Increased aggregation is a marker of hyperaggregation syndrome and thrombophilia. The most commonly used are the Born turbidimetric method, based on recording changes in the light transmission of platelet-rich plasma, and the method for studying platelet aggregation, based on the analysis of light transmission fluctuations caused by a random change in the number of particles in the optical channel.
Material for research.
Citrate platelet rich plasma
Research method
is determined by the operating procedure on a particular type of aggregometer.
Solutions of ADP, ristocetin, collagen, adrenaline, and arachidonic acid are most often used as inducers. Solutions of thrombin, serotonin, etc. can also be used.
Platelet aggregation with ADP
Exposure to small doses of ADP (usually 1*10-7 mol) leads to the formation of a double wave of aggregation. The first phase (primary wave) depends on added exogenous ADP, and the second phase (secondary aggregation wave) occurs due to the release reaction of intrinsic agonists contained in platelet granules. Large doses of ADP (usually 1*10-5 mol) lead to the merging of the first and second waves of aggregation.
When analyzing aggregograms, attention is paid to the general nature of aggregation (single-wave, two-wave; complete, incomplete; reversible, irreversible) and the rate of aggregation. The appearance of two-wave aggregation upon stimulation of ADP at concentrations that normally cause reversible aggregation (usually 1-5 µmol) indicates an increase in platelet sensitivity, and the development of single-wave incomplete (and often reversible) aggregation upon stimulation of ADP at concentrations of 10 µmol or more indicates an increase in platelet sensitivity. impaired platelet release reaction.
When should you get tested?
Indications for the study are:
- excessive bleeding gums;
- nosebleeds;
- the appearance of hemorrhagic rashes;
- prolonged blood cessation even with minor vascular damage;
- tendency to bruise;
- the need for treatment with antiplatelet agents and anticoagulants;
- pregnancy with a high risk of developing gestosis or bleeding during childbirth;
- pathologies of the hematopoietic system.
The study must be carried out before surgery. A low degree of platelet aggregation can lead to large blood losses during surgery, which must be taken into account.
The analysis is mandatory for pregnant women to assess the functional activity of platelets. The results of the study will help select preventative agents for excessive blood loss during childbirth.
In addition, this indicator is determined if treatment with antiplatelet drugs and anticoagulants is necessary. Aspirin in small dosages is indicated for people with atherosclerosis and pathologies of the cardiovascular system. Based on the analysis data, tentative forecasts are made for the body’s reaction after taking aspirin.
It is known that platelet aggregation is also affected by drugs from other groups (antibiotics, antihistamines, anti-inflammatory drugs). Therefore, analysis is also advisable when planning to take these drugs.
Read further: Norm of platelets in the blood of women by age
Platelet aggregation with ristocetin
Determination of platelet aggregation with ristocetin in plasma is used to quantify von Willebrand factor. The method is based on the ability of ristocetin to stimulate in vitro the interaction of von Willebrand factor with platelet glycoprotein Ib. In most cases of von Willebrand disease, there is a violation of ristocetin aggregation with a normal response to the effects of ADP, collagen and adrenaline. Disturbances in ristocetin aggregation are also detected in Bernard-Soulier disease. For differentiation, a test with the addition of normal plasma is used: in von Willebrand disease, after the addition of normal plasma, ristocetin aggregation is normalized, while in Bernard-Soulier syndrome this does not happen. Ristocetin-induced platelet agglutination is reduced in most cases of von Willebrand disease, except type IIB.
References
- Clinical laboratory diagnostics, National guidelines, Volume 1, Dolgov V.V., Menshikov V.V., 2012, pp. 761-765
- Kozlovsky V. I., Kovtun O. M., Seroukhova O. P., Detkovskaya I. N., Kozlovsky I. V. Research methods and clinical significance of platelet aggregation. Focus on spontaneous aggregation // Vestnik VSMU. 2013. No. 4.
- Puri RN, Colman RW.ADP-induced platelet activation.Crit Rev BiochemMol Biol. 1997;32(6):437-502. doi: 10.3109/10409239709082000. PMID: 9444477.
