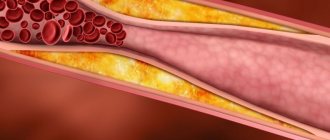
Hypercholesterolemia is a disease in which the level of cholesterol in the blood rises to pathological levels. From the point of view of normal physiology, this compound is important and useful. Normally, most of it is produced by the body (up to 80%). Cholesterol ensures the stability of cell membranes and is involved in the synthesis of vitamins, bile acids, and hormones. However, with hypercholesterolemia, its level increases, it is deposited on the walls of blood vessels, affects metabolic processes and leads to the development of serious complications, including heart attack, stroke, hypertension, etc.
Classification
Most often in clinical practice, the Frederickson classification of hypercholesterolemia is used, which is based on the division according to the predominance of one or another cholesterol fraction:
- Type I – increased concentration of chylomicrons (CM).
- Type IIa – increased levels of low-density lipoproteins (LDL).
- Type IIb – high content of low and very low density lipoproteins (VLDL and LDL).
- Type III – increased levels of intermediate density lipoproteins (IDL).
- Type IV – increased VLDL values.
- Type V – high level of VLDL and cholesterol.
Based on its origin, hypercholesterolemia is divided into:
1. Primary
. This form is in turn divided into:
- Polygenic. The most common variety. Caused by a combination of genetic predisposition and exposure to exogenous factors (diet, smoking, etc.).
- Family. Caused by various hereditary disorders of lipid metabolism due to genetic mutations.
2. Secondary
. High levels of cholesterol in the blood, which develops against the background of certain diseases, endocrine disorders, or taking medications.
Based on the degree of increase in blood cholesterol levels, the following are distinguished:
- Mild hypercholesterolemia
– from 5.0 to 6.4 mmol/l. - Moderate hypercholesterolemia
– from 6.5 to 7.8 mmol/l. - High hypercholesterolemia
– 7.9 mmol/l and above.
Signs and symptoms
Hypercholesterolemia is detected using a laboratory blood test for biochemistry. In addition, there are some external signs by which the presence of this pathology can be determined. The main one is the presence of xanthomas - skin neoplasms formed from pathologically altered cells consisting of lipid inclusions.
They look like dense nodules. Xanthomas accompany all forms of the pathology in question and are one of the external signs of fat imbalance. They do not cause unpleasant or painful sensations in a person. They can dissolve on their own.
How to donate blood for cholesterol?
The following classification of xanthomas is distinguished:
- Tuberous - large plaques are located in the elbows, buttocks, knees, on the back of the fingers, scalp and on the face and have a brown or purple tint with a cyanotic or reddish border.
- Eruptive - small yellow papules. They tend to appear on the buttocks and thighs.
- Tendon - localized mainly in the tendon area.
- Flat – spots of a light orange hue rise slightly above the surface of the skin. In most cases they appear on the palms.
- Xanthelasmas are flat yellow xanthomas of the eyelids. Occurs predominantly in women. They do not disappear on their own.
Another sign of hypercholesterolemia is the appearance of peculiar cholesterol deposits along the border of the cornea of the eyes. They have the shape of a grayish-white or white rim and in medical practice are called lipoid arcs. It appears more often in people who smoke. It is irreversible.
Persons with this sign of hypercholesterolemia are at risk for developing coronary artery disease. With homozygous familial hypercholesterolemia, a significant increase in blood cholesterol levels is observed. In people with this form of pathology, symptoms and signs of the disease develop already in childhood.
During puberty, they often experience atheromatous lesions of the aortic mouth, as well as narrowing of the lumen of the coronary arteries of the heart. They also experience all the clinical manifestations of IHD. The cause of premature death in this case is often acute coronary insufficiency.
The heterozygous form of hereditary hypercholesterolemia has a long and asymptomatic course. Cardiovascular insufficiency manifests itself only in adulthood. According to statistics, the first signs of pathology appear earlier in women by about 10 years than in men.
A long-term increase in blood cholesterol levels over many years, accompanied by such phenomena as arterial hypertension, diabetes mellitus, and smoking, accelerates the formation of atherosclerotic plaques on blood vessels. They narrow the lumen to the point of complete blockage. This, in turn, is fraught with deadly consequences.
These are the main external signs of hypercholesterolemia
Causes of hypercholesterolemia
Physiological
Cholesterol values can also exceed normal levels in healthy people. For example, changes in the balance of female sex hormones during pregnancy cause an increase in cholesterol levels. After childbirth, the indicators return to normal. In case of improper preparation before taking a biochemical blood test (eating fatty foods on the eve of blood donation), cholesterol turns out to be higher than normal.
