Increased aggregation is a marker of hyperaggregation syndrome and thrombophilia. The most commonly used are the Born turbidimetric method, based on recording changes in the light transmission of platelet-rich plasma, and the method for studying platelet aggregation, based on the analysis of light transmission fluctuations caused by a random change in the number of particles in the optical channel.
Material for research.
Citrate platelet rich plasma
Research method
is determined by the operating procedure on a particular type of aggregometer.
Solutions of ADP, ristocetin, collagen, adrenaline, and arachidonic acid are most often used as inducers. Solutions of thrombin, serotonin, etc. can also be used.
Platelet aggregation with ADP
Exposure to small doses of ADP (usually 1*10-7 mol) leads to the formation of a double wave of aggregation. The first phase (primary wave) depends on added exogenous ADP, and the second phase (secondary aggregation wave) occurs due to the release reaction of intrinsic agonists contained in platelet granules. Large doses of ADP (usually 1*10-5 mol) lead to the merging of the first and second waves of aggregation.
When analyzing aggregograms, attention is paid to the general nature of aggregation (single-wave, two-wave; complete, incomplete; reversible, irreversible) and the rate of aggregation. The appearance of two-wave aggregation upon stimulation of ADP at concentrations that normally cause reversible aggregation (usually 1-5 µmol) indicates an increase in platelet sensitivity, and the development of single-wave incomplete (and often reversible) aggregation upon stimulation of ADP at concentrations of 10 µmol or more indicates an increase in platelet sensitivity. impaired platelet release reaction.
Platelet aggregation with ristocetin
Determination of platelet aggregation with ristocetin in plasma is used to quantify von Willebrand factor. The method is based on the ability of ristocetin to stimulate in vitro the interaction of von Willebrand factor with platelet glycoprotein Ib. In most cases of von Willebrand disease, there is a violation of ristocetin aggregation with a normal response to the effects of ADP, collagen and adrenaline. Disturbances in ristocetin aggregation are also detected in Bernard-Soulier disease. For differentiation, a test with the addition of normal plasma is used: in von Willebrand disease, after the addition of normal plasma, ristocetin aggregation is normalized, while in Bernard-Soulier syndrome this does not happen. Ristocetin-induced platelet agglutination is reduced in most cases of von Willebrand disease, except type IIB.
To assess the platelet component of hemostasis, the number of platelets in the blood is counted. Platelet pathology is the cause of bleeding in almost 80% of cases. Thrombocytopenia is its most common manifestation. Thrombocytopenia should be diagnosed in cases where the platelet count is less than 150 × 109/L. The duration of bleeding is an important screening test, the main advantage of which is that it allows you to simultaneously qualitatively assess the number of platelets in the blood, their adhesive and aggregation functions, the functional properties of the blood vessel wall, as well as a pronounced deficiency of plasma coagulation factors (for example, factors VIII and IX, the deficiency of which is the cause of hemophilia A and B). Prolongation of bleeding time reflects a violation of hemostasis due to thrombocytopenia, thrombocytopathies (impaired platelet functions - adhesion and aggregation), disorders of the vascular wall, or a combination of these factors. Prolongation of bleeding time with a normal number of platelets in the blood suggests a violation of their functions. This is the main value of the test, because... To assess the adhesive and aggregation properties of platelets in laboratory conditions, complex and expensive equipment (aggregometer) is required. When platelet function is not impaired, bleeding time remains normal even when the platelet count drops to 100.0 x 109/L. Below this level, the bleeding time gradually increases in a linear relationship with the platelet count. Spontaneous bleeding occurs if the platelet count falls below 50.0 x 109/L; fatal bleeding is almost inevitable if the platelet count drops to 5.0 x 109/L. The duration of bleeding increases under the following conditions:
- Severe thrombocytopenia;
- Impaired platelet function - thrombocytopathies, which can be congenital (Bernard-Soulier syndrome) and acquired (pernicious anemia, acute and chronic leukemia, multiple myeloma, long-term use of aspirin);
- Marked decrease in plasma coagulation factors;
- If the resistance of the capillary wall is impaired (lack of vitamin C, defects in capillary contraction - microangiopathies).
A shortening of bleeding time has no diagnostic significance and is most often the result of a technical error during the test or indicates an increased spasticity of the capillaries. It is impossible to assess the susceptibility to thrombus formation using the bleeding duration test. An increased number of platelets in the blood - thrombocytosis, carries with it the risk of increased coagulation and is manifested by thrombosis. In clinical situations, the risk of thrombosis becomes real if the platelet count reaches 1000.0 x 109/L.
