The main cause of the pathology is varicose veins, which is why you can sometimes come across the term “Varicose eczema”.
Venous eczema of atypical localization
Quite often, signs of eczema can be found in young patients with a long history of varicose veins. There is no doctor, both in public and private clinics, who would not observe venous eczema in patients under 40 years of age.
Prevention of venous dermatitis
- Physical activity is beneficial. Aerobic exercises without jumping, walking at a fast pace, cycling, elliptical trainer, skiing improve microcirculation in the legs. Swimming has a powerful anti-edematous effect. At the same time, running, jumping, intense interval training and especially weight training increase impact load and increase intra-abdominal pressure. These sports should not be practiced by people prone to varicose veins.
- While resting, it is good to keep your legs elevated to help the veins carry blood to the heart and relieve swelling.
- Avoid standing still for long periods of time. If you have to stand for a long time without moving, taking steps in place, alternately bending your knees and hips and bending over will help the veins conduct blood.
- A contrast shower on the legs and feet should become a daily morning routine for people with problem veins. Alternate dousing with cold and hot water gives tone to the vascular wall and increases blood flow.
- Compression stockings are specially designed medical products that apply intense compression to the foot and ankle and become looser further up the leg, which promotes good circulation and helps blood move upward against gravity. They are put on in the morning, being in a horizontal position. Depending on the stage of the disease, stockings, knee socks and tights are produced with varying degrees of compression. Your doctor will help you choose the right compression stockings.
- Losing weight significantly reduces the likelihood of disease. Physical activity should be combined with proper nutrition.
Trophic venous eczema is very bad
Varicose eczema has a chronic, relapsing course and a tendency to progress. Quite often you can encounter a situation, especially in public hospitals, when only dermatologists treat venous eczema. Considering the main etiological component of the pathology, impaired venous outflow, treatment of such patients takes years.
Chronic recurrent eczema on the right lower limb
The disease slowly recedes, but invariably appears again. Moreover, trophic changes in the lower extremities progress, lipodermatosclerosis occurs, and then an ulcer appears.
Symptoms of venous dermatitis
As with other types of eczema, with varicose dermatitis the following changes are characteristic of the skin:
- Itching may be the first symptom; it appears unnoticed and gradually progresses, becoming more pronounced at night. Sometimes it is more pronounced on one of the lower extremities.
- Swelling, which is less in the morning, but intensifies in the evening.
- Dryness and flaking;
- Transparent discharge that dries out in the form of crusts. If an infection occurs, the liquid becomes cloudy, purulent, and the drying crusts turn yellow.
These changes primarily affect the inner surface of the ankle, and as the disease progresses, they spread to the foot and lower leg.
On lighter skin, the affected areas appear light brown or pink. In dark-skinned people, the lesion takes on a dark brown or grayish tint and can be difficult to notice. The disease occurs with periods of exacerbation, when symptoms intensify, and remission, when they disappear.
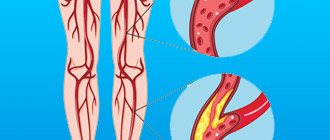
Feet often swell, especially at the end of the day or after periods of standing for a long time. Swelling most often occurs on the lower leg. Varicose veins may also be visible in the form of bluish tubercles and nodules, and spider veins are also characteristic.
Some people also experience these symptoms:
- Change in skin color, which becomes darker, brown, grayish, with a purple tint. This manifestation may appear before all other symptoms.
- The affected surface becomes sensitive and painful when touched.
- When saturated with liquid, the dermis thickens and becomes rougher to the touch; this condition is called lipodermatosclerosis.
- Areas of skin thinning (atrophy) appear that look like thin, whitish scars.
- Pain in the area affected by varicose eczema.
- Plaques and nodules of a purple hue on the legs and tops of the feet, in the place of which painful ulcers form.
- Venous dermatitis is often accompanied by other types of eczema, such as atopic or dyshidrotic.
