© Author: Sazykina Oksana Yuryevna, cardiologist, especially for SosudInfo.ru (about the authors)
To begin with, it should be noted that bigeminy and trigeminy are variants of ventricular extrasystole . Extrasystole is one of the types of heart rhythm disturbances, which is characterized by the occurrence of ectopic heart rhythms. This concept reflects a condition in which contractions of the atria or ventricles do not occur in those pathways of the conduction system along which the normal conduction of impulses occurs. Extrasystole can be atrial or ventricular.
In cases where extrasystoles alternate with normal contractions of the heart through one contraction, they speak of cardiac bigeminy (1:1), and when after two normal contractions, they speak of ventricular trigeminy (1:2). Accordingly, one extraordinary contraction after three normal ones is called quadrigeminy (1:3), and after four - pentageminy. These types of extrasystole are united by the concept of allorhythmia.
bigeminy on the ECG: every second complex is an extrasystole
In addition, paired extrasystoles (two in a row) and frequent group extrasystoles are distinguished if they follow three or more in a row. In the latter case, the extrasystole can be regarded as a short jog of ventricular tachycardia.
According to statistics, extrasystole occurs in more than 68% of people. At the same time, the majority (63%) are ventricular extrasystoles, about 25% are atrial, and the remaining cases are supraventricular bigeminy and trigeminy, as well as their combinations. The occurrence of ventricular bigeminy is also noted in more than 60% of patients with myocardial ischemia and more than 80% of patients with acute myocardial infarction.
Causes of bigeminy and trigeminy
Ordinary single atrial and ventricular extrasystoles are normally found in a healthy person. They are practically not felt and do not cause discomfort. More frequent extrasystoles, such as allorhythmia, as well as frequent paired extrasystoles and runs of ventricular tachycardia, cannot be considered a variant of the norm and are a reason for a detailed examination of the cardiovascular system.
So, the main reasons for the occurrence of episodes of bigeminy and trigeminy are:
- Acute myocardial infarction,
- Overdose of cardiac glycosides, or so-called glycoside intoxication with digitalis and digitalis preparations - strophanthin, digoxin, korglykon, etc.
- Acquired defects of the mitral and aortic valves,
- Previous rheumatic fever (rheumatism) with damage to the inner lining of the heart - endocarditis,
- The consequences of myocarditis - an inflammatory process in the thickness of the heart muscle, and even minor scar changes are the basis for the pathological circulation of the impulse along the myocardial fibers,
- Post-infarction cardiosclerosis (PICS) is cicatricial changes in the normal structure of the myocardium.
If the patient, after a complete examination, does not find organic damage to the myocardium, it is most likely that the cause of bigeminy and trigeminy is a violation of the autonomic influences on the heart due to vegetative-vascular dystonia. This pathology requires consultation with a neurologist.
Symptoms of bigeminy and trigeminy
Symptoms of extrasystole of the bi- or trigeminy type consist of cardiac and neurological symptoms.
Cardiological manifestations consist in the patient feeling rhythmic shocks in the heart area, alternating with a feeling of stopping, freezing of the heart. This period corresponds to a compensatory pause on the ECG. There is also internal trembling, a feeling of lack of air and discomfort behind the sternum or in the left half of the chest of a pressing or burning nature.
Neurological symptoms arise due to disruption of the full cycle of heartbeat, resulting in insufficient blood flowing to the brain. The patient may experience lethargy, drowsiness, spots flashing before the eyes, and a faint state. In rare cases, short-term fainting may develop, especially if allorhythmia is combined with other heart rhythm disorders.
If such symptoms occur, especially when combined with high or low blood pressure, the patient should immediately consult a doctor (at a clinic or emergency room).
What is trigemy?
Trigeminy is a heart rhythm disorder characterized by extraordinary contraction of muscles or their individual parts. The pathology is benign and therefore does not threaten the patient’s life. But if there is no treatment or the wrong treatment tactics are prescribed, adverse complications may occur.
Doctors distinguish several types of trigemynia depending on its location:
- Ventricular. On the ECG, this type is manifested by the presence of premature QRS complexes without preceding P waves. They are wider and deformed. There is also a complete compensatory pause. Ventricular extrasystole of the heart of the trigeminy type appears every 2 full contractions.
