Introduction
Definition
Resistant hypertension
Resistant hypertension is an increase in blood pressure (BP) that requires treatment with more than 3 drugs (one of them is a diuretic).
- An official report from the American Heart Association, published in 1988, expanded the definition to include patients whose blood pressure was eventually controlled but required 4 or more medications to do so, so-called. "controlled resistant hypertension."
Refractory hypertension
- The term “refractory hypertension” was used to refer to a subgroup of patients with ineffective antihypertensive treatment in four separate scientific publications.
- In the short period of time between these publications, the definition of refractory hypertension became increasingly clear.
- The term has been used to define arterial hypertension (HTN) in patients who have failed maximal antihypertensive therapy. When the term was first used, refractory hypertension was defined as uncontrolled hypertension using 5 or more antihypertensive drugs from different classes.
- Most recent uses in the literature of the term “refractory hypertension” have emphasized the failure of optimal blood pressure control with 5 or more antihypertensive agents, including long-acting thiazide diuretics and mineralcorticoid receptor antagonists (MRAs).
Epidemiology
Resistant hypertension
- Evidence from cross-sectional studies agrees that resistant hypertension is defined solely by the number of medications needed to control it in 10–20% of hypertensive patients.
- For example, in an analysis of studies of a large ethnically diverse cohort in the United States, Sim et al. assessed individuals enrolled in a Southern California health care system. More than 470 thousand people were studied, of which, according to the American Heart Association, 15.3% had resistant hypertension.
- Of the 68,045 patients included in the analysis, approximately 15% had resistant hypertension (as defined by the American Heart Association), i.e. Blood pressure > 140/90 mm Hg. Art. when using 3 or more antihypertensive drugs, including diuretics,
Long-term studies show that the prevalence of resistant hypertension has increased dramatically over the past few decades.
- Using data from the Continuing National Health and Nutrition Examination Survey, Roberie and Elliot suggested that the prevalence of overt resistant hypertension in the United States has increased from 8.8% in 1988–1994. up to 14.5% in 1999-2004, and up to 20.7% in 2005-2008.
- The rapid increase in estimated prevalence raises concern that resistant hypertension may represent one of the rapidly growing types of hypertension.
- The reason for the increase in resistant hypertension is not entirely clear, but there is no doubt that common risk factors for developing hypertension, such as older age,
- obesity,
- chronic kidney disease (CKD).
Refractory hypertension
- Among the four currently published studies on refractory hypertension, the estimated prevalence of this condition ranged from approximately 5% to 30%.
- In the initial study of refractory hypertension, a retrospective analysis of more than 300 patients conducted by the University of Alabama at Birmingham Resistant Hypertension Clinic found that approximately 10% of adequately treated patients were never able to achieve blood pressure control despite the use of 5 or more antihypertensive medications. .
- More recently, the same group of researchers published a prospective analysis of more than 700 patients with resistant hypertension, which found that only 29, or approximately 4%, had refractory hypertension.
- There are important differences between different studies' definitions of refractory hypertension. Previously, in a retrospective analysis, the definition of refractory hypertension was based only on the need for 5 or more antihypertensive drugs, without dividing the drugs used into classes. Later, in a prospective analysis, the definition of refractory hypertension became more stringent and consisted of irregular medication use, combining 5 or more drugs, including chlorthalidone and spironolactone.
- In a study by Modolo et al. refractory hypertension was determined only by the number of drugs, i.e. 5 or more. In a cross-sectional analysis of 116 people with resistant hypertension, 31% had hypertension that was not controlled by 5 or more medications. All refractory patients received diuretics and the majority received spironolactone (76%).
- Another study of refractory hypertension was a cross-sectional assessment of participants in the Reasons for Geographic and Ethnic Differences in the Course of Stroke (REGARDS) study, a large (n=30,239) cohort study. In this analysis, refractory hypertension was defined as uncontrolled hypertension despite taking 5 or more different classes of medications. The use of diuretics, including specifically chlorthalidone and spironolactone, was not a required part of the definition. The incidence of refractory hypertension was 3.6% of patients with resistant hypertension (not controlled by 3 or more drugs or controlled by 4 or more drugs) and 0.5% of all patients with hypertension. All REGARDS participants assigned to the refractory hypertension group received diuretics (either hydrochlorothiazide (HCTZ) or furosemide); none received chlorthalidone or spironolactone.
Studies on refractory hypertension have now been published, identifying its varying prevalence from a low of 5% to a high of 30% among patients with true resistant hypertension.
The wide discrepancy is undoubtedly due to significant differences in the cohorts analyzed and the definition of refractory hypertension. By definition, chlorthalidone and spironolactone must be used before diagnosing refractory hypertension.
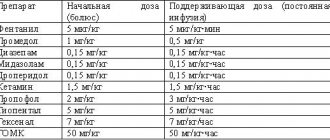
Treatment of resistant arterial hypertension: new perspectives
The focus is on resistant or refractory arterial hypertension (AH) as one of the causes of poor blood pressure control. Under resistant hypertension, in accordance with the recommendations of the RMOAH/VNOK [5], the European Society of Hypertension/European Society of Cardiology (ESH/ESC), as well as the American College of Cardiology (ACC) and the American Heart Association (AHA) [6,7], understand that the target blood pressure level is exceeded despite treatment with three antihypertensive drugs, one of which is a diuretic. Resistant hypertension can be controlled if blood pressure control is achieved by prescribing more drugs. Otherwise, hypertension is resistant uncontrolled. Pseudo-resistant hypertension is also identified, which is caused by incorrect blood pressure measurements, low adherence to treatment, and “office” increases in blood pressure. In most cases, unrecognized secondary hypertension is resistant: associated with obstructive sleep apnea syndrome (OSA), primary aldosteronism, pheochromocytoma, hypercorticism, parenchymal kidney diseases, renal artery stenosis, often poorly controlled hypertension occurs in diabetes mellitus. In addition, excessive salt intake, alcohol, and certain medications (nonsteroidal anti-inflammatory drugs (NSAIDs), laxatives, amphetamines, ephedrine derivatives, estrogen-containing oral contraceptives, licorice, glucocorticosteroids, erythropoietins) can lead to resistance. The severity of the hypertensive effect of these drugs varies from person to person, but it has been proven that old age, diabetes mellitus, and decreased renal function contribute to its manifestation. A special form of hypertension is malignant hypertension. Malignant hypertension is characterized by a significant increase in blood pressure (more than 180/120 mmHg) with the development of severe changes in the vascular wall (fibrinoid necrosis), which leads to hemorrhages and/or swelling of the optic nerve nipple, tissue ischemia and dysfunction of various organs. The transition of hypertension to malignancy is possible in all its forms, but more often this occurs in patients with secondary or severe hypertension. Without effective treatment, 50% of patients die within the first year. The presence of malignant hypertension is assessed as a severe emergency condition and requires a reduction in DBP to 100–110 mm Hg. Art. within 24 hours. Patients with malignant hypertension are prescribed three-component antihypertensive therapy. Predictors of insufficient blood pressure control are older age (over 75 years), left ventricular hypertrophy (LVH), obesity (body mass index more than 30 kg/m2), high initial blood pressure (systolic blood pressure more than 160 mmHg), chronic renal failure (CRF) with creatinine more than 1.5 mg/dl, diabetes mellitus, and also, according to the results of the ALLHAT study, belonging to the Negroid race and female gender. Along with this, of undoubted interest are the data found in the ASCOT study on the reduction in the risk of developing resistance in patients receiving treatment with calcium antagonists (CA) (amlodipine) followed by the addition of the angiotensin-converting enzyme inhibitor (ACE inhibitor) perindopril [8] (Table 1). Ways to overcome resistant hypertension, recommended for clinical practice. Prerequisites for successful treatment of hypertension are weight loss, limiting salt intake, alcohol consumption, regular moderate-intensity physical activity, a diet with limited animal fats and consumption of large amounts of polyunsaturated fats, coarse fiber, vegetables, fruits ( DASH–diet: Dietary Approaches to Stop Hypertension), if possible, discontinuation of drugs that increase blood pressure or reduce the effectiveness of antihypertensive therapy, identification and treatment of secondary hypertension, as well as observation by a hypertension specialist. It is very important that the doctor and patient are persistent in reducing high blood pressure and achieving its target level. To achieve effective blood pressure control, the patient is required to adhere to treatment, and it largely depends on how conscientiously the doctor will carry out explanatory work and be able to convince the patient of the need for treatment. Often, hypertension is formally recognized as resistant, although pharmacotherapy has not been selected, drug doses have not been adjusted to maximum therapeutic levels, rational combinations of antihypertensive drugs have not been used, etc. For the most effective treatment of resistant hypertension, it is advisable to target different stages of pathogenesis. Great importance is attached to the prescription of blockers of the renin-angiotensin-aldosterone system (RAAS). The effectiveness of the combination of RAAS blockers with AK has been proven in both hypo- and hyperrenin forms of hypertension due to the direct and renin-mediated mechanism of vasodilation. With the combined use of drugs from these groups, organoprotective effects are potentiated (regression of LVH, proteinuria, anti-ischemic, anti-atherosclerotic, natriuretic effects). In addition, when jointly prescribing an ACE inhibitor or an angiotensin receptor blocker (ARB) with ACB, counter-regulatory mechanisms that reduce the effectiveness of each drug in monotherapy are neutralized: in contrast to ACB, ACE inhibitors and ARBs suppress the activity of the RAAS and the sympathetic nervous system (SNS); in turn, AA increase sodium excretion, which increases the