Study of platelet aggregation functions Aggregation processes are studied using an aggregometer, which reflects the progress of aggregation graphically in the form of a curve; ADP, adrenaline and collagen are often used as aggregation stimulators.
Disorders of platelet aggregation in various diseases (according to the results of studies using an aggregometer)
| Type of thrombocytopathies | Aggregation stimulator and aggregation disorder | ||||
| ADF | collagen | adrenalin | ristocetin | ||
| primary wave | secondary wave | ||||
| Thrombasthenia | Pathology | Pathology | Pathology | Pathology | Norm |
| Essential atrombia | Pathology | Pathology | Pathology | Pathology | Norm |
| Aspirin-like defect | Norm | Pathology | Pathology | Pathology | Norm |
| Bernard-Soulier syndrome | Norm | Norm | (+,-) | (+,-) | Norm |
| Wiskott-Aldrich syndrome | Pathology | Pathology | Pathology | Pathology | Norm |
| von Willebrand disease | Norm | Norm | Norm | Norm | Reduced pathological |
Note: (+,-) – has no diagnostic value.
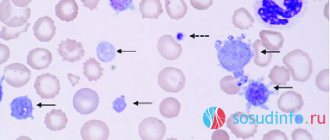
Platelet pathology is the cause of bleeding in almost 80% of cases. Thrombocytopenia is its most common manifestation. Thrombocytopenia should be diagnosed in cases where the platelet count is less than 150 × 109/L. There are acute and chronic thrombocytopenia. The latter is diagnosed when its duration exceeds 6 months. Individuals with platelet levels above 50×109/L rarely experience bleeding. However, a decrease in platelets below 100×109/L can accompany serious pathology. In this regard, the cause of each case of thrombocytopenia must be clarified. With thrombocytopenia, severe thrombocytopathies and von Willebrand factor (VWF) deficiency, the bleeding time is significantly prolonged. Bleeding is associated with insufficiency of the adhesive-aggregation function of platelets - a violation of the formation of a platelet plug in damaged vessels. This may be due to either a significant decrease in the number of platelets in the blood, or their dysfunction, which is most often based on the absence or blockade of receptors on the platelet membrane that interact with stimulators (agonists) of aggregation of these cells (VWF, adrenaline, ADP, fibrinogen, arachidonic acid and prostaglandins), or the absence in platelets or a violation of the release from them of granule components containing these aggregation stimulants. Modern hematology analyzers display thrombocytometric curves (histograms of platelet distribution by volume). There is a connection between the size of platelets and their functional activity, the content of biologically active substances in platelet granules, the tendency of cells to adhere, and changes in platelet volume before aggregation. The presence of predominantly young forms of platelets in the blood leads to a shift of the histogram to the right; old cells are located in the histogram on the left, since as platelets age, their volume decreases. An increase in the content of young forms of platelets is observed during blood loss and indicates enhanced regeneration. An increase in the content of old forms, vacuolated platelets, forms of irritation and a decrease in the content of mature platelets are characteristic of various inflammatory processes, intoxications, and malignant neoplasms.
Thrombomodulin is an integral membrane protein, a thrombin receptor located on endothelial cells of blood vessels and involved in the anticoagulation system. It determines the speed and direction of the hemostasis process, actively limits and regulates blood clotting. The endothelium, forming thrombomodulin, blocks active coagulants secreted by the liver and found in the blood plasma, primarily the most active coagulation factor, thrombin. Bound thrombin is excluded from the blood coagulation system. Thrombin, having joined thrombomodulin, acquires new qualities: together with the anticoagulant proteins C and S (protein S cofactor), it forms an antiplatelet and antithrombotic complex, which prevents coagulation and inhibits fibrinolysis. Thus, the thrombomodulin-protein C system performs an anticoagulant function. Moreover, thrombin, modified by interaction with thrombomodulin, loses the ability to convert fibrinogen into fibrin and cause platelet aggregation. When the vascular wall is damaged, thrombomodulin is “separated” from the endothelium and enters the blood. Its increase in the blood is observed in patients with prethrombotic conditions, vasculitis, etc. The degree of increase in thrombomodulin in the blood has diagnostic and prognostic significance. Thrombomodulin is significantly reduced in some diseases, such as atherosclerosis, which can increase blood clotting and increase the risk of thrombosis.