If varicose eczema is not treated, a trophic ulcer may form on the lower leg. This is a wound that appears in the area of greatest damage to the skin, does not heal on its own, is prone to suppuration and is very difficult to treat. This is facilitated by poor blood supply to tissues compressed by edema.
Cellulite is another complication that develops if treatment is delayed. This is an inflammation of the subcutaneous tissue, which is accompanied by severe swelling, redness, pain, fever and discharge of pus. It occurs when pyogenic bacteria penetrate through damaged skin, and local disruption of microcirculation and decreased immunity contribute to the formation of an infectious focus.
Why does trophic venous eczema almost always appear on the lower extremities?
The answer to this question lies in the pathogenesis of varicose veins, the dominant cause of venous eczema. Varicose veins affect exclusively the lower extremities, where, according to the gravity gradient, it is in their distal parts that trophic disorders occur. One of which is venous eczema.
Trophic eczema of the lower extremities
Pathological eczematous changes in the skin of the lower extremities are most often caused by varicose veins, since they are the cause of impaired venous outflow (up to 90% according to leading experts in the region).
Reasons for appearance
The main cause of varicose dermatitis of the lower extremities is a violation of venous circulation. This condition develops as a result of varicose veins, thrombophlebitis, and venous thrombosis of blood vessels. The development of the disease is provoked by:
- long stay “on your feet” – work in a standing position, long walking;
- cardiovascular diseases;
- overweight;
- traumatic lesions of veins;
- a “sedentary” lifestyle, due to which an increased load is placed on the venous valves.
Trophic venous eczema - diagnosis
Diagnosis of venous eczema in public and private urban medical institutions often begins in a dermatologist’s office, where a specialist evaluates local changes in the skin. It is very important here that the patient is referred to a good phlebologist in a timely manner. If eczematous changes are associated with venous pathology, then treatment of skin manifestations only is likely to be ineffective. Even a visual examination by a phlebologist using all kinds of functional tests often does not reveal the true cause of the pathology. At this stage, the best solution would be a good ultrasound examination of the veins of the lower extremities.
Ultrasound diagnosis of trophic venous eczema
Only competent modern diagnostics of the venous system will help determine the correct treatment tactics.
Stages of development of varicose dermatitis
Like many diseases, varicose dermatitis has 3 stages of the disease:
— 1st stage. It appears as minor changes on the skin in the vein area. A purple-red tint appears on the skin, periodic itching in the legs, minor peeling and thickening of the skin, and a decrease in temperature in the damaged areas. A slight appearance of transparent bubbles may occur.
— 2nd stage. Swelling of the legs and painful sensations appear. Peeling and itching become more intense. The number of watery blisters on the skin increases, which begin to burst and cause wounds. When palpating the affected area, you can feel lumps similar to a wen.
— 3rd stage. The number of bubbles increases. The color of the skin takes on a brownish tint. As a result of the opening of the blisters, a moist area appears and the itching becomes unbearable. Ulcers form on the skin, which, if left untreated, begin to fester.
Trophic eczema, treatment in Moscow
Good treatment of venous eczema in Moscow can be divided into local (topical effect on skin inflammation) and treatment of the venous system. In the first, a dermatologist is often actively involved. Local treatment includes:
- Ointments and creams, steroid drugs, both as part of the latter and as part of systemic treatment.
- The use of antibiotics and antiseptics when an infection occurs.
Often, in the conditions of public medicine, patient care ends at the stage of the above topical treatment. This is not the best solution, since the disease is based on completely different reasons and a relapse of the disease will not take long to occur. Namely, venous stasis, which requires a slightly different approach. It is very important that a patient in Moscow has a timely appointment and diagnosis with a good phlebologist who can determine the correct tactics for managing the patient. The treatment of venous eczema is based on eliminating stasis and improving venous blood flow. Correction of the latter most often involves removing pathologically altered varicose veins. The presence of innovative technologies in modern Moscow centers makes it possible to effectively treat even complicated forms of varicose veins, moreover, on an outpatient basis.