- Murugappa S, Kunapuli SP. The role of ADP receptors in platelet function.FrontBiosci. 2006 May 1;11:1977-86. doi:10.2741/1939. PMID: 16368572.
- Barbara Lunghi, Anna Lecchi, Rosa Santacroce, Mariangela Scavone, Rita Paniccia, Andrea Artoni, Christian Gachet, Giancarlo Castaman, Maurizio Margaglione, Francesco Bernardi, Marco Cattaneo. Severe bleeding and absent ADP-induced platelet aggregation associated with inherited combined CalDAG-GEFI and P2Y12 deficiencies.Haematologica 2020;105(7):e361-e364
Platelet aggregation with collagen
Platelet aggregation with collagen has a fairly pronounced latent phase, during which phospholipase C is activated. Depending on the concentration of the reagent used, the duration of this phase can be 5-7 minutes. After the end of this period, processes occur in platelets that lead to the formation of second messengers, as a result of which the secretion of platelet granules and the synthesis of thromboxane A2 develop, which is accompanied by a sharp increase in interplatelet interaction.
In laboratory and clinical practice, collagen is most often used in a final concentration of 50 μg/ml, however, collagens from different companies may have different activities, which must be taken into account when using them.
Reasons for decreasing and increasing aggregation
Increased aggregation level or hyperaggregation is a condition in which blood flows slowly through the vessels and quickly clots. Provocateurs of such deviation can be:
- diabetes;
- hypertonic disease;
- cancer of the kidneys, gastrointestinal tract or blood;
- vascular atherosclerosis;
- leukemia;
- sepsis;
- lymphogranulomatosis;
- surgical excision of the spleen;
- menstruation in women.
Moderate platelet hyperaggregation during pregnancy is normal. This deviation occurs due to the need to nourish the placenta with blood. The value reaches its peak in the 3rd trimester of gestation.
A decrease in platelet aggregation occurs due to the following pathologies:
- thrombocytopathy;
- diseases of the hematopoietic system;
- use of antiplatelet agents;
- renal failure;
- dysfunction of the thyroid gland;
- anemia;
- alcohol abuse.
Platelet aggregation
Platelet aggregation with adrenaline
Adrenaline, upon contact with platelets, interacts with α2-adrenergic receptors, which causes inhibition of adenylate cyclase. It is possible that the mechanism underlying the implementation of the effect of adrenaline and the development of the first wave of aggregation does not depend on the formation of thromboxane A2, the release reaction or the synthesis of platelet aggregation factor, but is associated with the ability of adrenaline to directly change the permeability of the cell membrane to calcium ions. The second wave of aggregation occurs as a result of the release reaction and production of thromboxane A2.
Indications for analysis
Platelet aggregation is studied when:
- hemorrhagic disorders (increased bleeding);
- thrombophilia (coagulation disorder with an increased risk of thrombosis);
- severe atherosclerosis;
- diabetes mellitus;
- before performing surgical interventions;
- during pregnancy;
- when monitoring the effectiveness of anticoagulant and antiplatelet therapy.
Also, this study is important in the diagnosis of hereditary hemorrhagic thrombocytopathies.
Platelet aggregation with arachidonic acid
Arachidonic acid is a natural aggregation agonist, and its action is mediated by the effects of prostaglandins G2 and H2, thromboxane A2, and includes activation of both phospholipase C with subsequent formation of second messengers, mobilization of intracellular calcium and expansion of the cell activation process, and phospholipase A2, which directly leads to release of endogenous arachidonic acid. Platelet aggregation with arachidonic acid occurs quite quickly, so the curve characterizing this process is often single-wave in nature.
To induce aggregation of blood platelets, arachidonic acid is used in concentrations of 10-3-10-4 mol. When working with arachidonic acid, it should be taken into account that in air this substance oxidizes very quickly.
An aggregation test with arachidonic acid is recommended in cases of using drugs that affect the aggregation reaction (for example, acetylsalicylic acid, penicillin, indomethacin, delagil, diuretics), which must be taken into account when assessing the research results.