effectiveness of ACEIs/ARBs. Thanks to this, the frequency of such undesirable effects as tachycardia and swelling of the legs is significantly reduced. The greater effectiveness of the combination of AKs with RAAS blockers in lowering blood pressure and preventing complications of hypertension is confirmed by the results of both Russian and foreign studies: ASCOT-BPLA (the combination of AKs + ACE inhibitors was compared with the combination of a β-blocker + diuretic), ACCOMPLISH (the combination of AKIs + AKIs was compared with combinations of ACEI + diuretic), HAMLET (a combination of amlodipine and lisinopril was compared with monotherapy), EMEA (combinations of amlodipine with valsartan 5/160 mg and 10/160 mg were compared with valsartan 160 mg monotherapy). The Russian PRORYV study [9] showed the high effectiveness of a fixed combination of perindopril with amlodipine in 4115 patients with uncontrolled hypertension in achieving the target blood pressure level (Fig. 1). For resistant and severe hypertension, in order to increase adherence to treatment and cost-effectiveness, their fixed combinations are recommended. At the same time, double blockade of the RAAS (simultaneous administration of ACE inhibitors and ARBs or the addition of the direct renin inhibitor aliskiren to one of them) did not justify itself due to the development of undesirable effects. Most treatment regimens for resistant hypertension include diuretics. Considering the hidden (as a rule, there is no edema) volume overload in patients with resistant hypertension, even when treated with diuretics in standard doses, the latter should be prescribed at the maximum tolerated/effective dose. The dose of the diuretic is gradually increased to the maximum allowable. In this situation, it is necessary to remember the possibility of clinical signs of excessive dehydration, such as weakness, orthostatic hypotension, decreased tissue perfusion (increased creatine not explained by other reasons). Excessive therapy with diuretics can lead to excessive excretion of sodium with subsequent activation of the RAAS and an increase in blood pressure. It is recommended to start treatment with diuretics with thiazide diuretics (hydrochlorothiazide, in some cases - the sulfonamide derivative of thiazides indapamide, as well as drugs not available in the Russian Federation: bendrofluazide, chlorthalidone, metolazone). The most effective blood pressure reducer in this group is chlorthalidone (available in the Russian Federation only in the form of fixed combinations with atenolol). Chlorthalidone has a longer duration of action and a more pronounced hypotensive effect than hydrochlorothiazide; its administration in lower dosages led to a comparable decrease in blood pressure. The ALLHAT study demonstrated the ability of chlorthalidone to reduce the risk of vascular events. For chronic renal failure, loop diuretics (furosemide, torsemide, bumetanide, ethacrynic acid) can be used. Abroad, for hypertension in combination with chronic renal failure, the thiazide derivative metolazone and its improved formula microx at a dose of 0.5–1.0 mg/day have an advantage. (currently not sold in the Russian Federation), however, its disadvantage is variable absorption. The main side effect of diuretics is hypokalemia, so monitoring plasma potassium levels is necessary for the first 10–14 days until a new potassium balance is established. Potassium-sparing agents and their combinations with thiazides may be useful. The RMOAG/VNOK recommendations for the diagnosis and treatment of hypertension [4] speak of the advisability of prescribing triple full-dose antihypertensive therapy for resistant hypertension; The following three-component combinations are considered rational: ACEI + dihydropyridine AC + β-adrenergic blockers (β-AB); ARB + dihydropyridine AA + β–AB; ACE inhibitor + AA + diuretic; ARB + AA + diuretic; ACE inhibitor + diuretic + β-blocker; ARB + diuretic + β-blocker; dihydropyridine AK + diuretic + β-AB. Of those presented, the combination of a RAAS blocker with an AK and a diuretic seems to be the most effective, and this is what American experts recommend (resistant hypertension). If there are special indications (coronary artery disease, heart failure), adding a β-blocker to this regimen, preferably with vasodilating properties, is justified. In recent years, there has been renewed interest in aldosterone antagonists, the long-known spironolactone, and the selective mineralocorticoid receptor antagonist eplerenone, which has recently entered clinical practice. In resistant hypertension, the effectiveness of aldosterone antagonists has been proven regardless of the presence or absence of hyperaldosteronism. One of the largest studies, ASCOT, analyzed 1411 people who met resistance criteria [10]. Spironolactone was added to the therapy in patients who did not reach the target blood pressure level at an average dose of 25 mg/day, which contributed to an additional reduction in systolic/diastolic blood pressure by 22/10 mm Hg. after a year of treatment (Fig. 2). This and a number of other studies have shown an increased risk of hyperkalemia in patients with chronic renal failure, as well as with the simultaneous administration of other drugs that increase the concentration of potassium in plasma: ACE inhibitors or ARBs, NSAIDs. In the recently completed randomized ASPIRANT trial (117 patients included), spironolactone or placebo was added to an average of four antihypertensive drugs, and spironolactone was effective in lowering systolic blood pressure in resistant hypertension. In another randomized trial, 42 overweight or obese patients received an ACEI or ARB or spironolactone (25–50 mg/day) in addition to initial therapy of an ARB or ACEI and 3 other drugs; It has been shown that in resistant hypertension the effect of spironolactone is higher than with double blockade of the RAAS. Eplerenone has a significantly lower incidence of such undesirable effects of spironolactone as hyperkalemia and gynecomastia. The effectiveness of eplerenone in resistant hypertension was studied in one study that included 52 patients with resistant hypertension, overweight/obesity and varying levels of renal function. When adding eplerenone at a dose of 50–100 mg/day. to therapy with 3 to 7 antihypertensive drugs (including ACE inhibitors or ARBs), there was a significant decrease in blood pressure, regardless of the initial level of aldosterone and plasma renin activity, and the need for prescribing other drugs that lower blood pressure decreased. Only 2 patients had a total of 3 cases of moderate hyperkalemia (plasma potassium less than 6 but more than 5.5 mmol/L). These studies, despite the relatively small sample of participants, indicate the advisability of including spironolactone or eplerenone in the treatment regimen of patients with resistant hypertension. There is evidence of the effectiveness of the combination of amiloride with hydrochlorothiazide in resistant hypertension, especially when it is impossible to use mineralocorticoid receptor antagonists. In the reserve of pharmacotherapy are drugs whose prescription is limited by side effects and requires medical supervision: centrally acting antihypertensives (clonidine, guanfacine), myotropic peripheral vasodilators (hydralazine, minoxidil, not currently available in the Russian Federation), sympatholytics (reserpine, guanethidine), α1 – blockers (doxazosin, terazosin). New antihypertensive drugs under development Over the last decade, attempts have been made to search for new pharmacological targets and influence them in order to more effectively lower blood pressure and reduce the incidence of side effects. From this point of view, blockade of the RAAS at the level of renin seemed attractive, but the advantage of its direct inhibitor aliskiren in resistant arterial hypertension has not been proven. In addition, there is evidence of negative effects of aliskiren in certain groups of patients. Thus, according to the results of the ALTITUDE study, simultaneous administration of the direct renin inhibitor aliskiren with an ACE inhibitor or ARB in patients with type 2 diabetes mellitus leads to impaired renal function, hypotension and hyperkalemia. Also, during treatment with this combination, an increase in mortality and stroke rates was noted, and therefore the study was stopped early. The simultaneous administration of aliskiren with an ACE inhibitor or ARB for diabetes mellitus and renal failure (glomerular filtration rate (GFR) less than 60 ml/min.) is not recommended. Currently, the following classes of new pharmacological agents can be distinguished at different stages of development: drugs acting on the RAAS (prorenin receptor blockers, double and triple inhibitors of vasopeptidases - ACE, neprilysin, endothelin-converting factor; aldosterone synthase antagonists; polymers - potassium ion exchangers created to prevent hyperkalemia 39; aldosterone receptor antagonists other than spironolactone and eplerenone, for example non-steroidal hybrids with calcium antagonist properties; drugs affecting the renalase system); selective endothelin-A receptor antagonists; nitric oxide donors (drugs that release nitric oxide: nitrosyl-cobalamide, NO-releasing hybrids of losartan and telmisartan, non-peptide nitro derivatives of renin inhibitors, naproxinod - an NO donor with NSAID properties (for the treatment of hypertension with arthritis); natriuretic peptide agonists, AT receptor agonists -2 type 2. Laboratory experiments on rats have shown the effectiveness of genetic therapy methods using viral and other vectors of genes responsible for the expression of substances that help lower blood pressure. Work is also underway to create a vaccine against AT-2. Of interest are molecules aimed at fight against cellular aging, i.e. inhibitors (aminoguanidine, pyridoxamine) and lidases (alagebrium and structural analogues of pyridine) of advanced glycation end products, which contribute to increased arterial stiffness and the formation of isolated systolic hypertension.Endovascular treatment of resistant hypertension The presence of resistant hypertension stimulates the development of non-drug methods influence on the pathogenetic mechanisms of the disease. Catheter ablation of the sympathetic plexus of the renal artery, or renal denervation, is currently considered a promising method in the treatment of resistant arterial hypertension [11,12]. At the beginning of the 20th century, R. Smithwick, head of the department of surgery at Boston University (USA), proposed an operation for the treatment of hypertension, during which bilateral lumbodorsal sympathectomy and splanchnicectomy with resection of the sympathetic ganglia in the lower thoracic region were performed. Symptomatic orthostatic hypotension was a common complication, but despite this, many patients with severe hypertension felt better after the intervention. Subsequently, this surgical method was not developed due to the advent of antihypertensive drugs. Today the Smithwick method is experiencing a rebirth. Pathophysiology. With hypertension of almost any origin, there is an increase in the tone of the sympathetic nervous system (SNS). Hyperactivation of the SNS and a progressive increase in blood pressure mutually reinforce each other