- Supraventricular. The cardiogram reveals the presence of premature QRS complexes, and there are P waves preceding them. With this type of trigeminy, an incomplete compensatory pause is observed on the ECG. Extrasystole occurs in the same way as in the first case - after 2 contractions.
- Mixed, affecting several areas of the heart at once.
There are also types of the disease depending on the frequency of occurrence:
- Frequent: appears more than 30 times per hour.
- Average: no more than 15 times per hour.
- Rare: less than 5 times per hour.
Trigemy is divided into varieties and according to the number of pathological foci. If there is one, then there is a monotopic form, and if there are two or more, it means a polytopic form.
Diagnostics
The diagnosis of bigeminy and trigeminy becomes obvious after an ECG.
extrasystoles according to the type of bigeminy, trigeminy and quadrigeminy on the ECG
In the case where the patient notes periodic similar complaints, but only single extrasystoles are recorded on the ECG, the patient requires 24-hour blood pressure and ECG monitoring (Holter). This is necessary in order to “catch” the extrasystoles, evaluate the gradation of extrasystoles according to Rayn or Low and obtain a prognostic classification of extrasystoles (see below).
Further, in the case when the patient actually has bigeminy or trigeminy, it is necessary to conduct a full examination to determine the cause of the arrhythmia. Additional examination methods are prescribed:
- General and biochemical blood tests to exclude an inflammatory process, as well as to assess the lipid spectrum of the blood (for atherosclerosis and coronary disease),
- Ultrasound of the heart, or Echo-x (echocardioscopy), which allows you to detect structural or morphological changes in the heart,
- Tests with physical activity (treadmill test, 6-minute walking test, bicycle ergometry) to assess the significance of physical activity in the occurrence of bigeminy and trigeminy, as well as to assess exercise tolerance in ischemia or chronic heart failure.
Video: bigeminy on ECG
Heart rhythm disturbances - we answer your questions
Heart rhythm disturbances – we answer your questions.
What does arrhythmia, heart rhythm disturbances mean?
Heart rhythm disturbances, arrhythmia, is a disturbance in the frequency, rhythm and sequence of contractions of the heart muscle.
The human heart works throughout life. It contracts and relaxes 50 to 150 times per minute. During the systole phase, the heart contracts, ensuring blood flow and delivery of oxygen and nutrients throughout the body. During the diastole phase it rests. Therefore, it is very important that the heart contracts at regular intervals. If the systole period is shortened, the heart does not have time to fully provide the body with blood movement and oxygen. If the diastole period is shortened, the heart does not have time to rest.
What causes arrhythmia and what types of it occur?
The causes of heart rhythm disturbances are not fully understood. It is believed that the main two reasons are changes in nervous and endocrine regulation or functional disorders, and abnormalities in the development of the heart and its anatomical structure - organic disorders. Often there are combinations of these underlying causes.
The reasons may be:
inflammation and dystrophy of the heart muscle, hypertension, coronary disease, heart defects, etc.;
diseases of the endocrine system, most often the thyroid gland;
neuroses, emotional experiences, stress;
unhealthy lifestyle: unbalanced diet, absence or systematic violation of the daily routine, lack of physical activity, smoking and excessive alcohol consumption, etc.
Risk factors for developing cardiac arrhythmias include:
Age. With age, the heart muscle becomes depleted, weakens and loses some of its nutrition. This can affect the formation and conduction of electrical impulses.
Genetics. In people with congenital abnormalities of the heart, arrhythmias occur more often. Moreover, a number of arrhythmias (eg, Wolff-Parkinson-White syndrome, some supraventricular tachycardias, some forms of long QT syndrome) are congenital.
Coronary heart disease, other heart diseases, open heart surgery. Narrowing and occlusion (complete closure) of the lumen of the coronary arteries (arteries that supply the heart muscle), pathology of the heart valves, previous open-heart surgery, cardiomyopathies and other factors damaging the heart are a serious risk factor for the development of almost all types of arrhythmias.