Platelet hemostasis
Study of platelet aggregation ability
Evaluation of patients with bleeding requires a thorough history, including family history, medication history, physical examination, and only then laboratory testing.
Quantitative and functional platelet abnormalities are common in patients with bleeding disorders.
Types of platelet dysfunction:
| Platelet dysfunction | Probable diagnosis |
| Impaired platelet adhesive function | Bernard-Soulier syndrome Velocardiofascial syndrome Glanzmann's thrombasthenia Congenital afibrinogenemia Von Willebrand disease (possibly a platelet type of von Willebrand disease) Collagen receptor defects |
| Platelet receptor abnormalities | TxA2 receptor defects α-adrenergic receptor defect P2Y12 receptor defect Antiplatelet drugs (eg, clopidogrel) |
| Platelet granule abnormalities | Deficiency of dense granules - deficiency of α-granules - gray platelet syndrome |
| Abnormalities in secretion of the contents of platelet granules, or disruption of signal transduction in platelets | Primary secretion defects Aggregation defects that are similar to those seen in platelet pool storage disorders, but with normal granule and TxA2 content Defects in platelet surface receptor agonists - epinephrine - thromboxane - ADP - collagen Defects in protein G activation (defects in intracellular signal transduction) |
| Arachidonic acid metabolism disorder | Cyclooxygenase defects Thromboxane synthase deficiency Taking drugs |
| Disturbance of the procoagulant mechanism of platelets | Scott syndrome |
| Platelet cytoskeleton defects | MYH9-associated disorders Wiskott-Aldrich syndrome |
Before performing specific tests examining the functional properties of platelets, it is recommended to perform the following laboratory tests:
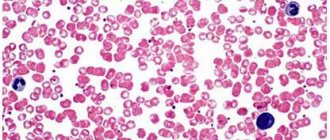
- Complete blood count with determination of platelet count and average platelet volume. This is important for hereditary macrothrombocytopenia (Bernard-Soulier syndrome), microthrombocytopenia (Wiskott-Aldrich syndrome), and for some bone marrow diseases.
- Study of blood smear and platelet morphology. Necessary for establishing diagnoses such as pseudothrombocytopenia, gray platelet syndrome. In some cases, for example, with Hegglin's thrombocytopenia, a blood smear may show the presence of Dele bodies (light gray-blue oval basophilic leukocyte inclusions located in the peripheral cytoplasm of neutrophils).
Specific laboratory tests to determine the functional properties of platelets include examinations such as:
- screening tests reflecting the functional activity of platelets, for example, activated clotting time (ACT), bleeding time (BT) and PFA-100, - aggregometry, for example, classical Born aggregometry , - flow cytometry to quantify the presence or absence of platelet membrane glycoproteins, — specialized studies used in research laboratories.
The principle of the Born aggregometry method:
The method for measuring platelet aggregation using the Born turbidimetric method is based on recording changes in light transmission in a platelet suspension. These changes are due to a decrease in light scattering and an increase in light transmission (transparency) of the suspension during the formation of platelet aggregates.
Classical Born aggregometry uses platelet-rich plasma (PRP). In the aggregometer, BTP is mixed in a cuvette at a temperature of 37°C. When an agonist is added, the resulting platelet aggregates absorb less light, which is detected by a photocell.
PRP – platelet-poor plasma, PRP – platelet-rich plasma.
The principles of Born aggregometry can be clearly seen in the animated English-language presentation, kindly provided by the authors of the scientific website https://www.platelet-research.org - https://www.platelet-research.org/3/aggregometry.htm.
Pre-analytical variability
Drugs that block platelet function include NSAIDs (non-steroidal anti-inflammatory drugs), specific antiplatelet drugs such as clopidogrel, as well as some antibiotics, antidepressants, beta blockers, etc. Foods such as garlic, turmeric can also affect platelet function and caffeine, high-fat foods (these can cause chylomicrons in the plasma, which interferes with normal light transmission during platelet aggregation testing). A number of factors can influence the accuracy of platelet aggregation results:
- very high or low platelet count;
- temperature - blood samples for platelet aggregation testing should be stored at room temperature;
— pH — platelet aggregation should be carried out at a physiological pH value;
- fibrinogen concentration.