and participate in the formation of a vicious circle. Increased activity of the SNS most affects the kidneys. When the SNS is hyperactivated, vasoconstriction occurs in the kidney, blood flow and filtration decrease, renin secretion increases, and sodium and water reabsorption increases. Afferent impulses from the kidneys along afferent nerve fibers enter first the lateral horns of the spinal cord, and then to the vascular center in the central nervous system, contributing to an increase in blood pressure. It increases with stretching of mechanoreceptors, renal ischemia, and under the influence of hypoxia. The experiment showed that electrical stimulation of the afferent nerve fibers of the kidneys increases blood pressure and causes vasospasm. Denervation of these fibers, on the contrary, helps reduce blood pressure. Procedure. The Medtronic Ardian Sympicity Catheter System consists of a radiofrequency wave generator and a disposable catheter with a tip control mechanism. The generator produces radio frequency waves with a capacity of 5–8 watts and constantly controls the temperature and impedance at the tip of the catheter. If the necessary parameters are exceeded or not distant or after 2 minutes. The system is automatically disconnected of effective exposure. The tip of the catheter is a platinum -iridium electrode, it is radiocontranstens and, thanks to this, also performs the function of the label during catheterization. In case of endovascular renal denervation after angiography of the renal artery at its mouth, the controller 6f is installed, then under angiographic control the catheter for radio frequency ablation (RCH) is summed up to the level of bifurcation and connected to the generator (Fig. 3). After that, with the help of a special mechanism that allows to orient the catheter for the RCC in the right direction, it moves proximally (from the kidney to the aorta). At the same time, 4-6 radio frequency influences of 2 minutes are performed. With a step of at least 5 mm and a rotation angle of 45 ° around the circle of the vessel. The catheter affects sympathetic fibers through the entire thickness of the renal artery. Ablation leads to a certain damage to the endothelium, but so far, according to the results of control angiograms, the clinically significant consequences of this damage have not been revealed. In the literature there are attempts to explain the absence of significant damage to the endothelium by its lower sensitivity to the chosen effects, as well as the cooling effect of blood washing the internal wall of the artery. The evidence base is currently the effectiveness and safety of endovascular denervation of the kidneys is actively studied around the world. At this point, the Symplicity HTN --1,2 studies have been completed; Studies of HTN -3 and Duration of Renal Sympathetic Activation and Hypertension are conducted [12–14]. The research shows the effectiveness of the method in reducing blood pressure with resistant hypertension, as well as its safety. The maximum duration of the observation was 2 years, by the end of this period the decrease in blood pressure was about 30/10 mm Hg. According to Symplicity HTN -1, after the renal denervation, the level of the garden is below 140 mm Hg. was reached in 39%, below 160 mm Hg. - In 82% operated. With high efficiency, the complications took place in a small number of cases and were successfully cured. Among the complications there were 1 pseudoenerism, 1 dissection, successfully eliminated by stenting, 1 episode of postoperative hypotension, 1 case of urinary tract infection, 1 case of pain in the back, 7 out of 52 operated during the procedure, a transient bradycardia was noted, which in some cases required the introduction of atropine In 2 patients, there was an aggravation of atherosclerosis of the renal artery, endovascular treatment did not require (in particular, in HTN –1 there was a case of progression of the stenosis of the renal arteries in the segment remote from the place of exposure). There were no cases of violation of the nitrogen function of the kidneys (estimated after 6 months according to creatinine, SKF, cystatin C). For the first time in Russia, this procedure was carried out in 2011 in the RKNPK. Data on 5 successfully conducted operations were published [15]. With control after 1 month. The persistent effect of the procedure was preserved, blood pressure continued to decline, side effects, as well as early and late complications, was not noted. The sympathetic denervation of the renal arteries is still not a well -studied method, so ESH/ESC experts recommend resorting to it only if there are strict indications. The indication for the procedure is a resistant uncontrolled essential hypertension (systolic blood pressure when measured by a doctor and self -control - more than 160 mm Hg or 150 mm Hg - in patients with diabetes mellitus), despite the three -component treatment and a satisfactory commitment conducted by an AH specialist and a satisfactory commitment the patient for treatment. Contraindications to the procedure are: renal arteries less than 4 mm in diameter and less than 20 mm in length, manipulation on the renal arteries (angioplasty, stenting) in a history, stenosis of the renal arteries of more than 50%, renal failure (SKF less than 45 ml/min./1 , 75 m2), vascular events (them, episode of unstable angina, transient ischemic attack, stroke) less than 6 months. Before the procedure, any secondary form of hypertension. The method of electrical stimulation of carotide baro -receptors of the carotide sinus, another method of impact on the activity of the SNA at the stage of clinical tests is the electrical stimulation of carotide sinus barooreceptors (BCS) with the aim of reflex reduction in blood pressure. BCS, located in the area of bifurcation of carotid arteries, take part in the regulation of blood pressure. When it increases, the receptors are stretched, then the impulse from them enters the vascular center of the brain, which leads to a decrease in blood pressure. With hypertension, the sensitivity of baroreceptors decreases. The BCS circuit is shown in Figure 4. With electrical stimulation of the electrodes of the rhythm -sinus stimulant RHEOS (CVRX, Minneapolis, MN, USA) are brought to the sleepy arteries and are connected to the generator, which is sewn under the skin of the anterior chest wall. The implantation of the stimulant is carried out by a vascular surgeon, cardio or neurosurgeon. Before introducing the electrode, the most sensitive to stimulation of the carotide sinus zone is made in the thickness of the carbon artery wall: the generator supplies a small discharge to the electrode (for the treatment of watts, current is used under a voltage of 1-6 V); 30 s after exposure to this section of the carotide sinus, blood pressure is measured. The electrode is left in the place where the decrease in blood pressure in response to the category of a given force is as much as possible. The strength of the discharge supplied to the electrodes is regulated by the computer program, by analogy with how this happens when setting a pacemaker; The generator and the computer are in radio frequency conjugation. The data of the first randomized double -blind and controlled study on the assessment of the clinical efficiency of BCS - Rheos Pivotal Trial's stimulation were published in 2011 [16]. During the study, 265 patients with resistant hypertension showed the effectiveness of the BCS stimulation method. During control after a year, the decrease in systolic blood pressure was an average of 35 mm Hg; In half of the subjects, blood pressure values of less than 140 mm Hg were achieved. The maximum duration of the observation was 53 months, during all this period, the hypotensive effect remained. The main complications were associated with the infection of the operating wound and nerve damage, however, their frequency was significantly less than with a well -developed endarctomy operation, and in most cases these complications were reversible, and residual effects were insignificant. It is important to note that in order to achieve a complete effect it is necessary for a long time, because The restructuring of vascular tone is in nature a long process. In another recently published study of Barostim Neo (30 patients), a 2nd generation device was studied, much smaller for unilateral stimulation. Barore receptor stimulation showed their effectiveness even in those 6 patients who had previously performed unsuccessful catheternaries of the renal arteries and a higher initial level of blood pressure [17]. The results indicate the prospect of the method. Its improvement is currently ongoing. Perhaps in the near future the introduction of electrical stimulation of BCS in clinical practice will begin. In the Russian Federation, clinical trials of this method were not carried out. Thus, it seems that in the arsenal of AH experts, new methods of non -kettle treatment will soon appear - the denialization of the renal arteries and the electrical stimulation of BCS. In addition to evaluating the effectiveness of these methods, different aspects of treatment remain unclear: predictors of success and criteria for the effectiveness of procedures, the duration of the effect, the possibility of damage to the vascular endothelium, the risk of developing undesirable effects. Nevertheless, the success of their first clinical trials allows us to count on their use in the near future. The procedures and hardware methods for treating hypertension at the stage of scientific development are of interest is the method of neurovascular decompression of the brain stem. There is evidence that increased blood pressure can be associated with its compression of air, mainly the posterior lower cerebellar artery. In small work (randomized studies in this area have not yet been carried out), a persistent decrease in blood pressure was noted as a result of surgical decompression of the brain, however, in accordance with the Norman Kaplan data, not any of the arteries are pathogenetically determined by Agricultural and surgical decompression helps all patients with AH. It is still unknown how to determine whether AH is connected in a particular patient with neurovascular compression, but syndromes are described in which this connection significantly exists (brachidactyli, hypertension, neurovascular compression). It is noted that the deep stimulation of the brain used in chronic pain syndrome, Parkinson's disease, etc., can lead to a decrease in blood pressure in concomitant hypertension, but so far it is not used in clinical practice. The possibility of developing a new treatment method for AH with the help of hardware control of the respiratory function based on the connection of the respiratory and vascular centers is also discussed. Conclusion Effective Treatment of AH refers to priority areas in medicine. “Overcoming resistance” in the treatment of patients with hypertension is largely based on compliance with all the recommended principles for conducting this category of patients, including a rational selection of combined therapy. In cases of true resistance to therapy, there are treatment methods using apparatuses to achieve control of blood pressure with an acceptable degree of safety.