Thyroid diseases. With increased thyroid function, increased production of hormones occurs, overall metabolism increases, and heart contractions become more frequent and irregular. Atrial fibrillation most often develops. With insufficient thyroid function, metabolism decreases, which causes bradycardia, and in some cases, extrasystole.
Medications. Most often, arrhythmia is caused by uncontrolled and excessive use of cold medications containing ephedrine and pseudoepinephrine, as well as a number of other drugs, for example, diuretics, laxatives or anti-asthmatics.
High blood pressure. This increases the risk of developing coronary heart disease. High blood pressure also causes the wall of the left ventricle to thicken, which can change the way impulses are conducted through it.
Obesity. Being a risk factor for the development of coronary heart disease, obesity also increases the risk of developing arrhythmias.
Diabetes. Diabetes mellitus in the stage of decompensation (uncontrolled blood sugar levels) greatly increases the risk of developing coronary heart disease and arterial hypertension. In addition, episodes of hypoglycemia (low blood sugar) can be a trigger for the development of cardiac arrhythmias.
Pathological sleep apnea syndrome. This pathology may be accompanied by bradycardia and atrial fibrillation.
Electrolyte disturbances. Electrolytes such as potassium, magnesium, sodium and calcium form the basis for the formation, maintenance and conduction of electrical impulses in the heart. Too high or too low concentrations of electrolytes in the blood and in heart cells affect the electrical activity of the heart and can cause the development of arrhythmias.
Alcohol consumption. Drinking large doses of alcohol increases the risk of developing atrial fibrillation. Sometimes, the development of atrial fibrillation after excessive alcohol consumption is called “holiday heart syndrome”. Chronic alcohol abuse has a detrimental effect on heart cells and can lead to cardiomyopathy, which is also the basis for the development of cardiac arrhythmias.
Use of stimulants. Psychostimulants such as caffeine, nicotine, etc. cause the development of extrasystole and can also lead to the development of more severe heart rhythm disturbances over time. The use of amphetamines and cocaine can damage the heart muscle with the development of any of the existing arrhythmias and even lead to sudden cardiac death due to the development of ventricular fibrillation.
The most common heart rhythm disturbances are:
•extrasystole (extraordinary contraction),
•atrial fibrillation (atrial fibrillation),
•paroxysmal tachycardia (sharp increase in heart rate from 150 to 200 beats per minute).
An increase in heart rate of more than 100 per minute is called sinus tachycardia. In this case, the full contractions of the heart muscle and the cardiac complexes on the electrocardiogram do not change, an increased rhythm is simply recorded. This can be a healthy person’s reaction to stress or physical activity, but it can also be a symptom of heart failure, various poisonings, and thyroid diseases.
A decrease in heart rate below 60 beats per minute is called sinus bradycardia. Cardiac complexes on the ECG also do not change. This condition can occur in well-trained physically people (athletes). Bradycardia is also accompanied by diseases of the thyroid gland, brain tumors, mushroom poisoning, hypothermia, etc.
Disturbances in cardiac conduction and rhythm are very common complications of cardiovascular diseases.
What symptoms can be used to identify rhythm disturbances?
The classification of rhythm disturbances is very complex. Arrhythmias and blockades can occur anywhere in the conduction system of the heart. Their type depends on the place of occurrence of arrhythmias or blockades.
Extrasystoles or atrial fibrillation are felt by the patient as palpitations, the heart beats faster than usual or there are interruptions in the heart.
If the patient feels fading, cardiac arrest, and at the same time he experiences dizziness and loss of consciousness, most likely the patient has a heart rhythm block or bradycardia (decreased heart rate).
If any heart rhythm disturbance is detected in a patient, it is necessary to conduct a full examination to determine the cause of the arrhythmia.
The main method for diagnosing heart rhythm disorders is an electrocardiogram. An ECG helps determine the type of arrhythmia.
But some arrhythmias occur sporadically. Therefore, Holter monitoring is used to diagnose them. This study provides an electrocardiogram recording over several hours or days. At the same time, the patient leads a normal lifestyle and keeps a diary, where he notes the actions he performs hourly (sleep, rest, physical activity). When interpreting the ECG, the electrocardiogram data is compared with the diary data. The frequency, duration, time of occurrence of arrhythmias and their connection with physical activity are determined, while signs of insufficiency of the blood supply to the heart are analyzed.