Hereditary disorders of lipid metabolism
This group of diseases is called “hereditary (familial) hypercholesterolemia.” They are caused by mutations in genes encoding the expression of lipoprotein receptors (LDLR, ApoB-100, PCSK9) or the lipoprotein lipase enzyme. This leads to disruption of catabolism and absorption of lipoproteins by cells, as a result of which the concentration of cholesterol in the blood begins to increase significantly.
A distinctive feature of familial forms of hypercholesterolemia is the detection of very high levels of cholesterol (in homozygous patients it can reach 20 mmol/l) already from early childhood (5-7 years). All this is associated with the rapid progression of atherosclerosis and the development of serious cardiovascular complications already at 20-25 years of age. Aggressive lipid-lowering therapy is required to normalize cholesterol levels.
Xanthelasma on the eyelids is a sign of hypercholesterolemia
Obesity
Excess weight ranks first among the etiological factors of hypercholesterolemia and accounts for more than 90% of all its cases. The pathogenesis of the effect of excess weight on cholesterol levels is as follows. Adipocytes secrete a large amount of biologically active substances that reduce the sensitivity of cells to insulin, and insulin resistance is formed.
As a result, lipolysis and the release of free fatty acids (FFA) are activated. From excess FFA entering the liver, a large amount of VLDL, one of the cholesterol fractions, is synthesized. Hypercholesterolemia increases slowly and is directly proportional to the degree of obesity; it can gradually return to normal with weight loss, but over a long period of time it becomes irreversible.
Kidney diseases
The cause of hypercholesterolemia can be kidney diseases accompanied by nephrotic syndrome: the initial stage of glomerulonephritis, diabetic or hypertensive nephropathy, nephropathy with multiple myeloma. An increase in cholesterol levels is associated with the loss in urine of carrier proteins and enzymes involved in lipid catabolism (lecithin-cholesterol acetyltransferases, lipoprotein lipases).
The severity of hypercholesterolemia correlates with the degree of proteinuria. After specific therapy for the underlying disease and relief of nephrotic syndrome, cholesterol levels usually normalize, but in some cases they remain elevated for a long time, which may require additional therapeutic measures to prevent the progression of atherosclerosis.
Endocrine disorders
Diseases of the endocrine system occupy a special place in the structure of the causes of hypercholesterolemia. Insufficiency or excess production of a particular hormone causes significant changes at different stages of lipid metabolism.
- Diabetes mellitus type 2.
The most common cause among endocrine diseases. The mechanism of development of hypercholesterolemia is the same as in obesity (relative insulin deficiency, increased synthesis of VLDL). The degree of increase in cholesterol corresponds to the severity of diabetes. To normalize indicators, both antidiabetic and lipid-lowering therapy are necessary. - Hypothyroidism.
Thyroxine and triiodothyronine stimulate the formation of VLDL receptors and regulate the activity of cholesterol-7-alpha-hydroxylase, the main enzyme in the synthesis of bile acids. A decrease in the concentration of thyroid hormones in hypothyroidism leads to a slowdown in the catabolism of VLDL and the conversion of cholesterol into bile acids. Hypercholesterolemia is moderate, completely reversible. Disappears along with other symptoms of the disease after hormone replacement therapy. - Cushing's disease/syndrome.
Primary and secondary hypercortisolism increase cholesterol levels both directly (adrenocortical hormones and glucocorticosteroids reduce the number of VLDL receptors) and indirectly (through the development of steroid-induced diabetes mellitus). Hypercholesterolemia is more pronounced and more persistent than with hypothyroidism.
Cholestasis
An increase in serum cholesterol levels can be observed in diseases of the liver and biliary tract, accompanied by intra- or extrahepatic cholestasis (stagnation of bile). Hypercholesterolemia is caused by impaired utilization of cholesterol for the production of bile acids. Its degree correlates with the severity of cholestasis.
The highest rates are observed in primary sclerosing cholangitis, primary and secondary biliary cirrhosis, less pronounced in parenchymal liver diseases (alcoholic, viral hepatitis, fatty liver). Elimination of cholestasis leads to a fairly rapid normalization of cholesterol.
Other reasons
- Autoimmune diseases:
systemic lupus erythematosus, hypergammaglobulinemia. - Metabolic disorders:
gout, storage diseases (Gaucher disease, Niemann-Pick disease). - Mental illness:
anorexia nervosa. - Taking medications:
oral contraceptives, beta-blockers, thiazide diuretics.
4.Treatment
In fact, the only way to medically influence the concentration of cholesterol in the blood (in the direction of reducing it) are drugs from the pharmacological group of statins. However, to date, extensive medical and statistical material has been accumulated, which reliably indicates, firstly, the insufficient effectiveness of these drugs (the so-called residual cardiovascular risk with such therapy remains at the level of 60-70%), and secondly, the unacceptably high likelihood of complications and side effects, incl. very heavy.