Treatment of trophic eczema in our phlebology center
Leading medical centers in Moscow for the treatment of venous pathology use thermoobliteration techniques for these purposes. In a good city medical phlebology center you can count on safe, effective treatment. Modern vein removal procedures are performed under local anesthesia through skin punctures with minimal surgical trauma.
How to treat varicose dermatitis
Each stage of development of varicose dermatitis has an individual approach to treatment. In order to get rid of varicose dermatitis, systemic treatment is necessary:
- Gets rid of foci of inflammation;
- Relieve swelling of the legs;
- Increase blood flow speed;
- Constant hydration of thickened areas of the skin;
- Prevention of purulent inflammation.
The first stage of treatment of varicose dermatitis
At this stage, medications are taken that increase the muscle activity of blood vessels. Along with medications, treatment includes wearing compression garments. It improves the functioning of vascular walls. Lingerie helps relieve swelling and fatigue in the legs. Antihistamines are used to relieve itching. To prevent skin cracking, moisturizers are used.
If you are faced with the task of choosing compression underwear for yourself, a loved one or relative, we recommend reading the article “Compression stockings: how to choose, compression class, sizes.”
The second stage of treatment of varicose dermatitis
Treatment is the same as in stage 1. To reduce itching, antihistamine and hormonal ointments are used simultaneously. Antiseptic creams are applied to areas with suppuration.
In addition, valerian or motherwort are used to increase calmness of the whole body. Be careful when using such tinctures; they should be used only after being prescribed by your doctor.
The third stage of treatment of varicose dermatitis
In this case, surgery is required. Since recovery is possible only after restoration of vascular changes. Initially, it is necessary to eliminate the acute manifestation of inflammation, this is achieved by:
- Raise the affected leg to a height of 25-35 degrees for blood outflow;
- Washing of emerging ulcers;
- Administration of injections that increase the permeability of blood through the vessels;
- Using elastic bandages to increase pressure on the surface of the leg;
- The use of antihistamines intravenously.
Trophic varicose eczema - treatment without surgery
The main factor in the development of congestive eczema is the pathology of the venous system. Therefore, there is no need to talk about any effective treatment without radical intervention. The best solution would be to stop the inflammation and carry out a procedure to remove varicose veins. But is surgery really that scary?
Trophic eczema - laser treatment in our center
Modern European technologies for vein removal are not inferior to advanced manipulations in dentistry in terms of minimal surgical trauma and possible side effects. But today it would not even occur to anyone to refuse caries treatment due to fear of intervention.
Trophic venous eczema - laser treatment (EVLO, EVLT), radiofrequency treatment (RFA, RFO)
Considering that radical treatment of varicose eczema is the treatment of venous pathology, it is modern methods of removing varicose veins that will be the main way to combat eczema itself. Today, the undisputed leaders at the forefront of innovative treatment of varicose veins are thermal obliteration techniques, laser and radiofrequency. If we compare both technologies, there are simply no fundamental differences for the patient.
Treatment of trophic eczema with radiofrequency
What are the advantages of thermoobliteration technologies:
- Radicality and effectiveness (when used by experienced specialists, the result is practically 100%).
- Low invasiveness, the procedure is carried out through skin punctures.
- Highest cosmetic value.
- Full outpatient, no need for anesthesia or hospitalization.
- Safety and comfort of the procedure for the patient.
The result of laser treatment of trophic eczema after 1 month
After endovascular treatment, the symptoms of eczema quickly resolve on their own.