References 1. Kearney PM, Whelton M, Reynolds K et al. Global burden of hypertension: analysis of worldwide data // Lancet. 2005. Vol. 365. P. 217–233. 2. Guidelines for the management of arterial hypertension. The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) // Eur. Heart J. 2007. Vol. 28. P. 1462–1536. 3. Oganov R.G., Timofeeva T.N., Koltunov I.E. and others. Epidemiology of arterial hypertension in Russia. Results of federal monitoring 2003–2010. // Cardiovasc. therapy and prevention. – 2011. – T. 10(1). – P. 8–12. 4. Russian Medical Society for Arterial Hypertension (RMAS)/All-Russian Scientific Society of Cardiologists (VNOK). Diagnosis and treatment of arterial hypertension. Russian recommendations (fourth revision) // Systemic hypertension. – 2010. – No. 3. – P. 5–26. 5. The 7th report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure // JAMA. 2003. Vol. 289. P. 2560–2572. 6. Calhoun DA, Jones D, Textor S et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research // Hypertension. 2008. Vol. 51. P. 1403. 7. Acelajado MC, Pisoni R., Dudenbostel T. et al. Refractory hypertension: definition, prevalence, and patient characteristics // J. Clin. Hypertens. (Greenwich). 2012. Vol. 14(1). P. 7–12. 8. Gupta AK, Nasothimioua EG, Changa CL et al. Baseline predictors of resistant hypertension in the Anglo–Scandinavian Cardiac Outcome Trial (ASCOT): a risk score to identify those at high–risk // J. Hypertens. 2011. Vol. 29. 9. Karpov Yu.A., Deev A.D. on behalf of the doctors participating in the PRORYV program. Uncontrolled hypertension - new opportunities in solving the problem of increasing the effectiveness of treatment // Cardiology. – 2012. – No. 2. – P. 29–35. 10. Chapman N., Dobson J., Wilson S. et al. Anglo-Scandinavian Cardiac Outcomes Trial Investigators. Effect of spironolactone on blood pressure in subjects with resistant hypertension // Нypertens. 2007. Vol. 49. P. 839–845. 11. Schmieder RE, Redon J, Grassi G et al. ESH Position Paper: renal denervation – an interventional therapy of resistant hypertension // J. Hypertens. 2012. Vol. 30(5). 12. Krum H., Schlaich M., Whitbourn R. et al. Catheter–based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof–of–principle cohort study //Lancet. 2009. Vol. 373. P. 1275–1281. 13. Symplicity HTN–1 Investigators. Catheter–based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months // Hypertens. 2011. Vol. 57. P. 911–917. 14. Symplicity HTN–2 Investigators. Renal sympathetic denervation in patients with treatment–resistant hypertension (The Symplicity HTN–2 Trial): a randomized controlled trial // Lancet. 2010. Vol. 376. P. 1903–1909. 15. Danilov N.M., Matchin Yu.G., Chazova I.E. Endovascular radiofrequency denervation of the renal arteries is an innovative method for the treatment of refractory arterial hypertension. First experience in Russia // Angiol. and a vessel. Surgery. – 2012. – No. 18(1). – pp. 51–56. 16. Burke SL, Evans RG et al. Levels of renal and extrarenal sympathetic drive in angiotensin–2–induced hypertension // Hypertens. 2008. Vol. 51. P. 878–883. 17. Bisognano JD, Bakris G, Nadim MK et al. Baroreflex activation therapy lowers blood pressure in patients with resistant hypertension: results from the double–blind, randomized, placebo–controlled rheos pivotal trial // JACC. 2011. Vol. 58. P. 765.
Appearance versus truth
Resistant hypertension
- Estimation of the prevalence of resistant hypertension builds on the above and is based solely on the level of clinical BP measurement and the number of antihypertensive medications prescribed.
- The general causes of the so-called pseudotherapeutic resistance, including the “white coat” effect, are not taken into account.
- low adherence to therapy,
- incomplete compliance with the therapeutic regimen.
- Correction of these factors will result in a reduction in the estimated level of hypertension and a better estimate of the incidence of “true” resistant hypertension.
- For example, in a study by de la Serra et al. It was discussed that the analysis of the Spanish Ambulatory BP Monitoring Registry took into account individual risk factors. Notably, nearly 38% of patients diagnosed with resistant hypertension had “white coat” hypertension (ie, BP was elevated in the clinic but controlled outside the clinic).
- For example, Jung et al. recently reported that of 76 patients referred to a dedicated resistant hypertension clinic, 53% were not regularly taking their antihypertensive medications (data based on urine and blood tests measuring relevant drug metabolites). As it turned out, of these patients with low adherence to treatment, 30% did not take any drug.
- In an evaluation of more than 200 clinical community organizations in the southeastern United States, Egan et al. identified 44,684 patients whose blood pressure remained uncontrolled despite being prescribed 3 or more antihypertensive medications.
- The authors retrospectively assessed patients who were completely randomized in a multidisciplinary study designed to assess clinical failure of therapy or blood pressure control.
- 91% of patients received diuretics (either HCTZ or furosemide), none received chlorthalidone or mineralcorticoid receptor antagonists.
Overall, data from Grigoryan and other recent studies indicate that the incidence of true resistant hypertension is probably less than 50% of the incidence of diagnosed resistant hypertension.
Refractory hypertension
- The definition of diagnosable versus true refractory hypertension has not yet been systematically developed.
- Rigorous definitions of adherence rely on measurement of drug levels in serum and urine.
- It is possible that the prevalence of treatment non-adherence among patients with refractory hypertension will be higher than in patients with resistant hypertension.
- Two published studies on refractory hypertension report a white coat effect with 24-hour ambulatory BP monitoring. Modolo et al. say that patients with refractory hypertension may have had a greater “white effect” (≥20/10 mmHg when comparing ambulatory and office blood pressure levels) than patients with controlled or uncontrolled resistant hypertension, but it is not clear a certain number or percentage of patients with refractory hypertension.
- Dudenbostel et al. their study reported that 24-hour ambulatory monitoring BP levels were significantly higher in patients with refractory versus controlled resistant hypertension, but did not report the extent of the white coat effect or its prevalence.
Thus, while many studies show that the causes of pseudoresistance are common in patients with resistant and refractory hypertension, the extent to which these same factors are found in patients with refractory hypertension is still not determined.
Resistant arterial hypertension - possible ways to overcome the problem
Conradi A.O. made a presentation at the Internet Congress.
00:00
Grigory Pavlovich Arutyunov , Doctor of Medical Sciences, Professor:
— We give the floor to Alexandra Olegovna.
Alexandra Olegovna Conradi , Doctor of Medical Sciences, Professor:
— I am glad to greet you from frosty St. Petersburg.
The topic of my speech today is “Resistant arterial hypertension.” Today we have traditionally begun to deal with this problem. We will try to share with our program listeners modern ideas on resistant hypertension.
Short plan. Today we will discuss the question of what we mean by the concept of resistant hypertension, how often it occurs, what are its causes, how to actually identify it and how to actually treat it.
According to the latest definition (there have been no updates since 2007), we can understand resistant hypertension (or refractory to therapy) as a condition when the patient’s treatment includes lifestyle changes and the prescription of at least three antihypertensive drugs in adequate doses. But at the same time, systolic and/or diastolic blood pressure (BP) does not decrease properly.
There are two quite important points in this definition, namely about three drugs. The European recommendations do not specify which ones. The concept of “adequate dose” is flexible. In this case, apparently, a larger full therapeutic dose of the drug should be implied. If the drug is underdosed, then we cannot consider such a patient resistant.
Americans always go a little further, so there are some notes in their recommendations. Drugs should be used in rational recommendations, but include diuretics. Here it becomes more clear in which case, if there are three drugs, we can consider the patient resistant to therapy.
Reducing blood pressure to the target level is necessary. For all patients it is 140 and 90. For high-risk patients it is 130 and 80. Isolated arterial hypertension (AH) is at least less than 160. The condition of actually taking the drugs must be met, that is, patients must be committed to treatment.
According to modern data, what can we say about the prevalence of hypertension and its control. Despite our large government investments and the implementation of federal programs (to combat hypertension and socially significant diseases), today the proportion of patients who have the proper level of blood pressure during therapy is slightly more than 20%, according to the most optimistic forecasts.
02:47
Uncontrolled hypertension does not mean resistant. Let's think about how many such patients there are in the world today.
If we imagine, according to prevalence data, that 40% of Russian residents (adults) suffer from high blood pressure, then this is approximately 60 million people living in the Russian Federation. Approximately 20 million in Russia do not know that they have high blood pressure. Only 12 million receive treatment. Of these, only 6-7 million people have target blood pressure levels. If we are talking about patients with diabetes, then this is even less.
Thus, according to the most conservative estimates, about 6-7 million patients walking down the street and attending our appointments today have uncontrolled blood pressure levels for various reasons.
Uncontrolled blood pressure levels, even in patients receiving treatment, are always resistant to the therapy. Very often, unfortunately, this is low adherence and our not entirely adequate selection of treatment.
We analyzed a regular average St. Petersburg clinic in a random sample of patients. We noticed that today, in a standard therapeutic area, approximately 63–64% of patients have uncontrolled blood pressure levels, despite the fact that they regularly visit their doctor.
If we look at those patients who were in the hospital and received treatment and had a target blood pressure level upon discharge, then the effect disappears after some time for various reasons. Almost the same 60% are outside target blood pressure levels. In approximately 2/3 of patients, this problem also occurs after inpatient selection of therapy.
Thus, this also does not provide significant progress.
What is the reason. This may be partly due to the fact that we overestimate our own capabilities. We conducted a large survey among doctors in St. Petersburg, Irkutsk, Leningrad region and other regions. How do they themselves evaluate the results of their treatment? In particular, the proportion of patients who actually achieve the target blood pressure level.
05:06
Today we can see that most doctors believe that up to 50 - 60% of their patients have target blood pressure levels. In fact, in a real situation it is approximately 5-10% of patients. This overestimation of our capabilities leads to the fact that we do not truly treat our patients.
According to modern data, true resistance to therapy is not so common - from 1 to 11% in specialized departments. No more than 5% of the entire population of patients with hypertension. More often it occurs in patients with severe organ damage, in patients with significant hypertrophy of the left ventricle, with damage to the fundus and kidneys.
Its prevalence increases with age. Most often observed in patients with diabetes (DM) and metabolic syndrome (MS).
Any organ damage (be it left ventricular hypertrophy, thickening of the intima media complex, the presence of plaques in the carotid arteries, severe retinopathy) is more common in patients who are resistant to therapy than in the average patient with increased blood pressure.