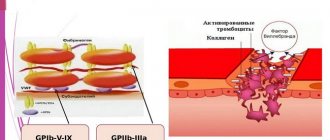
Factor B illebrand is a complex multimeric adhesive glycoprotein, a carrier-stabilizer of the procoagulant protein F VIII:C, which is an adhesion protein in the processes of hemostasis. Von Willebrand factor can bind collagen and possibly other endothelial structures and mediates platelet adhesion to the subendothelium through binding of the platelet surface receptor glycoprotein Ib. Von Willebrand Factor-mediated platelet adhesion occurs most intensely at high shear rates, i.e. in the arteries. VIII-vWF is also a carrier of F VIII - antihemophilic globulin A. Von Willebrand factor in healthy people prevents the growth of blood clots in blood vessels by activating the formation of plasmin. Elevated levels of von Willebrand factor activity are an indicator of endothelial damage in vascular disease, which may be significant for hypertensive vascular complications. Von Willebrand disease is a congenital hemorrhagic diathesis. In its mild form, this disease is the most common hemorrhagic disorder in men, with an incidence of 1:100. This is a disease of a heterogeneous nature, caused either by defects in protein structure or by a decrease in the concentration of von Willebrand Factor. Classification of the disease is based on the clinical picture, history and laboratory results, including clotting time and determination of antigen and von Willebrand factor activity. Determining the level of Von Willebrand Factor helps in the differential diagnosis of two main types of disease: type 1 and type 2. Determining the type of disease is important, since the choice of patient management tactics depends on it.
Fibronectin is a receptor for fibrin-stabilizing factor. Promotes platelet adhesion by participating in the formation of a white blood clot; binds heparin. By joining fibrin, fibronectin thickens the blood clot. Under the influence of fibronectin, smooth muscle cells, epithelial cells, and fibroblasts increase their sensitivity to growth factors, which can cause thickening of the muscular wall of blood vessels (narrowing of diameter).
Platelet aggregation with collagen
Platelet aggregation with collagen has a fairly pronounced latent phase, during which phospholipase C is activated. Depending on the concentration of the reagent used, the duration of this phase can be 5-7 minutes. After the end of this period, processes occur in platelets that lead to the formation of second messengers, as a result of which the secretion of platelet granules and the synthesis of thromboxane A2 develop, which is accompanied by a sharp increase in interplatelet interaction.
In laboratory and clinical practice, collagen is most often used in a final concentration of 50 μg/ml, however, collagens from different companies may have different activities, which must be taken into account when using them.
Induced aggregation with adrenaline
Description Platelets play a significant role in human life: they prevent blood loss by connecting with each other on the wall of a damaged vessel. This process of platelets sticking together is called aggregation. It is important that this parameter does not deviate from the normal values, otherwise this is fraught with blood loss or the formation of a blood clot that can block the entire diameter of the vessel and lead to tissue death.
It is important that this parameter does not deviate from the normal values, otherwise this is fraught with blood loss or the formation of a blood clot that can block the entire diameter of the vessel and lead to tissue death.
Platelet aggregation: what is it?
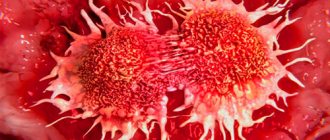
The process of platelet aggregation into conglomerates is as follows: when a vessel is injured, platelets combine with von Willebrand factor and collagen of the subendothelial layer.
Aggregation of platelets with collagen causes activation of red blood cells, and they become sources of components that stimulate aggregation: thromboxane and serotonin. Platelet disaggregation is the reverse of aggregation.
Platelet aggregation is a protective function of the body, but it is also subject to the influence of pathological reactions.
On the one hand, platelet aggregation saves us from excess blood loss, which is important during surgical operations, major injuries and childbirth; on the other hand, hyperaggregation leads to the formation of a blood clot.
Blood clots are very dangerous: their movement through the circulatory system into the heart, brain or pulmonary artery can lead to rapid death. The study of platelet aggregation takes into account their ability to connect: with deviations above the norm, a heart attack or stroke may occur, below the norm - blood loss, anemia, exhaustion.
What is platelet aggregation in the blood? To determine the value of platelet aggregation, it is necessary to take a blood test from a vein into a test tube, and in this case, when there is no wound, it is necessary to create conditions for the combination of platelets into a conglomerate.
For this purpose, induced platelet aggregation is introduced in the laboratory.