Platelet agonists:
The addition of a platelet agonist to PRP leads to activation of platelets, a change in their shape from discoid to spherical, which is associated with an increase in optical density during platelet activation. The only exceptions to this are adrenaline (epinephrine), which does not change the shape of platelets, and ristocetin, which causes platelet agglutination rather than aggregation.
There are two types of agonists:
- strong agonists - collagen, thrombin, ThA2, arachidonic acid - directly cause platelet aggregation, synthesis and secretion of ThA2 platelet granules.
- weak agonists - ADP and adrenaline - cause platelet aggregation without causing secretion.
Strong agonists at low concentrations may act as weak agonists, but weak agonists, even at high concentrations, will not act as strong agonists.
With some weak agonists (ADP and epinephrine), the platelet aggregation curve may have a biphasic appearance - an initial wave of aggregation (primary wave), followed by a secondary wave of aggregation, which is usually irreversible. At higher ADP concentrations, the two waves of aggregation merge and there is no biphasic signal.
The aggregation response to the agonist is enhanced by the release of TxA2 from membrane phospholipids and the secretion of ADP from dense granules. ADP and TxA2 are agonists that, interacting with their specific receptors, enhance the platelet aggregation reaction.
Working concentrations of the agonists used and their mechanism of action:
| Agonist | Working concentration (C) | Mechanism of action |
| ADF | Low –1.0 μM, 2.5 μM, 5.0 μM High – 10.0 μM | ADP binds to its receptor on the surface of platelets. Initial binding results in the release of intracellular calcium and a change in platelet shape, leading to the formation of a primary wave of aggregation. The secondary wave reflects the release of ADP from platelet storage granules. A low dose of ADP causes only primary aggregation and its effect is reversible. ADP binds to two G-protein receptors P2Y1 and P2Y12. Binding of ADP to the P2Y1 receptor causes a shape change and initiates platelet aggregation (primary wave) by mobilizing calcium. The P2Y12 receptor is considered the main ADP receptor and is responsible for complete platelet aggregation through inhibition of adenyl cyclase. The P2Y12 receptor is also a target of clopidogrel. The second wave of ADP-induced aggregation is suppressed by aspirin and NSAIDs. |
| Adrenalin | 5μM, 10μM | Epinephrine binds to the α2-adrenergic receptor on the surface of platelets, resulting in inhibition of adenyl cyclase and the release of calcium ions. Platelet aggregation with epinephrine is visually similar to aggregation with ADP, with an initial primary wave of aggregation, release of stored ADP from platelets, and a second wave of irreversible aggregation. As with ADP, this second wave of aggregation is inhibited by aspirin and NSAIDs. Adrenaline, like ADP, is considered a weak agonist. |
| Ristocetin | Low –0.5 mg/mL High –1.5 mg/mL,5 mg/mL | Ristocetin in high concentrations causes platelet agglutination through von Willebrand factor and the GPIb-IX-V complex. |
| Collagen | 1.4μg/mL | Collagen binds to the GPVI and GPIa/IIa receptors, inducing the release of granule contents, the TXA2 pool, and then leads to sustained activation of GPIIb-IIIa. The GPIa/IIa receptor is involved in platelet adhesion. The GPVI receptor is involved in platelet signaling and TxA2 generation. The lag phase is formed after the addition of collagen to PRP, usually in less than 1 min. |
| Arachidonic acid | 500μg/mL | Arachidonic acid is a precursor of TxA2 in platelets. Arachidonic acid is converted to TxA2 with the participation of cyclooxygenase and thromboxane synthetase. TxA2 is a potent inducer of platelet aggregation, causing the release of granules, the formation of even greater generation of TxA2 and then the sustained activation of GPIIb-IIIa receptors. |
| Thrombin | Low –50 nmol/L High – 100 nmol/L | Thrombin is the most potent physiological platelet activator, acting on the PAR1 and PAR4 receptors. Thrombin causes platelet aggregation even at low concentrations, this does not lead to complete aggregation, but it changes the shape of platelets. At higher concentrations, thrombin induces complete platelet aggregation. |
Abbreviations used: PRP - platelet-poor plasma, PRP - platelet-rich plasma, TxA2 - thromboxane A2, C - concentration, GP - glycoprotein.