Echocardiography allows you to identify diseases that contribute to the development of arrhythmias - valve prolapse, congenital and acquired heart defects, cardiomyopathies, etc.
More modern research methods are also used:
•endocardial (from the internal cavity of the heart),
•transesophageal electrophysiological research methods.
Transesophageal ECG is a study that allows you to cause a patient’s heart rhythm disturbance. It is carried out using a thin electrode, which is inserted through the esophagus to the level of the patient’s right atrium and is activated to provoke an arrhythmic attack. At this time, the doctor takes data on the patient’s heart using standard sensors attached to the patient’s arms, legs and chest. A transesophageal ECG allows you to obtain more accurate data about the disease that caused rhythm disturbances and build a competent treatment plan for it;
ultrasound examination (echocardiography). Allows you to obtain and analyze an image of the heart, which in turn helps to identify the cause of problems in the functioning of the heart;
Endocardial catheterization - the procedure involves inserting a thin radiopaque tube - a catheter - into the heart through large blood vessels. This method allows you to measure pressure in different parts of the heart muscle, as well as obtain samples of heart tissue for analysis, etc. Catheterization is used to confirm and clarify the diagnosis of a systemic disease that has caused a disturbance in the rhythm of contractions of the heart muscle: ischemic heart disease, pulmonary hypertension, etc.
In order to identify the reasons that caused the patient’s arrhythmia, the doctor may prescribe additional laboratory tests of blood, urine and other examination methods.
How should arrhythmia be treated?
When the first signs of cardiac dysfunction appear, you should consult a doctor to make a diagnosis and receive recommendations for treatment.
Treatment of patients with obvious heart rhythm disturbances directly depends on the type of arrhythmia, as well as its degree. As a rule, doctors begin by treating the underlying disease that caused the development of this disease. Most types of heart rhythm disturbances do not require drug treatment and can be eliminated by simple changes in a person’s lifestyle: giving up caffeine in all its forms, quitting smoking, judicious consumption of alcoholic beverages, avoiding stressful situations.
For some heart rhythm disorders, the only treatment method is surgery. This type of treatment is used for arrhythmias such as severe bradycardia, severe AV block, sick sinus syndrome. People suffering from ventricular tachycardia or episodes of ventricular fibrillation are implanted with a defibrillator, which only begins to function when there is an abnormal heart rhythm. When, as a result of research, a pathological focus with increased activity is revealed, which is the source of heart rhythm disturbances, it is destroyed surgically through cardiac catheterization.
What is the prevention of heart rhythm disturbances?
To reduce the risk of arrhythmic disorders it is necessary:
•avoid stress, physical and emotional overload;
•build a daily routine and stick to it: sleep at least 8 hours a day, regularly take walks in the fresh air, conduct moderate physical activity;
•normalize nutrition: eliminate undereating and overeating, give up foods that are too fatty, high in calories and contain a large amount of artificial additives. Patients with heart rhythm disturbances should include in their diet fruits and vegetables containing vitamins C, group B, biotin, carnitine, calcium and magnesium. Their use helps improve the conductivity of cardiac impulses and muscle nutrition; regularly (at least once a year) undergo a full medical examination by qualified specialists;
• give up “bad habits” (smoking, alcohol).
Heart rhythm disturbances are a common manifestation of many diseases of the cardiovascular, endocrine and nervous systems. Therefore, you should remember about prevention and, if necessary, treatment of underlying diseases that lead to rhythm disturbances.
Prevention, timely diagnosis and treatment help prevent the occurrence of pathological consequences dangerous to human health and life.
When the first signs of heart rhythm disturbances appear, you should consult a doctor for a diagnosis and treatment recommendations.
Clinical manifestations of irregular heartbeat can be very varied. At the same time, the patient himself is most often not able to determine what may threaten him with certain interruptions in the work of the heart. For example, such a harmless rhythm disturbance as a single extrasystole (premature contraction of the heart) is quite difficult for many to tolerate and forces them to immediately consult a cardiologist. At the same time, a more serious disorder - a series of extrasystoles - can be perceived as palpitations or “fluttering” in the chest or neck, which the patient gradually ceases to notice.