Therefore, one of the primary tasks of modern research medicine is the search and testing of alternative, more effective and safe ways to control the concentration of both total cholesterol and its individual fractions.
However, statins in any case play the role of ultima ratio (“last argument”), which should be resorted to only if there is no effect from all other measures. They always begin with examination and treatment of identified pathology, often latent or asymptomatic (chronic somatic diseases, endocrine-metabolic disorders, etc.), with the most serious correction of lifestyle and daily diet, cycle of rest and stress (physical and mental); with normalization of body mass index and categorical refusal of harmful habits.
With this approach, pharmacotherapy will most likely not be needed.
Diagnostics
Laboratory hypercholesterolemia is detected by examining venous blood. In addition to the concentration of total cholesterol, the determination of its fractions and triglycerides is of great information. For differential diagnosis, the patient’s age and other anamnestic data are important - taking medications, the presence of close relatives with a confirmed familial form of hypercholesterolemia. To clarify the etiological factor, the following examination is carried out:
- Routine laboratory tests.
The content of liver transaminases (ALT, AST), markers of cholestasis (alkaline phosphatase, gamma-glutamyl transpeptidase), and glucose are measured. If nephrotic syndrome is suspected, a general urinalysis, analysis for microalbuminuria, and daily proteinuria are performed. - Hormonal studies.
The concentration of TSH and thyroid hormones (free T4 and T3) is determined. To confirm hypercortisolism, the level of cortisol in the blood is checked after performing small and large dexamethasone tests. - Immunological tests.
Tests are performed for markers of viral hepatitis (HBsAg, HCV), antimitochondrial (AMA), antineutrophil (ANCA) antibodies. - Ultrasound.
An ultrasound of the abdominal organs may reveal gall bladder stones, wall thickening, and signs of fatty infiltration in the liver. - Genetic research.
If hereditary hypercholesterolemia is suspected, mutations in the LDLR, PSCK-9, and ApoB-100 receptor genes are detected using the polymerase chain reaction.
For drug correction of hypercholesterolemia, different groups of drugs are prescribed
Causes and stages of development of pathology
Hypercholesterolemia occurs under the influence of certain causes and risk factors. This pathology has several varieties, which depend on its development mechanism. Primary hypercholesterolemia is hereditary in nature , transmitted from generation to generation, its first manifestations can occur in childhood due to the fact that the biochemistry of fat metabolism is disrupted at the genetic level.
The secondary form is a consequence of the patient’s existing ailments (decreased thyroid function, diabetes, liver pathologies).
The causes of hypercholesterolemia of alimentary origin are excessive human consumption of food rich in animals or hydrogenated fats, frequent consumption of simple carbohydrates (sweets, baked goods).
In addition to the above reasons, the failure of lipid metabolism with the subsequent addition of hypercholesterolemia is due to a number of provoking factors:
- presence of bad habits (abuse of alcoholic beverages, smoking hookah or cigarettes);
- lack of adequate physical activity;
- presence of excess kilograms:
- love of foods rich in fats (fast food, baked goods and flour products, lard, fatty cheeses, margarine or butter, sausages);
- being under conditions of chronic stress;
- lack of work and rest schedule;
- reaching adulthood;
- gender (females before menopause are less susceptible to hypercholesterolemia than males due to the hormonal characteristics of the body)
According to statistics, secondary or nutritional hypercholesterolemia is most common. The hereditary form of the disease is registered with a frequency of 1 sick person per 500 healthy people.
Correction
Conservative therapy
If hypercholesterolemia is detected, it is imperative to consult a doctor to find out the cause of this laboratory phenomenon and select appropriate treatment. Much attention is paid to the fight against the underlying disease (immunosuppressive therapy for nephrotic syndrome, hormone replacement therapy for hypothyroidism, choleretic therapy for cholestasis), since its elimination can lead to normalization of cholesterol levels without additional intervention.
Non-drug methods for correcting hypercholesterolemia include complete smoking cessation and limiting alcohol consumption. Also, in order to reduce body weight, obese patients must follow a diet with a decrease in the proportion of animal fats in the diet (butter, fried meat, sausages) and an increase in vegetable fats (vegetables, seafood), fruits and whole grains, and regularly perform various physical exercises.