ARGOSULPHAN in the treatment of trophic and diabetic ulcers of the lower extremities B.S. Briskin, A.V. Proshin, M.V. Polyansky, Ya.I. Yakobishvili, E.V. Kuznetsov Moscow State Medical and Dental University City Clinical Hospital No. 81Trophic ulcers most often complicate the course of the underlying disease - varicose or postthrombophlebetic disease, diabetic foot syndrome [3]. From the point of view of modern basic theory, trophic disorders in chronic venous insufficiency (CVI) are a consequence of valvular insufficiency of various parts of the venous bed of the lower extremities, as a result of which phlebohypertension forms and increases. The latter does not cause direct tissue destruction, but acts through a cascade of pathological changes at the molecular, cellular, microcirculatory and tissue levels. The main proven pathogenetic mechanisms of trophic disorders in CVI are [4]: – leukocyte trapping – a significant increase in the number of leukocytes in the veins and venules of the affected limb; – occlusion of microvasculature vessels due to smudging and formation of microthrombi; – activation of leukocytes and their penetration into surrounding tissues; – extravasal polymerization of fibrinogen in the form of a fibrin “cuff” around the venous and arterial limbs of the capillaries; – swelling of soft tissues, which results in an increase in the distance between capillaries and a deterioration in metabolic processes. Ultimately, tissue damage develops with the emergence of a primary affect. Diabetic trophic ulcers are a consequence of diabetic macro-microangiopathy and polyneuropathy. The main cause of morbidity, hospitalization and mortality in patients with diabetes is infection of the lower extremities. Infection is a common complication of developing ulcers or wounds on the foot [8]. In conditions of impaired blood flow, infection significantly worsens the prognosis of the likelihood of saving a limb or even life itself [2]. The infectious process promotes thrombosis of arteries already changed due to atherosclerosis, which leads to the progression of ischemia and the development of gangrene [6]. Currently, the polymicrobial nature of a purulent focus with an association of aerobes and anaerobes on the feet of patients with diabetes is generally accepted [5, 7]. The arsenal of drugs used for local treatment of wounds has now expanded significantly, but its results remain not entirely satisfactory due to the high cost and low availability of a number of drugs. Inpatient treatment for several months is not economically feasible [1]. One of the alternative methods of local treatment of trophic ulcers of the lower extremities of various etiologies is the administration of the drug Argosulfan, which is a 2% silver salt sulfathiazole cream. It has been established that the combination of silver with sulfonamides has an antibacterial effect that is several tens of times more powerful than sulfonamides alone. Argosulfan has a local antimicrobial effect, exhibiting a wide spectrum of action against gram-negative and gram-positive bacteria. The antibacterial effect of sulfathiazole is enhanced by the influence of silver, which has an oligodynamic effect and at the same time weakens the sensitizing properties of sulfonamides. Silver ions inhibit the growth and division of bacteria by binding to DNA. Sulfathiazole inhibits the proliferation of bacteria. In addition, silver helps accelerate regenerative processes in the wound. The low solubility of the silver salt of sulfathiazole makes it possible to maintain a constant concentration of the drug in the wound, and also ensures non-toxicity due to minimal resorption. The hydrophilic base and appropriate pH level of Argosulfan cream ensure its analgesic effect and good tolerability. It should be emphasized that the drug is stable and does not decompose under the influence of light. Materials and research methods The study was carried out on the basis of the department of purulent-septic surgery of City Clinical Hospital No. 81. An analysis of the results of treatment of 72 patients with trophic defects of soft tissues of various locations and origins, in whom Argosulfan was used as local treatment, was carried out. Of these, 44 patients were in the hospital for complicated forms of diabetic foot (wounds after treatment of diabetic phlegmon and gangrene of the feet), 26 - with trophic ulcers of the legs against the background of chronic venous insufficiency with a duration of existence from 3 to 5 years. The age of the patients ranged from 36 to 76 years. There were 31 men (43.1%), 41 women (56.9%). The characteristics of patients by age and sex are presented in Table 1. The average duration of diabetes mellitus in 44 patients exceeded 15 years, which undoubtedly influenced the severity of the wound process due to neuro-vegetative disorders and pronounced changes in microcirculation. The absence of a working classification of diabetic foot syndrome in domestic surgical practice allows us to propose a generalized classification developed in our clinic, taking into account the morpho-anatomical changes in the foot, reflecting the state of regional blood flow and sensorimotor disorders [1]. Classification of complicated forms of diabetic foot syndrome A. By form: 1. Neuropathic foot; 2. Ischemic foot; 3. Neuroischemic foot.