In the case when the arrhythmia occurs with periodic attacks, the patient feels periods of acceleration of the heart rate or, conversely, a slowdown. If the arrhythmia is permanent, the patient may eventually get used to it and will not seek help from a doctor. This is quite dangerous, because if the arrhythmia becomes protracted, its effect on the functioning of the heart becomes quite significant and the consequences can be serious.
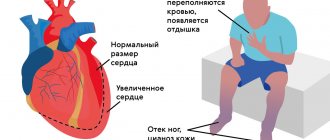
More serious systemic symptoms occur when an arrhythmia causes the heart to stop pumping enough blood. If the arrhythmia is based on weakness of the heart muscle or atherosclerosis (deposition of fats, cholesterol and other substances) in the coronary arteries, then the pumping function of the heart may decrease even more. The patient begins to feel tired, dizzy, and short of breath. Some people begin to experience fainting. In patients with coronary heart disease, angina begins to progress. With chronic heart failure, swelling in the legs increases, heaviness appears in the right hypochondrium and attacks of cardiac asthma occur. If you are concerned about any interruptions in the functioning of your heart, it is better to consult a doctor in a timely manner, who will be able to determine their cause and, if necessary, give valuable recommendations, prescribe treatment, and begin to monitor the condition of your heart.
Prevention measures are best focused on the following:
1.Control cholesterol and blood pressure.
2.Diet low in fat and salt. Regular exercise. Your doctor can tell you what level of activity is appropriate and safe for you.
3. Quit smoking.
4.Limit your alcohol consumption.
5.Take your medications as prescribed.
6. Visit your doctor regularly for periodic examinations, examinations and ongoing monitoring.
Print Email
- Back
- Forward
Treatment
If the patient has excluded organic heart disease as the cause of bigeminy and trigeminy, then he requires examination by a neurologist with treatment of vegetative-vascular dystonia.
First of all, it is necessary to correct the lifestyle with adequate nutrition and a regime of work and rest. It is also necessary to normalize the patient’s psychological state and provide psycho-emotional comfort. Contrast showers, dousing and rubbing with a damp cloth are very good for training the cardiovascular system.
In the case when a patient is diagnosed with one or another heart disease as the cause, it requires mandatory treatment. In some cases, surgical correction of heart disease may even be indicated.
In addition to the main treatment, the patient is prescribed beta-blockers for constant use, for example, sotalol, nebilet, coronal, concor, etc., as well as calcium channel blockers - diltiazem, verapamil, etc. These drugs can reduce the heart rate and reduce the conduction of pathological impulses along the ventricular myocardium.
Cordarone, lidocaine and intravenous quinidine are used as emergency treatments for sudden frequent bigeminy or trigeminy.
In cases where antiarrhythmic therapy is contraindicated for a patient, or its poor tolerability and/or ineffectiveness is noted, the issue of the need for RFA (radiofrequency ablation) must be resolved - that is, cauterization of the tissue of the atrium or ventricle through which pathological impulses pass.
Are there possible complications of bigeminy and trigeminy?
Complications can develop in patients with any extrasystole - ventricular and atrial.
Thus, atrial extrasystole can turn into atrial fibrillation and flutter, and ventricular bigeminy or trigeminy can turn into ventricular tachycardia, ventricular fibrillation and lead to asystole (cardiac arrest). Prevention of complications is the timely initiation of treatment for diseases that led to bigeminy and trigeminy.
Forecast
The prognosis is favorable in most cases. The disease can be easily eliminated if it develops independently. In the presence of concomitant diseases or complications, the outcome for the patient is not so positive.
Having considered what cardiac trigeminy is, we can conclude that in itself it does not pose a danger to human life, but its untimely treatment can lead to negative consequences. To prevent heart problems, you should undergo a preventive examination every year.
It is also important to be more attentive to your health, lead an active lifestyle, eat right, stop smoking and drinking alcohol, do not subject your body to excessive physical activity, monitor your blood pressure and promptly treat any heart disease.