View of the classic two-phase platelet aggregation curve:
With the introduction of adrenaline and low doses of ADP, a biphasic aggregation curve is usually formed, while with the introduction of other agonists, or at high concentrations of inducers, a merger of the first and second waves is possible. In biphasic aggregation, the second wave is associated with the release reaction of platelet granules.
Aggregation parameters.
The main parameters of the aggregogram can be interpreted only after a preliminary assessment of platelet activity according to the types of aggregator curves (reversible, biphasic, irreversible and no platelet aggregation).
The main parameters of the aggregogram are the intensity of primary ( Tpa ), secondary ( Twa ), maximum aggregation ( Tma ) and disaggregation ( Tda ). The dynamics of the aggregation process on the graph should be judged by the slope angles of the aggregogram curve at the stage of primary aggregation ( α1 ), secondary aggregation ( α2 ) and disaggregation (β ). A characteristic of the dynamics of the reaction of release of endogenous stimulators of platelet aggregation is the latent period for collagen-induced aggregation ( tlp ) and the time of onset of secondary aggregation ( twa ) is normal for biphasic aggregation curves (high doses of ADP and adrenaline).
For collagen-induced aggregation, it is also important to evaluate the shortening or lengthening of the latent period ( tlp ) compared to the value of this indicator in healthy people.
A qualitative assessment of the aggregogram allows not only to diagnose hyper- or hyporeactivity of platelets, but also to suggest the causes of their occurrence. To quantitatively register various types of aggregation diagrams, the following indicators should be calculated:
- with irreversible aggregation - Tma, Tpa, Tda, Tba, α1, α2, of which the most informative are Tba, α2 and Tba;
- with reversible aggregation - Tma and Tda.
Fluctuation range of the main indicators of the aggregation diagram:
| Aggregogram parameters | Range of changes | Aggregogram parameters | Range of changes |
| Tma | 30-50% | Tva | 30-45 s |
| Twa | 30-40% | α1 | 60-75º |
| Tda | 60-80% (of Tpa value) | α2 | 60-75º |
| Tpa | 10-20% | β | 30-45º |
| tlp | 25-30 s | ||
Reference values
Normal aggregation activity when using inductors is:
- Platelet aggregation with ADP (5.0 µmol/ml): 60-90%
- Platelet aggregation with ADP (0.5 µmol/ml): 1.4-4.3%
- Platelet aggregation with adrenaline: 40-70%
- Platelet aggregation with collagen: 50-80%
Data interpretation
| Tentative diagnosis | Changes in the aggregogram |
| Glanzmann's thrombasthenia or afibrinogenemia | Absence or significant decrease in aggregation upon stimulation with any agonists except ristocetin |
| Bernard-Soulier syndrome or von Willebrand disease | Absence or significant reduction of aggregation with ristocetin |
| Storage pool violation | Primary wave of aggregation with only ADP, adrenaline and collagen. |
| Action of aspirin or aspirin-like effect | No aggregation with arachidonic acid. Presence of a primary wave only with ADP. Decreased or absent aggregation with collagen. |
| Effect of clopidogrel | No aggregation with ADP |
| Type 2B von Willebrand disease (VWD) or platelet type VWD | Aggregation with low dose of ristocetin (0.5 mg/ml) |
Link to the manual “Clinical and laboratory diagnosis of platelet function disorders”. Vasiliev S.A., Berkovsky A.L., Melkumyan A.L., Suvorov A.V., Mazurov A.V., Kozlov A.A. Federal State Budgetary Institution Hematological Research Center, Ministry of Health of the Russian Federation, Moscow, 2013.
When preparing this section, data from the scientific website www.practical-hemostasis.com was used.
How to prepare for submitting biomaterial?