This problem, unfortunately, will become even more urgent. The life expectancy of the population is expected to increase. Data for the US and around the world. We expect an increase in the proportion of people over 60 years of age. Thanks to advances in healthcare, life expectancy in Russia is also increasing. Especially the elderly population in St. Petersburg, where we work.
The problem of old age is becoming urgent. There are more and more such patients. Almost any doctor knows that achieving target blood pressure levels in an elderly person is more difficult.
If we look at the statistical data, we note that with age, the prevalence of isolated systolic hypertension and the proportion of patients with insufficient blood pressure control increases.
The same problem is associated with the increasing prevalence of obesity and diabetes. The US has calculated the expected increase in obesity prevalence. From 1991 to 2001, the prevalence of both conditions in the United States almost doubled.
The same applies to the expected incidence of diabetes, the prevalence of which is believed to increase almost 25 times by 2005. We know well that lowering blood pressure is difficult.
07:41
If you look at all the large randomized trials, systolic blood pressure rarely drops below 140, the target blood pressure level. But if we isolate patients with diabetes, for whom the target blood pressure level is 130, then none of the studies we refer to when discussing the issue of antihypertensive therapy have ever reached this level of the average population.
This is due precisely to the fact that it is extremely difficult to cure such a patient to the target level. The body of a patient with diabetes stubbornly resists the therapy prescribed to it.
Today we must acknowledge the fact that the prevalence of therapy-resistant hypertension will only increase. This is due to the fact that we are dealing with:
- - aging population;
- - increasing prevalence of obesity;
- - decreased physical activity;
- — insufficient attention in general to systolic blood pressure;
- - increased consumption of various types of endogenous stimulants (including medications that prevent adequate reduction in blood pressure);
- - more stringent goals of the treatment itself.
Today we recalled modern target blood pressure levels.
According to the explanatory dictionary, what is a goal? This is the result to which our efforts are aimed. But 100% hitting the target does not always happen, even in sports. The real result is achieved, particularly in basketball, in about half the cases. We can say the same today about the success of treatment of hypertension.
09:11
The success of therapy very strictly depends on what goal we set for ourselves today. If once our target blood pressure level was 160 and 95, then we could very easily control 40% of patients. As soon as we set ourselves a target level, thanks to 140 and 90, the share of control immediately decreased to 10%.
Today, some honest studies that study patients with diabetes and set a target level of 130 and 80 indicate that the result in the population is achieved in approximately 1% of cases.
(Slide show).
I will show this using our own data on screening patients with hypertension in St. Petersburg. These are data from a real epidemiological study on a representative sample. You can see that the awareness of treatment is very low. The proportion of patients receiving treatment and the proportion of patients with blood pressure control, unfortunately, is only 2%, and not even 20%, which gives us official data on monitoring hypertension.
Classification of resistant hypertension. One of the common reasons is not resistance itself, but errors in measuring blood pressure and using the concept of resistance. There are specific reasons. In particular, secondary hypertension, which we sometimes do not diagnose, despite our knowledge in this matter.
Exogenous influences, among which we have not yet mentioned salt abuse today. This is one of the common reasons - insufficient restriction of sodium intake. Alcohol abuse.
Related factors. Obstructive sleep apnea syndrome, metabolic syndrome. It is very important in the work of a doctor - the imperfection of the prescribed therapy and violation of adherence on the part of the patient.
As for sleep apnea, I’ll literally show you very briefly. Among patients who receive three or more antihypertensive drugs in maximum doses, that is, they are truly resistant. In men, the prevalence of sleep apnea reaches 97%, in women 65%.
Women are the group for whom this problem is generally underestimated and little discussed. This data is really impressive and shows that this is a very important situation. It is not for nothing that in the American recommendations sleep apnea syndrome is considered one of the variants of secondary hypertension.
11:35
Today, thanks to this 2007 study, a connection between sleep-disordered breathing of any origin and resistance to therapy has been shown.
There is a myth that target BP is very dependent on adherence to treatment. Of course it is. The lower the adherence to treatment, the worse the ability to achieve the target blood pressure level.
We very often look for the causes of secondary hypertension in young people. In general, the recommendations always state that the younger the patient, the higher his blood pressure level, the more active our search should be for the cause of secondary hypertension.
However, I would like to draw your attention to the fact that the likelihood of secondary hypertension does not decrease with age, but only increases. At the age of 70 years it reaches 17.5%. This is a fairly significant number. Although on average we believe that only 10% of patients have secondary hypertension.
Currently, unfortunately, thanks to the introduction of strict standards for the treatment of hypertension, our diagnostic capabilities in the search for secondary hypertension are even somewhat reduced.
I would like to draw your attention to such an important cause of resistance to therapy as primary aldosteronism. Today, it is one of the most underdiagnosed conditions of hypertension. The higher the degree of pressure increase (especially in patients with resistant hypertension), the higher the prevalence of primary aldosteronism in the population of patients with hypertension. It reaches 20%. This is almost every fifth patient.
According to modern data, only 20% of patients with primary aldosteronism have such a symptom as hypokalemia. It may alert us to the presence of aldosteronism in patients.
13:33
Today, determination of renin activity in plasma aldosterone concentration is considered a mandatory study, which should be carried out if it is difficult to select therapy. The presence of a significant mass visualized in the adrenal glands is not necessarily present in this condition. Very often, these patients have benign bilateral adrenal hyperplasia, which is not visualized in any way and can only be diagnosed through hormonal studies.
Various studies were carried out in various clinics. In Seattle, in Birmingham, in Norway and in the Czech Republic. Almost all of these studies give the same twenty percent prevalence of aldosteronism in patients with resistant hypertension.
If we look generally at patients who have refractory hypertension, most of them say that 60% are due to drug causes. Our therapy is imperfect. We create our own problems of treatment resistance.
Another Rush study. The same 58% are reasons associated with the imperfection of the therapy itself. Of that 58 percent, 94 percent is occupied by suboptimal treatment regimens. Only a small proportion can be attributed to drug interactions and some other drug imperfections.
We tried to conduct the same study in Russia on our St. Petersburg population among patients who are being treated in our clinic. We got absolutely the same indicator, but differing by only 1% (59% of patients). The reason for resistance to treatment is the so-called drug causes. But even in a regular therapeutic area it is slightly less (about 46%).
One of the main reasons is clinical inertia, that is, the doctor’s lack of action regarding intensification of treatment if necessary. This is related to what I already said. We overestimate the success of the treatment. Sometimes we deliberately use various excuses in order not to intensify treatment.
In particular, that the patient is elderly, he may not tolerate it, and so on. Thus, we leave the patient at an unattained target blood pressure level.
15:57
In order to treat a patient with severe hypertension, three points must be taken into account:
- — patient commitment;
- - fight your own incompetence in this matter, namely the inertia of the doctor (although this is the absolute norm of human behavior):
- — overcome various mechanisms of blood pressure increase;
- - have a good organization of care for such patients.
The problem of therapeutic inertia exists absolutely everywhere. The problem here is not even the cost of the treatment. This has clearly been shown to be a problem even in studies where the drug is provided free of charge to patients.
Today, you need to change your own attitude in this treatment in order to understand that the target blood pressure level must be achieved in the patient at any cost. There was an interesting study published in 2002 comparing the two strategies.
Patients were initially treated according to routine guidelines. The strategy was then applied to achieve the target level at absolutely any cost, including a combination of four, five, six or more drugs. It was still possible to overcome resistance to therapy in most cases.
The current treatment algorithm for patients with resistant hypertension includes a mandatory assessment of one’s own adequacy of the therapy regimen and assessment of adherence to treatment. Mandatory diagnosis of obesity and sleep apnea syndrome. Mandatory analysis of concomitant therapy and analysis of the correctness of blood pressure measurement and accuracy.
In order to establish the cause of the increase in blood pressure, it is necessary to evaluate the home blood pressure level. Measure blood pressure by another person to rule out white coat hypertension. If necessary, carry out daily monitoring.
Review all therapy the patient is receiving. Discontinue medications that may increase blood pressure if possible. Study side effects of therapy. Conduct screening for the presence of sleep apnea syndrome (at least using questionnaires). Examine the patient in depth for secondary hypertension. Ensure that the patient adheres to a diet, exercise regimen, and be sure to limit table salt.
If necessary, consult a psychologist, even a psychiatrist. Panic attacks as a cause of a blood pressure crisis must be excluded. It is also important to pay attention to hemodynamic parameters. In particular, peripheral resistance and cardiac output.
18:31
Modern recommendations for the treatment of resistant hypertension, oddly enough, are quite scarce. Some of the most successful ones were published in 2006 (although there are also international recommendations). It states that if a patient receives three medications, including diuretics, and the target blood pressure is still not achieved, then we must necessarily reduce salt intake and adjust diuretic treatment taking into account renal function.
If your creatinine is normal, thiazide diuretics are the main choice. When creatinine is exceeded, loop diuretics are used. Vasodilators of an alternative class are necessarily used, and so on. If there is no effect, the patient is hospitalized in a specialized clinic.
Modern treatment combinations include combinations of many drugs (diuretics, beta blockers, calcium antagonists, long-acting drugs). Preferably fixed combinations. Original drugs with proven effectiveness must be used.
Even within the structure of one class, one should try to use drugs that are most effective in the regimen of each class and have proven their effectiveness in a number of clinical studies. If the effect is insufficient, low doses of spirinolactone or Verospiron are used. Central medications may also be effective.