Conditions become as close as possible to the body’s environment; substances identical in chemical composition to human substances that can cause thrombus formation are taken as an inducer of platelet aggregation.
Inductors can be:
- Serotonin.
- Collagen.
- Adrenalin.
- Arachidonic acid.
- Adenosine diphosphate (ADP).
The way to measure platelet aggregation is to pass light through the blood plasma.
The difference between the light density of plasma before blood clotting and after clot formation is the aggregation activity of platelets. Additionally, the rate of platelet aggregation in 1 minute, the shape and type of waves are determined.
Spontaneous platelet aggregation is calculated without the use of an inducer.
Degree of platelet aggregation:
- norm with ADF – 30.7 – 77.7%
- with collagen – 46.4 – 93.1%
- with adrenaline – 35 – 92.5%
Preparing for the test
A reliable assessment of the result can be obtained if the following conditions are met: Do not eat 12 hours before the test. The day before blood sampling, do not perform physical activity or experience emotional turmoil.
7 days before the test, stop taking a number of medications (if this is not possible, then inform the nurse).
The day before the test, avoid alcohol, smoking, garlic and coffee. Come to donate blood healthy, without inflammation in the body.
Deviation from the norm
A decrease in platelet aggregation can occur for the following reasons:
- The presence of thrombocytopathy.
- Treatment with antiplatelet drugs.
Thrombocytopathy is a disease in which platelet functions (clotting, thrombus formation) are impaired. The disease manifests itself by the presence of bruises and bleeding, which subsequently leads to anemia.
If platelet aggregation is reduced, then drug treatment is prescribed, which should be carried out by a qualified specialist.
Increased platelet aggregation can occur with:
- Hypertension.
- Atherosclerosis of joints.
- Stroke and heart attack.
- Diabetes mellitus.
- Thrombosis.
If platelet aggregation is increased, then conservative therapy with the use of antiplatelet agents cannot be avoided. Be sure to visit a doctor to get tested and receive treatment recommendations.
During pregnancy, deviations from normal platelet aggregation values are possible.
A reduced level indicates the danger of bleeding, an increased level indicates toxicosis as a result of loss of fluid from the body and is fraught with miscarriage.
During pregnancy, the degree of platelet aggregation: the norm is 30-60% for any inducer. A platelet aggregation test is prescribed in cases of complicated pregnancy, poor medical history, and before planned conception.
Platelet aggregation with adrenaline
Adrenaline, upon contact with platelets, interacts with α2-adrenergic receptors, which causes inhibition of adenylate cyclase. It is possible that the mechanism underlying the implementation of the effect of adrenaline and the development of the first wave of aggregation does not depend on the formation of thromboxane A2, the release reaction or the synthesis of platelet aggregation factor, but is associated with the ability of adrenaline to directly change the permeability of the cell membrane to calcium ions. The second wave of aggregation occurs as a result of the release reaction and production of thromboxane A2.
What is “platelet aggregation”
Platelets are colorless blood cells whose function is to protect the body from blood loss. When body tissues are damaged, platelets immediately rush to the site of injury and block it, preventing excessive blood loss. This blocking occurs due to the fact that platelets instantly stick together and form a block that closes the wound. This blocking process is called platelet aggregation. The process occurs in two stages:
- Blood cells stick together
- Later they adhere to the walls of the vessel, forming a blood clot or thrombus.
When the body is healthy, this function is protective. But if pathological changes occur in the body, the formation of blood clots can disrupt nutrition in vital organs and tissues.
Platelet aggregation with arachidonic acid
Arachidonic acid is a natural aggregation agonist, and its action is mediated by the effects of prostaglandins G2 and H2, thromboxane A2, and includes activation of both phospholipase C with subsequent formation of second messengers, mobilization of intracellular calcium and expansion of the cell activation process, and phospholipase A2, which directly leads to release of endogenous arachidonic acid. Platelet aggregation with arachidonic acid occurs quite quickly, so the curve characterizing this process is often single-wave in nature.
To induce aggregation of blood platelets, arachidonic acid is used in concentrations of 10-3-10-4 mol. When working with arachidonic acid, it should be taken into account that in air this substance oxidizes very quickly.
An aggregation test with arachidonic acid is recommended in cases of using drugs that affect the aggregation reaction (for example, acetylsalicylic acid, penicillin, indomethacin, delagil, diuretics), which must be taken into account when assessing the research results.