B. According to the extent of the lesion (Wagner): degree 0 – no changes in the skin or bone deformities; 1st degree – superficial ulcer without penetration into the deeper layers; 2nd degree - superficial ulcer with damage to the tendon, bone, articular ligaments; 3rd degree – inflammation of the tendon sheath, osteomyelitis or deep abscesses; 4th degree – gangrene of the fingers or the entire foot; Grade 5 – gangrene of the entire leg.
B. According to the location and nature of the lesion: Right, left foot, damage to both feet. The surface is dorsal, plantar, and both at the same time. Foot area – toes, metatarsus, tarsus, joints, foot as a whole.
1. Fingers (felons: cutaneous, nail (paronychia, subungual felon), subcutaneous, tendon (purulent tendovaginitis, plantar and dorsal purulent tendobursitis), bone, articular, osteoarticular) 1.1. Ulcer: superficial, perforating 1.2. Acral necrosis of the finger 1.3. Pandactylitis: gangrene – dry, wet.
2. Foot 2.1. Abscesses 2.1.1. Skin 2.1.2. Mozolny
2.2. Cellulitis: 2.2.1. Epifascial plantar and dorsal surface 2.2.2. Interdigital 2.2.3. Subaponeurotic of the plantar surface and dorsum of the foot 2.2.4. Lateral plantar space 2.2.5. Medial plantar space 2.2.6. Median plantar space
2.3. Foot ulcer 2.3.1. Surface 2.3.2. Perforating
2.4. Gangrene of the foot 2.4.1. Dry 2.4.2.Wet
2.5. Panphlegmon.
Based on the proposed classification, 26 patients (59.1%) were diagnosed with a neuropathic form of foot damage, and 18 (40.9%) - neuroischemic. The neuroischemic form of foot damage occurred with a predominance of neuropathy - in 65% and dominance of ischemia - in 35%. The group of observed patients included patients with types I and II diabetes mellitus. In table Figure 2 shows the distribution of patients depending on the type of diabetes, its severity and insulin dependence. All the patients we studied with complicated diabetic foot syndrome had trophic disorders in the tissues of the foot with the formation of ulcers, abscesses, phlegmon, osteomyelitis, necrosis, and gangrene. All patients underwent various organ-preserving surgical interventions on the foot (opening and drainage of phlegmons, disarticulation of fingers, foot resections, necrectomy). The control group included 88 patients with trophic ulcers and wounds on the lower extremities. Of these, 56 were with complicated diabetic foot syndrome and 32 were with trophic ulcers due to venous insufficiency, who received standard medications (dioxidine, chlorhexidine, ointment dressings with Levosin, Levomekol) as local treatment for wound healing. To assess the effectiveness of the ongoing antibacterial therapy, we used data from cytological studies of contents from wounds and microbial contamination of the tissues of the purulent focus. Results and discussion The use of Argosulfan in the local treatment of wound processes made it possible to improve the course of the wound process in all patients. This was expressed, first of all, in the reduction or disappearance of pain during and outside of dressings, in the cleansing of the wound defect from necrotic tissue with the appearance of mature granulations and marginal epithelization in the area of the ulcer by the 10th day of treatment in 24 of 26 patients with CVI of the lower extremities, as well as the absence or sharp decrease (up to 102) of microflora growth. The most frequently sown pathogens in this group of patients were Staphylococcus aureus – 78%, Pseudomonas aeruginosa – 13%, Proteus vulgaris – 9%. The use of Argosulfan in patients of this group led to rapid scarring of ulcers (on average within 20–22 days depending on the depth and extent of the defect), in 18 patients and in 8 it allowed to prepare the trophic ulcer for plastic closure, in contrast to patients in the control group, where this dynamics in terms of the wound process was noted only by 30–32 days. In patients with complicated diabetic foot syndrome, positive dynamics in local wound treatment were also obtained in the vast majority of patients. Locally: in 26 patients with a neuropathic form of foot damage, a decrease or disappearance of swelling on the foot, a decrease or relief of the phenomena of bacterial cellulite, a limitation of necrosis, and a tendency to cleanse postoperative wounds were noted. The most frequently cultured pathogens in patients with complicated diabetic foot syndrome are presented in Table. 