If we are talking about calcium antagonists, without which it is impossible to treat a patient with resistant hypertension, then, for example, more modern third-generation calcium antagonists, such as the drug Lercanidipine, have a very long-lasting effect. They prevent problems with morning blood pressure rise, which provides a smoother antihypertensive effect and may help overcome treatment resistance.
When using this drug, there is no sympathetic stimulation associated with vasodilation. There is no effect that has a prohypertensive effect and activates other prohypertensive pathways during treatment. It is very important.
20:32
If we take the class of angiotensin II receptor blockers that we use in our patients, then also in the structure of this class, in addition to any organ-protective effects (which there is no time to talk about today, and you know about them well), you need to pay attention to the strength of the antihypertensive effect. It is not entirely unambiguous among representatives of the same class.
One of the new drugs “Olmesartan” or “Cardosal”, which has now appeared on the Russian market, gives a fairly significant reduction in blood pressure, more pronounced when using standard therapeutic doses than some other representatives of this class .
The addition of Veroshpiron is effective to a certain extent in most patients (and not only in patients with secondary or primary hyperaldosteronism). In this case, the Veroshpiron prescription test should not be used to diagnose aldosteronism. Overall, adding this drug as a fourth drug provides additional benefits.
Very briefly about new strategies in the treatment of such patients. Today, stronger natriuretics, sympatholytic drugs, and new vasodilators are used. In addition, non-pharmacological approaches are used. Such as devices that affect baroreceptors (continuous stimulation of baroreflexes).
Controlled breathing system. CPAP specific for the treatment of sleep apnea syndrome. Some drugs with alternative mechanisms of action. In particular, endothelin blockers. There is quite a lot of data on Darusentan.
22:06
(Slide show).
Thus, a system is implanted to stimulate the baroreflex, with bilateral implantation of special electrodes. Over time, it provides a significant reduction in systolic and diastolic blood pressure and heart rate.
(Slide show).
This is what an x-ray of a patient with an implantable device looks like. On both sides.
Today, this company has already created electrodes with unilateral implantation of a significantly smaller size. This technique is being developed very actively. Let’s say that an experimental animal’s blood pressure drops sharply. Today, more than two thousand patients in the world walk with similar implantable devices.
(Slide show).
This is what a CPAP therapy machine looks like. This is a nasal mask. It provides a fairly significant reduction in blood pressure while taking antihypertensive drugs.
Another new approach. Renal sympathetic nerve ablation procedure. It is performed as a standard angiography of the renal arteries. The procedure is similar to stenting. Apply 4 to 6 applications to each renal artery. After this, over time, a significant decrease in regional and total norepinephrine spillover is ensured.
During the year there was a significant decrease in blood pressure, up to 25–30 mm Hg. Art. on average for the group, which makes it possible to even cancel therapy in some patients.
New gene technologies are also being developed. In particular, “Antisence” technology. Today, experimental work already shows that blocking RNA of a number of receptors and proteins leads to a decrease in blood pressure.
The problems of gene therapy are quite large. But in the future this is also possible. The biggest problem is the safety of such treatment. Otherwise, we would probably today have approached gene therapy in relation, first of all, to the NO synthase gene, which Oksana Mikhailovna spoke about in such detail.
24:06
The vaccine against hypertension caused a great boom in the literature. Although it did not have major side effects, surveillance of these patients did not lead to widespread adoption of the vaccine. The costs and complexity of this treatment were not worth the results we had.
Resistant hypertension. How can we improve the result? The first thing I would like to say is. Never settle for missing your BP target. If you don't put up with this and try to improve the patient's prognosis, then patients will be more adherent to treatment.
You should always make sure your blood pressure measurement is correct. Always consider that the patient may not be fully compliant with treatment. It is always necessary to exclude secondary hypertension in such patients according to existing recommendations. Try to change the therapy, make it more rational. Never be afraid of a large number of drugs if they are prescribed in rational combinations.
Use fixed combinations to increase adherence and reduce polypharmacy. Do not hesitate to consult a specialist if you have such a need.
The main principle today is aggressive therapy against aggressive hypertension. In such a situation, I think that hypertension will definitely give in under our pressure.
Thank you for your attention.
Grigory Arutyuno in: Alexandra Olegovna, thank you very much for this wonderful emotional and very deep report. Several questions have come to your name. If you allow me, I will voice them.
Question: When can we conclude that hypertension is resistant? After what time?
Asks the doctor who works in the clinic.
Alexandra Conradi : Today, different specialists devote different amounts of time to our patients. In general, we can suspect this problem after a month. But to make such a diagnosis 100%, it will still take us three to six months.
It takes time to develop the full effect of all drugs and to work out therapy.
26:12
Grigory Arutyunov: Thank you very much. Second question.
Question: What therapy for systolic hypertension in the elderly is most effective?
Alexandra Conradi: The most effective today is still the use of dihydroperidine calcium antagonists and thiazide diuretics. Isolated by systolic hypertension.
The only problem can be that this therapy is not always well tolerated. Angiotensin II receptor blockers are gaining ground in systolic hypertension. Although, in my opinion, no drug has yet been able to defeat calcium antagonists in this category of patients.
Grigory Arutyunov : A question from real life.
Question: In your personal practice, was there a situation where resistance could not be overcome? What have you done?
Alexandra Conradi : Of course it was. We have a lot of such patients. A whole center for resistant hypertension has been organized. We began the procedure of radiofrequency ablation of the renal arteries. There are 5 patients under our supervision. In the near future there will be 10 of them. We will be happy to share this data.
The problem will always remain patients who are not amenable to therapy. It is for them that alternative approaches are being developed. We must look for another way out. Due to the pronounced remodeling and problems the patient has, drug therapy cannot provide treatment for all patients.
27:38
Grigory Arutyunov : Thank you very much for your very honest and professional answer.
But there is still a question.
Question: Are there any biochemical markers of resistant hypertension?
Alexandra Conradi : Unfortunately, no. Even today I did not dwell on the studies that were conducted regarding what predictors exist, how the patient will respond to therapy, and so on.
Algorithms were used very often. Let's say high renin, low renin. Depending on this, select therapy. They do not justify themselves clinically. The effect of treatment is often unpredictable.
The only approach that more or less works is hemodynamic. If we determine the level of cardiac output and the level of peripheral vascular resistance, then where the latter is increased, add a large number of vasodilators, up to the desired effect.
Where there are patients with high output, it is necessary to give beta-blockers. Although this is no longer fashionable in the treatment of hypertension. This provides them with an additional antihypertensive effect.
As for biochemical markers, how does a patient with resistant hypertension differ from a normal one? There is no clinically reliable one.
Grigory Arutyunov: Thank you. Last little question.
Question: How to distinguish “white coat” hypertension from what you were talking about – resistant hypertension?
Alexandra Conradi : In real life, the simplest thing is to ask the patient to bring a diary of self-monitoring of blood pressure, see what pressure he has at home. If you don't trust someone to measure correctly, you can even ask your nurse to take your blood pressure outside of the doctor's office. This causes less of a “white coat” effect.
In difficult cases - 24-hour blood pressure monitoring. It also has its problems. The patient also reacts to the monitoring procedure. Everything is different. This method, although much praised, is not ideal for diagnosing white coat hypertension.
Grigory Arutyuno in: Thank you very much, Alexandra Olegovna, for these deep, comprehensive answers. Thank you for your lecture and your answers.
Until next time.
29:55
Patient characteristics and comorbidities
Resistant hypertension
A large analysis suitable for evaluation is the study by Sim et al. more than 470 thousand patients with hypertension enrolled in the Southern California healthcare system between January 1, 2006 and December 31, 2007.
- Overall, 60,327 patients with hypertension met the criteria for resistant hypertension. This represents 12.8% of all patients with hypertension and 15.3% of those receiving medications.
- older age,
- diabetes,
Refractory hypertension
- In the cross-sectional analysis of the Reasons for Geographic and Ethnic Differences in Stroke (REGARDS) cohort discussed above, the strongest predictor of refractory hypertension was African American race, with a prevalence ratio of 4.88 (95% confidence interval, 2.79–8.72). African race was also a strong independent risk factor for the development of refractory hypertension in the study by Modolo et al.
- In studies at the University of Alabama, refractory hypertension was more common in African Americans than in whites.
Overall, these studies suggest that, as with resistant hypertension, obesity and African ancestry . Also similar to resistant hypertension, comorbidities commonly associated with refractory hypertension include diabetes, chronic kidney disease, heart disease, and stroke .
Forecast
Resistant hypertension
An increasing number of longitudinal and prospective studies clearly demonstrate that patients with resistant hypertension have an increased risk of cardiovascular and renal complications and all-cause mortality compared with patients with more easily controlled hypertension.
- For example, researchers assessed the risk of stroke and coronary heart disease and all-cause mortality among 2,043 REGARDS participants with resistant hypertension relative to 12,279 REGARDS participants with controlled hypertension treated with <4 classes of antihypertensive medications or uncontrolled hypertension treated with 1 or 2 classes of antihypertensive medications. .
- Resistant hypertension was divided into 2 subgroups, including participants with controlled hypertension with ≥4 classes of antihypertensive medications (ie, controlled resistant hypertension) and uncontrolled hypertension with ≥3 classes of antihypertensive medications (ie, uncontrolled resistant hypertension).
- Over a mean follow-up period of 5.9 years and after multivariable adjustment, the risk of stroke was found to increase by 25% (hazard ratio, 1.25; 95% confidence interval, 0.94–1.65) compared with participants without resistant hypertension.
- During a mean follow-up period of 4.4 years, the risk of developing coronary heart disease was found to increase by 69% (1.69; 1.27-2.24) and overall mortality by 29% (1.29; 1.14-1.46). ) over an average observation period of 6 years.