The study of platelet aggregation is carried out strictly on an empty stomach, with a minimum interval of 6 hours after the last meal. 24 hours before the visit to the laboratory, the following are excluded: alcohol intake, sports training and psycho-emotional stress. Smoking should be stopped for 3 hours before blood collection.
If you are taking medications, you should consult your doctor in advance. Since drug exposure significantly changes the indicator and can lead to false results. You should not independently adjust the timing of taking medications and cancel them at your own discretion.
Features in children
Despite the fact that increased aggregation capacity is usually found in the adult population, recently there has been an increase in cases of the disease in children.
Hyperaggregation can be either hereditary or acquired. The causes of elevated platelet levels are not much different in adults. Mainly:
- diseases of the circulatory system;
- infectious and viral diseases;
- surgical intervention.
- In children under one year of age, hyperaggregation can be caused by dehydration and anemia. In adolescence, stressful situations and physiological growth of the body play an important role.
- Hypoaggregation in children manifests itself in the form of nosebleeds and bruises. Girls in adolescence may experience heavy periods. In 100% of cases, pinpoint rashes are observed on the skin, and 20% of children experience bleeding gums.
Treatment begins with finding out the cause of the deviation from the norm in platelet aggregation ability. Sometimes adjusting your diet and drinking regime is enough. In some cases, treatment of the disease that caused the abnormality is required.
Platelets in child tests:
If necessary, a hematologist will conduct an additional examination and prescribe medication according to the patient’s age and severity of the disease.
Reasons for deviation of the indicator from the norm
To fully understand the reasons for the deviation of the indicator from the norm, we will consider the reasons for each method separately.
ADP more than 85%
Indicators of aggregation with adenosine triphosphate that are overestimated by more than 85% are recorded when:
- coronary heart disease, in which there is a disruption in the normal blood supply to the cardiac myocardium. One of the causes of the pathology is arterial thrombosis. In this case, platelets begin to stick together without the influence of external factors and damage to blood vessels, clogging the lumen of the vascular bed and disrupting the normal blood flow (when a blood clot breaks off, a heart attack or ischemic stroke develops). After blocking 75% of the lumen of an artery, a person experiences a decrease in blood flow to the organ. Which naturally causes a lack of incoming oxygen, tissue hypoxia and organ atrophy. The pathology is characterized by a chronic course and steady progress. Competent therapy can slow down pathological damage to the myocardium;
- acute stage of myocardial infarction, as one of the clinical forms of coronary heart disease. The stage is characterized by necrosis (death) of an entire section of the myocardium;
- blood hypercoagulation syndrome can be physiological in nature or develop with combined pathologies. In other words, the syndrome is referred to as “blood thickening.” It is a normal option for pregnant women after the 2nd trimester. In non-pregnant women and men, indicates the development of pathological processes;
- inflammation of internal organs of various localization and etiology.
The reason for the increased degree of aggregation in a sample with collagen or ristomycin (more than 85%) is hyperaggregation syndrome.
Platelet aggregation with adrenaline is increased (more than 81%) in coronary heart disease, acute myocardial infarction, as well as against the background of extensive injuries and stress overexertion.
ADP reduction up to 65%
A decrease in platelet aggregation after exposure to ADP to 65% indicates:
- thrombocytopathy - combines various pathologies that arise due to the inability of platelets to activate and stick together, forming a primary thrombus and triggering a further cascade of hemostasis. According to statistics, every twentieth person has thrombocytopathy to varying degrees. The disease can be hereditary or acquired. In this case, the patient experiences a decrease in blood clotting, even with a normal platelet count;
- pathologies of the liver or kidneys, leading to impaired utilization of toxic substances. There is a deposition of toxic substances that interfere with the normal physiological activity of platelets;
- disturbances in the functioning of the endocrine system, in particular, excessive activity of the thyroid gland.
Low values of the indicator in a test with adrenaline (up to 61%) and collagen (up to 65%) are detected with thrombocytopathy and taking medications with anti-inflammatory activity.
The reason for the decrease in the rate in the study with ristomycin to 65% is von Willebrand disease.