3. With the neuroischemic form of foot damage, all patients noted a limitation of the purulent-necrotic process on the foot with a tendency to clear it with relief of the phenomena of perifocal inflammation. It should be noted that preventing the generalization of infection on the foot in this category of patients made it possible to carry out a complex of conservative therapy or perform reconstructive surgery aimed at relieving the phenomena of critical ischemia in the affected foot. We consider this point important in the pathogenetic treatment of the neuroischemic form of foot injury, since early radical surgical interventions on the foot without restoring blood flow under conditions of ischemia lead to the generalization of infection with the development of gangrene, which ends in high amputation of the limb. In 4 patients, against the background of local application of Argosulfan and complex conservative therapy, reconstructive surgical interventions on the arteries of the lower extremities were successfully performed, and in 8 patients, extraperitoneal lumbar sympathectomy was performed, aimed at improving regional blood flow in the affected limb. Thus, the clinical effectiveness of local treatment of wound processes with Argosulfan was 100%. The duration of local treatment with Argosulfan in patients with complicated diabetic foot syndrome was carried out on average 14–20 days, until a clear clinical effect appeared and the level of microbial contamination in the wound decreased to 103 microbial bodies per 1 g of tissue, which allowed the wound to heal or prepare it for plastic surgery. closing To assess the effectiveness of the treatment, data from studies of cytological prints from wounds and microbial contamination of the tissues of the purulent focus were used. Cytological examination of wound prints makes it possible to judge the nature and phases of the wound process, the effectiveness of the complex treatment, and, in turn, determine indications or contraindications for various conservative and surgical measures. Cytological examination was based on determining the quantitative and qualitative composition of neutrophils, lymphocytes, macrophages, fibroblasts, and the presence of microflora. For a more accurate idea of the dynamics of the cellular composition, it was expressed as a percentage when counting 100 cells in different parts of the preparation, depending on the homogeneity of the cellular composition of wound prints in patients with various forms of complicated diabetic foot syndrome (neuropathic, neuroischemic). Analysis of the data obtained indicates that upon admission to the hospital in 23% of patients, the cytology of the wound process was degenerative-inflammatory in nature. The cellular composition of the wound in this type of cytogram was characterized by the presence of neutrophils in a state of varying degrees of destruction, as well as a large number of microorganisms. In 39% of patients, a purulent-necrotic type of cytogram was noted. This was evidenced by a large number of neutrophils in a state of degeneration and destruction. In all patients, the presence of microorganisms was noted among the destroyed neutrophils in the cytograms. In 38% of patients, the cytology of the wound process corresponded to the purulent-inflammatory type. In this group of patients, the cellular composition was characterized by a predominance of neutrophils, most of which were in the stage of decay. Other cellular elements in the wound print had degenerative changes. The cytological dynamics of the wound process were assessed from the moment the patient was admitted, on days 3, 5, 10, 15 of treatment. On days 10–14 of antibacterial therapy with levofloxacin, the cytological characteristics of the wound process changed - in 42% with a transition to the inflammatory type, in 38% to the inflammatory-regenerative type, which was characterized by the predominance of a neutrophilic reaction, combined with a high level of lymphocytes and macrophages, as well as the presence in smears-imprints of single fibroblasts. Continuing the course of antibacterial therapy in patients with the inflammatory type of cytogram for 10–14 days made it possible to change it to regenerative in 79% of patients. At the same time, it was possible to achieve a reduction in the level of microbial contamination in the purulent focus to 103–104 microbial bodies in 97% of patients, in contrast to the control group, where this degree of microbial contamination was achieved only in 78%. A complex of clinical, microbiological and cytological studies made it possible to resolve the issue of discontinuing antibacterial drugs. Further treatment of the open wound was carried out only under dressings with Argosulfan, which provides a high antimicrobial effect directly in the wound. In the control group, 36% of patients continued to use broad-spectrum antibiotic therapy. Conclusions 1. Argosulfan mixes well with wound secretions and prevents the gauze bandage from sticking to the wound surface. 2. During treatment with the drug, activation of the processes of granulation and epithelization in the wound surface is observed. 3. Argosulfan is well tolerated by patients; no cases of local or general allergic reactions were detected during treatment. 4. Argosulfan 2% cream effectively prevents the occurrence of reinfection of the wound surface due to a wide spectrum of antimicrobial activity.