- Compared with controlled resistant hypertension, uncontrolled resistant hypertension was associated with an increased risk of coronary heart disease (2.33; 1.21–4.48), but not stroke or death.
- Having controlled resistant hypertension does not increase the risk of stroke, coronary heart disease, or death relative to participants without resistant hypertension.
In an analysis of antihypertensive and lipid-lowering treatments to try to prevent myocardial infarction, researchers determined that the risk of stroke, coronary heart disease, peripheral artery disease, end-stage renal disease, and all-cause mortality in participants with controlled resistant hypertension (n=1870) relative to participants without resistant hypertension ( n=12814) was defined by BP control using ≤3 antihypertensive medications. The average follow-up period was 4.9 years.
- The incidence of all outcomes, as well as overall mortality, increases in patients with resistant hypertension.
- The risk of developing end-stage kidney disease (95%), congestive heart failure (88%) and stroke (57%) increases significantly.
- The risk of developing chronic heart disease and peripheral artery disease increases by 44% and 23%, respectively.
- Overall mortality increased by 30% compared with study participants without resistant hypertension.
- Interestingly, the estimated rates of development of chronic heart disease, congestive heart failure, peripheral arterial disease, and end-stage renal disease were each higher among patients with controlled resistant hypertension relative to participants without resistant hypertension, leaving a residual risk of developing cardiovascular and renal disease even after diagnosis. control over blood pressure when using 4 or more drugs.
- These two studies, as well as the prospective studies, clearly show that hypertension that requires the use of 4 or more drugs generally increases the risk of cardiovascular and renal complications and the risk of death, compared with hypertension that is controlled by the use of 3 or more less drugs.
Refractory hypertension
Outcomes, including all-cause mortality, have not yet been assessed for patients with refractory hypertension.
- Given the history of long-standing, uncontrolled, and often severe hypertension, the risk of sudden cardiovascular events such as stroke and congestive heart failure may be increased.
- It seems intuitive that patients with refractory hypertension have a greater risk of cardiovascular events and death relative to patients with controlled hypertension, but evidence of such a higher risk is currently lacking.
Mechanisms of resistant versus refractory hypertension
- Most of the literature agrees that persistent intravascular fluid retention is a common cause underlying resistant hypertension. For example, Thaler et al. demonstrated that patients with true resistant hypertension are characterized by increased vessel wall distension, assessed by chest fluid.
- In turn, numerous studies indicate that increased aldosterone levels play a role in persistent fluid retention.
- Additional factors also contribute to inappropriate fluid accumulation. Known risk factors for developing resistant hypertension include salt sensitivity, African-American race, older age, chronic kidney disease, and diabetes. High salt concentrations, common in most countries around the world, have been shown to directly contribute to fluid retention and the development of resistant hypertension, although excess fluid retention is not consistently associated with high salt intake in animal models of hypertension and generalized cohorts of hypertension.
- The etiology of refractory hypertension may be completely different and independent of the volume of intravascular fluid.
- A retrospective analysis by Acelajado et al. showed that persistent intravascular fluid retention is unlikely to explain the failure of antihypertensive therapy that occurred in all patients with refractory hypertension who were treated including the combination of chlorthalidone and spironolactone along with many other classes of drugs.
- In addition, despite significantly higher basal blood pressure levels, the antihypertensive response to spironolactone was much less in patients with refractory hypertension relative to those in whom blood pressure could be controlled (<140/90 mmHg). This minor effect was observed even when using high doses of spironolactone when compared with the control group.
- The failure of such intensive diuretic therapy, including high doses of spironolactone, suggests that the mechanism of treatment failure is not related to inappropriate fluid retention.
- If this is true, then this feature has important clinical implications; additional intensification of diuretic therapy is unlikely to provide any improvement in blood pressure control while the risk of diuretic-related adverse events increases.
- These data are based on observation of premeasured, high resting heart rates in individuals with refractory hypertension compared with individuals with controlled resistant hypertension.
- This study again observed high office heart rates in patients with refractory hypertension, as reported by Acelajado. High heart rate levels were confirmed by ambulatory monitoring with a greater difference at night (72.7 ± 9 beats/min in refractory hypertension vs. 65.6 ± 9 beats/min in controlled resistant hypertension).
Resistant arterial hypertension
Arterial hypertension (AH) is defined as resistant (refractory) if, while taking three or more antihypertensive drugs of different classes (one of which is a diuretic) in doses close to the maximum, it is not possible to achieve a target blood pressure (BP) < 140/90 mm rt. Art. in most patients with hypertension (or < 130/80 mmHg in patients with diabetes mellitus and renal failure).
The ALLHAT study found that approximately 47% of patients remained resistant to antihypertensive therapy one year after randomization, despite the rigorous titration and drug combination regimens used in the study. Similar results (43% resistant patients) were obtained in the Syst-Eur Study. According to Yakovlevitch and Black, suboptimal drug regimen is the most common cause of resistance (43%), the next most common cause is drug tolerance (22%), followed by secondary hypertension (11%), low compliance (10%).
Refractory hypertension (RAH) can be divided into two broad categories: true RAH and pseudo-resistant hypertension.
PSEUDO-RESISTANT AG
Problems associated with blood pressure measurement
A large number of publications in the medical press and guidelines are devoted to the basic rules for measuring blood pressure, as well as technical factors influencing blood pressure levels. However, general practitioners often neglect the existing rules for measuring blood pressure, which entails a number of errors:
- using a small cuff;
- measuring blood pressure without prior rest;
- rapid release of air from the cuff:
- measuring blood pressure on one arm;
- auscultation before palpation blood pressure measurement.
Pseudohypertension is diagnosed quite rarely: in the case when blood pressure measured using the Korotkoff method does not correspond to the true (intra-arterial) blood pressure level. This phenomenon, associated with severe atherosclerosis and calcification of the brachial and radial arteries, is observed in elderly patients. Thickening and compaction of the arterial wall with age leads to the fact that in order to achieve compression of a stiff artery, a higher pressure (above the true one) is required in the cuff, which leads to an overestimation of blood pressure figures. The presence of pseudohypertension in a patient can be suspected if the following signs are present:
- absence of target organ damage;
- calcification of the brachial and other arteries according to research data (X-ray, ultrasound);
- Blood pressure in the brachial artery is higher than in the legs (which once again illustrates the need for a complete propaedeutic examination of the patient);
- symptoms of hypotension during antihypertensive therapy in the absence of a pronounced decrease in hypertension (usually interpreted in elderly patients as a worsening of the neurological symptoms of dyscirculatory encephalopathy in the vertebrobasilar region);
- severe systolic hypertension.
The existence of pseudohypertension can be verified by the presence of Osler's sign - palpation of the brachial artery even when the intracuff pressure exceeds systolic blood pressure. Final confirmation of the diagnosis is possible only with intra-arterial blood pressure measurement.
Low compliance
Compliance (patient adherence to therapy) is defined as the patient's ability to accurately follow clinical instructions for taking medications and lifestyle modifications. Taking medications in accordance with medical prescriptions in at least 80% is the most common characteristic of medication compliance. Low compliance occurs in more than 50% of patients, including those included in clinical trials. It is noteworthy that the number of patients with low adherence to therapy decreased to 10% among patients observed by specialists in the treatment of hypertension (USA), which demonstrates the importance of specialist qualifications and the lack of time factor in communication with the patient, which is present with general practitioners.
Numerous factors, such as the cost of medications, the low intellectual level of the patient, the complexity of the administration and dosage regimen, etc., should be analyzed by the doctor when diagnosing RAG and suspecting low adherence to therapy. Careful questioning remains one of the best methods for determining whether a patient is adherent to treatment. The clinician should set realistic short-term goals for all specific components of treatment (weight control, salt reduction, physical activity, alcohol reduction, and, if possible, a single or double dosage regimen) and individualize their recommendations as much as possible based on the specific clinical situation, social and family characteristics of the patient.
Errors in prescribing medications
Such errors are a common cause of the development of pseudo-resistant hypertension. Despite the huge number of clinical studies, the constant publication of research and methodological materials in the medical press, widespread discussion of the rules of prescription and combination of drugs among general practitioners and cardiologists, errors in the dosing and combination of antihypertensive drugs are quite common.
Modern tactics of drug antihypertensive therapy provide the possibility of choosing between monotherapy and combination therapy. To achieve target blood pressure levels in most patients, especially with grades I–III increases in blood pressure, combination therapy is required.
Among the advantages of combination antihypertensive therapy are the following:
- the use of drugs with different mechanisms of action makes it possible to control several pathogenetic links of hypertension;
- the drugs included in the combination are used in lower doses, which reduces the likelihood of side effects;
- when prescribing fixed combinations (two drugs in one tablet), adherence to therapy improves.
The following drug combinations are considered effective and well tolerated:
- diuretics and β-blockers (atenolol, bisoprolol);
- diuretics and ACE inhibitors (captopril, lisinopril, enalapril) or angiotensin II receptor antagonists (valsartan, losartan);
- calcium antagonists (dihydropyridines: amlodipine, nifedipine) and β-blockers;
- calcium antagonists and ACE inhibitors or angiotensin II receptor antagonists;
- calcium antagonists and diuretics;
- α-blockers (doxazosin, terazosin) and β-blockers.
Other combinations with centrally acting drugs (α2-agonists, imidazoline I2 receptor agonists), as well as a three- or more-component regimen can be used.
It is recommended to use long-acting drugs that provide an effect within 24 hours and require a single dose per day, which significantly improves adherence to therapy.
An inadequate regimen of drug use means the prescription of antihypertensive drugs in low doses, the use of pathogenetically illiterate combinations (drugs of the same class, for example verapamil and dihydropyridine, or drugs with a similar mechanism of action - an ACE inhibitor and an angiotensin II receptor antagonist - or similar side effects).