For the drug correction of hypercholesterolemia, the following drugs are used:
- Statins
(atorvastatin, rosuvastatin). The most effective and frequently prescribed means to reduce cholesterol levels. The mechanism of action is based on the suppression of cholesterol synthesis in the liver. - Fibrates
(clofibrate). These drugs stimulate the activity of the LPL enzyme, thereby accelerating the degradation of the drug. They reduce not only cholesterol, but also triglycerides, so they often become the drugs of choice for patients suffering from diabetes. - Ezetimibe
. Inhibits the absorption of cholesterol in the intestine. Used in combination with statins. - PCSK9 inhibitors
(alirocumab). These are monoclonal antibodies that bind to LDL receptors in the liver, which stimulates the breakdown of lipoproteins. Prescribed when statins are ineffective. - Bile acid sequestrants
(cholestyramine, colestipol). They are ion exchange resins that suppress the absorption of bile acids in the intestine. Depletion of FA reserves activates their synthesis from cholesterol in the liver. Used in patients with cholestasis. - A nicotinic acid
. This drug reduces the flow of fatty acids into the liver, which suppresses the synthesis of lipid. It has a weak hypocholesterolemic effect, therefore it is used as an addition to other drugs. - Omega-3 fatty acids
. Eicosapentaenoic acid and docosahexaenoic acid are components of fish oil. These substances bind to the nuclear PPAR receptors of liver cells, which leads to a decrease in serum lipid levels.
Surgery
One of the prerequisites for the effective treatment of hypercholesterolemia is normalization of body weight. For patients with morbid obesity (body mass index above 40), especially in combination with type 2 diabetes mellitus, if conservative methods are unsuccessful, bariatric surgery is indicated - gastric banding, gastric bypass or resection.
If hypercholesterolemia is caused by cholestasis due to cholelithiasis, surgical removal of the gallbladder (cholecystectomy) is performed. Patients with Cushing's disease undergo endoscopic transnasal adenomectomy (removal of the pituitary adenoma). For Itsenko-Cushing syndrome, bilateral adrenalectomy is used.
Pathogenesis
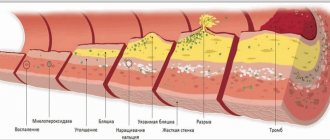
Lipoproteins whose diameter is less than 70 nm pass through the vascular endothelium. ApoB-containing lipoproteins in the arterial wall become trapped and trigger a process whereby lipids are deposited in the wall. Low-density lipoproteins are oxidized and, together with monocytes, form the core of an atherosclerotic plaque. The active substances released during this process are involved in the proliferation of smooth muscle cells in blood vessels and the breakdown of collagen. In patients with high levels of apoB-containing lipoproteins, more particles are deposited, and the atherosclerotic plaque progresses faster. Over time, other particles are deposited in the vessel wall, and the atherosclerotic plaque, reaching a critical point, ruptures with the formation of a blood clot on the surface. It becomes the cause of blockage of the vessel with the development of angina or myocardial infarction .
Dyslipidemia develops with
insulin resistance .
Under conditions of increased insulin secretion with decreased tissue sensitivity to insulin, increased breakdown of fats into fatty acids occurs. The latter are delivered to the liver, where they produce low-density lipoprotein cholesterol. Dyslipidemia causes increased blood pressure. The role of very low-density and low-density lipoproteins in the development of vascular endothelial dysfunction has been proven, which causes disruption of the synthesis of nitric oxide and an increase in the production of the vasoconstrictor peptide endothelin-1. As a result, vasoconstriction occurs and systemic blood pressure increases. Primary hyperlipidemia type 1 is associated with a mutation in the lipoprotein lipase gene. A defect in this enzyme blocks the metabolism of chylomicrons and they accumulate in large quantities in the plasma. With reduced lipoprotein lipase activity, triglycerides are not broken down and severe triglyceridemia .
Forecast
Hypercholesterolemia leads to the deposition of cholesterol on the walls of arterial vessels, the formation of atherosclerotic plaques, narrowing of the lumen and deterioration of blood supply to organs and tissues. This is of primary clinical importance for the coronary and cerebral arteries. Therefore, a long-term increase in cholesterol concentration is an unfavorable prognostic factor for cardiovascular diseases and is associated with such serious complications as acute myocardial infarction and acute cerebrovascular accident.
Prognosis and prevention
The prognosis for hypercholesterolemia largely depends on a number of factors:
- The level of pro-atherogenic and anti-atherogenic fat-like substances in the body (the former cause atherosclerosis, and the latter prevent this process).
- The degree of progression of atherosclerotic changes.
- Location of atherosclerotic formations in the vessel. Atherosclerosis of the aorta has a more favorable course, while atherosclerosis of the native arteries of the heart has a less favorable prognosis.
Elimination of risk factors for increased cholesterol levels, as well as timely and complete treatment, can significantly prolong the patient’s life without compromising its quality. Experts identify measures for primary and secondary prevention of hypercholesterolemia. Primary prevention involves taking action before the onset of pathology.
It involves influencing modifiable risk factors, in particular:
- getting rid of excess weight;
- diet;
- giving up cigarettes and alcohol;
- feasible physical activity;
- normalization of blood pressure;
- stabilization of blood sugar levels;
- limiting emotional turmoil.
Secondary prevention measures concern people who have already been diagnosed with hypercholesterolemia. They are aimed at preventing the progression of the pathological process and the development of complications.