ABSTRACT Argosulfan in the treatment of trophic and diabetic ulcers of the lower extremities The article presents the results of our own study of the effectiveness of Argosulfan in the treatment of trophic and diabetic ulcers of the lower extremities. During the study, the clinical effectiveness of local treatment of wound processes with Argosulfan was 100%. Acceleration of granulation and epithelization of the wound surface and a decrease in microbial contamination were observed. The drug is easy to use, does not cause adverse reactions and can be recommended as a local antibacterial and wound healing agent for widespread use in clinical practice in patients with trophic ulcers of the lower extremities.
REFERENCES 1. Briskin B.S., Proshin A.V., Kuznetsov E.V. et al. Main directions in complex therapy of patients with complicated forms of diabetic foot //International Medical Journal. 2001. No. 8. P. 49-52. 2. Dibirov M.D., Briskin B.S. Surgical treatment of complications of diabetic angiopathy // Moscow. 2001. 327 p. 3. Kirienko V.Yu., Bogachev V.Yu., Bogdanets L.I. Treatment of trophic ulcers of venous etiology // Consilium medicum. 2000. pp. 22-26. 4. Savelyev V.S., Kirienko A.I., Bogachev V.Yu. Venous trophic ulcers // Phlebolymphology. 2000. No. 11. P. 5-10. 5. Svetukhin A.M., Zemlyanoy A.B. Purulent-necrotic forms of diabetic foot syndrome // Consilium medicum. 2002. T. 4. No. 10. P. 537-544. 6. Boyko EJ, Lipsky BA Infection and diabetes. In: Harris (ed) Diabetes in America, 2nd Ed. Bethesda, Md., National Institutes of Health Publication 1995:95 – 1468. 7. Gerding DN Foot infections in diabetic patients: the role of anaerobes. Clin. Infect. Dis 1995;20(Suppl. 2):283- 8. Lipsky EA Infections problems of the foot in diabetic patients. Levin and O'Neal's The Diabetic Foot. Eds. Bowker JH, Pfeifer MA St. Louis, C. V. Mosby, 6th Ed. 2001. 467-80.
Polyclinic No. 2 2006 (14-19)
Results of treatment of trophic venous eczema. Photos before and after treatment
The result of treatment of trophic eczema using endovenous laser coagulation (EVLC) using German Biolitec technology in our center
Photos before and after treatment of trophic eczema on the left lower limb
The result of treatment of trophic venous eczema using radiofrequency ablation (RFA) in our patient
Photos before and after treatment of trophic venous eczema on the left lower limb
Composition and effect of gels and ointments for varicose veins
Creams, gels and ointments for varicose veins are produced based on the following substances:
- hirudin;
- vitamin P;
- heparin.
Many similar preparations are created with the addition of plant extracts of birch leaves, horse chestnut and other substances.
External use of ointments, gels and creams for varicose veins allows you to relieve the symptoms of the disease (pain disappears, swelling decreases). Most external remedies for varicose veins also have a venotonic and anti-inflammatory effect. However, this is not enough to completely cure the disease.
Frequently asked questions from patients on the Internet about trophic venous eczema
How to treat venous eczema of the legs in Moscow?
For good treatment of venous eczema of the lower extremities in Moscow, you need to contact a competent specialist, a phlebologist. The doctor will conduct a detailed diagnosis, including an ultrasound examination. Only after this can we talk about modern treatment. The best solution would be to find a good city phlebological center, where the ultrasound will be performed by the phlebologist himself.
What is the modern treatment for venous eczema of the legs in Moscow?
In Moscow, good modern treatment of venous eczema that meets European standards includes innovative technologies for both diagnosis and treatment. Leading city phlebological centers, including our Moscow Innovative Phlebological Center, successfully treat venous eczema. First, a detailed duplex angioscanning of the venous system of the lower extremities is performed. Only then is treatment prescribed, including the fight against local inflammation and modern treatment of the true cause of eczema, varicose veins.
How to treat venous eczema with folk remedies?
Specialists of the Moscow City Phlebological Center have good experience in working with various trophic disorders in venous diseases, including venous eczema. Leading phlebologists at our center do not recommend treating venous eczema with folk remedies. The disease responds well to treatment using modern technologies, but we often encountered serious complications after treatment with folk remedies.
My mother has venous eczema on her legs, which doctor is best to see?
If you suspect that your mother has venous eczema, it is better to first contact a good phlebologist, a doctor specializing in the diagnosis and treatment of venous pathology. First you need to understand the cause of inflammation in the lower extremities. You may need the help of a dermatologist. If eczema is of venous origin, then now there are modern European technologies with the help of which curing your mother will not present any special problems.
Treatment of venous dermatitis
In case of dermatitis associated with vein pathology, it is necessary to consult a doctor as soon as possible. If treatment is not started on time, dangerous complications can develop that can be very difficult to cope with.
All therapy is divided into drug treatment and a number of non-drug measures aimed at alleviating the condition and reducing symptoms.
- For venous dermatitis, soaps and bubble baths are contraindicated, as they dry out the skin and irritate areas of the body affected by eczema. Regular moisturizing lotion can be used as a substitute for soap by applying to damp skin and then rinsing off.
- When using a shower or bath for personal hygiene, the water should be lukewarm, or even cool. Hot water causes severe loss of moisture and worsens the itching.
- Contact with water should be short. Water washes away the fatty protective layer, and moisture freely evaporates from the skin. You should not take a bath longer than 10 - 15 minutes.
- Products containing alcohol, dyes and fragrances are dangerous for eczema skin. They can cause irritation and allergies, and worsen the symptoms of dermatitis.
Treatment with medications
- Emollients, or medicated moisturizers, help keep skin hydrated and elastic and prevent damage and cracking. This is one of the most important groups of drugs in the treatment of all types of eczema. Use the product on your legs and feet twice a day, or more often if your skin is very dry. Apply it with light movements, in enough quantity to make the skin look slightly shiny.
- Glucocorticosteroids are medications based on adrenal hormones. They have an anti-inflammatory effect. Entering the subcutaneous tissue, glucocorticoids inhibit immune cells and prevent them from releasing inflammatory mediators - chemicals responsible for the symptoms of eczema. In the treatment of venous dermatitis, these drugs should be used with caution, since tissue swelling and increased vascular permeability in the area of the pathological process lead to the fact that the drug is absorbed in large quantities and enters the bloodstream. Side effects can be quite serious: decreased immunity, obesity, increased blood pressure and blood sugar levels, suppression of the adrenal glands. Therefore, moderate or weak glucocorticoids are used according to their potency, and they are prescribed for a short course. Hydrocortisone and prednisolone ointments are suitable.
- Non-steroidal anti-inflammatory ointments regulate immunity and suppress inflammation, while they do not contain hormones and are free of their side effects. These drugs include Elidel cream; it is well suited for targeted therapy of varicose veins dermatitis.
- Zinc oxide is used in this disease due to its drying effect. Due to swelling, eczema against the background of varicose veins often becomes wet, and clear discharge oozes from the lesions on the skin. Zinc oxide reduces itching, softens and alleviates general discomfort.
- Antimicrobial agents become relevant if an infection occurs. In conditions of impaired microcirculation, edema and damage to the epithelium, bacteria inhabiting the surface of the body easily penetrate inside, into the subcutaneous tissue, and cause inflammation. In this situation, antibiotics must be taken in tablet form, and antiseptic solutions must be used topically. The doctor selects a suitable drug, usually a broad-spectrum antibiotic from the group of penicillins, cephalosporins or macrolides.