The algorithm for optimizing antihypertensive therapy is shown in Figure 1.
| Figure 1. Algorithm for optimizing drug therapy |
Thus, in the case of resistant hypertension, the clinician must carefully analyze the prescribed antihypertensive therapy regimen: make sure that the prescribed doses are adequate and the pathogenetic justification of the combinations used, as well as the correctness of the prescribed therapy regimen (correlation between the duration of action and the frequency of drug administration). If necessary, another drug should be added to the regimen used, taking into account the individual characteristics of the patient (target organ damage, associated and concomitant pathology).
TRUE RESISTANT AG
Increased variability and reactivity of blood pressure
“White coat hypertension” (“office hypertension”, “office hypertension”) is defined as a state of stable increase in blood pressure during measurement at a doctor’s appointment with normal values outside the hospital. Considered as a manifestation of stress-induced hypertension. According to Brown et al., 2-3 out of every 10 patients with resistant hypertension have good blood pressure control (mean value less than 135/85 mm Hg) with 24-hour blood pressure monitoring. Patients with this phenomenon often demonstrate increased sensitivity to antihypertensive drugs, which significantly reduce “non-stress” blood pressure and can cause symptoms of hypotension. In this case, patients independently discontinue antihypertensive drugs or begin to take them chaotically, which significantly complicates the management of these patients and reduces compliance.
In this case, it is recommended to carry out out-of-office blood pressure measurements (24-hour monitoring and blood pressure self-monitoring diaries) before adjusting the antihypertensive therapy regimen. Despite the relative simplicity of diagnosing this phenomenon, clinicians often underestimate its prevalence and significance, which leads to errors in the selection of drug therapy regimens and decreased compliance.
Baroreflex failure
Blood pressure instability with periods of significant increases and decreases occurs in patients with damage to baroreflex function. This condition is quite rare and very difficult to diagnose.
Physiological resistance (volume overload)
The most common cause of physiological resistance to hypertension is volume overload. Excessive salt intake may cause the development of RAH in treated patients. The use of direct vasodilators (minoxidil, hydralazine), adrenergic blocking drugs (α-blockers and β-blockers) and large doses of potent diuretics can lead to increased fluid retention and the formation of RAG. The most common cause of persistent hypervolemia is the administration of a single daily dose of furosemide. The decrease in intravascular volume within a few hours of furosemide is followed by activation of the renin-angiotensin-aldosterone system (RAAS) with sodium retention mechanisms that restore all lost sodium during the brief interval of natriuresis. If renal function is preserved, a morning dose of long-acting hydrochlorothiazide (12.5–25 mg) can break this vicious cycle. All drugs that lower blood pressure also reduce renal perfusion pressure and glomerular filtration, which leads to sodium and fluid retention.
Unfortunately, many patients with RAH who are receiving multiple antihypertensive medications are not prescribed diuretics in adequate doses. Limiting salt intake in itself leads to adequate control of circulating plasma volume, lowering blood pressure, improving treatment tolerability, and reducing the number of antihypertensive drugs used. With a decrease in salt intake, the effectiveness of all antihypertensive drugs increases, with the exception of calcium antagonists.
If volume overload is suspected, the amount of sodium in 24-hour urine should be determined. At the same time, inadequacy in the implementation of dietary recommendations is often found in patients who claim to follow a low-salt diet. In patients who do not follow a low-salt diet, sodium excretion increases.
Drug interactions
Identification of drugs that reduce the effectiveness of antihypertensive therapy is extremely important, as it helps to individually optimize therapy in patients, taking into account the mechanism of action of the drugs used. Let's focus only on the most frequently used ones.
Steroids. Hypertension is reported in more than 20% of patients taking synthetic corticosteroids. Taking these drugs can also cause hypertension resistance. A risk factor for the development of RAH is old age. Medicinal substances such as natural licorice, phenylbutazone, carbenoxolone, prednisolone, and cortisol preparations have mineralocorticoid activity. Taking these drugs in moderate doses can lead to pseudohyperaldosteronism (sodium retention, hypervolemia, hypokalemia with metabolic alkalosis and suppression of plasma renin and aldosterone). Ointments, antihemorrhoidal drugs, eye drops, inhaled bronchodilators, nasal antiallergic sprays may contain substances with significant mineralocorticoid activity. Some of these drugs may contain sympathetic amines. To reduce blood pressure and overcome refractoriness, it is necessary to stop using these drugs. In cases where steroid therapy is mandatory, diuretics are effective drugs. Potassium monitoring is necessary during diuretic therapy, since these drugs can increase hypokalemia in steroid-dependent hypertension.
Sex hormones. Oral contraceptives are capable of inducing hypertension in approximately 5% of cases when using high-dose combinations of estrogens and progestins. Risk factors for the occurrence and worsening of hypertension are smoking, obesity, race (African Americans), diabetes, and renal pathology. Cases of the development of malignant hypertension while taking oral contraceptives have been described. The next risk group for developing RAG is men taking estrogens for the treatment of prostate cancer. Danazol, a semisynthetic androgen used to treat endometriosis and hereditary angioedema, can lead to hypervolemia and worsening hypertension.
Drugs affecting the sympathetic nervous system . Phenylephrine, prescribed in the form of eye drops, and adrenaline-like substances used topically for glaucoma, can lead to an increase in blood pressure in normotensive patients and patients with hypertension. Adding α-blockers, α- and β-blockers to the antihypertensive regimen neutralizes these effects.
Most undesirable anorectics consist of a combination of antihistamine-like substances and adrenergic agonists (usually phenylpropanolamine, ephedrine, pseudoephedrine, or caffeine). α-adrenergic intoxication induced by nasal and oral decongestants and antitussives containing large doses of oxymetazoline, phenylephrine, and ephedrine can induce hypertension or aggravate existing pathology. The drugs of choice are α-blockers, α- and β-blockers.
Non-steroidal anti-inflammatory drugs. NSAIDs may potentiate the increase in blood pressure and compete with antihypertensive drugs. NSAIDs increase the risk of developing hypertension by 40%. NSAIDs interact with some antihypertensive drugs, such as diuretics, beta-blockers, ACE inhibitors, but not with calcium channel blockers - centrally acting drugs whose antihypertensive effectiveness is not related to the production of prostaglandins. Indomethacin, piroxicam, and naproxen cause significant increases in blood pressure, while sulindac and full-dose aspirin have the least effect on blood pressure. Minimum doses of aspirin do not affect blood pressure in patients with hypertension. Selective cyclooxygenase-2 inhibitor drugs (celecoxib, rofecoxib) do not increase blood pressure and do not have dose-dependent effects on blood pressure. Meta-analyses have shown that NSAIDs lead to an increase in mean blood pressure of 4–5 mmHg. Art. They cause sodium retention and increased sensitivity to pressor hormones. Given the high prevalence of joint and spine diseases among elderly patients, clinicians should be keenly aware of the possible interactions of NSAIDs with antihypertensive drugs.
Tricyclic antidepressants. Tricyclic antidepressants antagonize the hypotensive effects of adrenergic blockers such as guanethidine, which can lead to a significant increase in blood pressure. These drugs prevent the accumulation of antihypertensive drugs in adrenergic nerve endings, where they block the transmission of nerve excitation. Similar interactions have been described for other antihypertensive drugs (methyldopa, clonidine).
Associated states
Metabolic syndrome and obesity. The prevalence of metabolic syndrome is currently becoming epidemic and in some countries, including Russia, reaches 25–35% among the adult population.
In patients with metabolic syndrome, the effectiveness of antihypertensive drugs is reduced, and a two-component regimen, as a rule, does not allow achieving target blood pressure. This is due to the pathogenetic features of hypertension in metabolic syndrome.
Normally, insulin has vascular protective effects and causes insulin-mediated vasodilation. But with chronic hyperinsulinemia and insulin resistance, other pathophysiological mechanisms leading to hypertension are triggered: stimulation of the sympathetic-adrenal system (SAS), RAAS; an increase in the content of intracellular Na+ and Ca2+, a decrease in K+ with an increase in the sensitivity of the vascular wall to pressor influences; increased reabsorption of Na+ in the proximal and distal tubules of the nephron (fluid retention with the development of hypervolemia). Of particular importance is the stimulation of proliferation of smooth muscle cells of the vascular wall under the influence of hyperinsulinemia (narrowing of arterioles and increased vascular resistance).
Failures in the treatment of hypertension in metabolic syndrome are usually due to the focus of therapeutic tactics only on hypertension. Successful therapy is based on the principle of simultaneous correction of all links in the pathogenesis of metabolic syndrome, a comprehensive impact on the causes and consequences of insulin resistance: lifestyle changes, treatment of obesity, treatment of carbohydrate metabolism disorders, treatment of dyslipidemia. When selecting antihypertensive therapy, the following features should be taken into account: metabolic effects of antihypertensive drugs (effect on lipid spectrum, insulin resistance, glucose and uric acid levels); the need for more frequent use of a 3- and 4-component therapy regimen with an impact on various parts of the pathogenesis of hypertension characteristic of metabolic syndrome.
Smoking leads to a transient increase in blood pressure and increased blood pressure variability. With a large number of cigarettes smoked, the duration of episodes of hypertension increases. The antihypertensive effectiveness of β-blockers in smoking patients with hypertension is reduced.
Alcohol. Alcohol abuse (chronic alcohol intoxication) leads to increased blood pressure in normotensive patients and induction of resistance to antihypertensive drugs. There are dose-dependent hypertensive effects of alcohol. The main type of treatment is to stop or reduce drinking. In some cases, stopping alcohol intake does not improve blood pressure control.
Genetic features
The polygenic syndrome of essential hypertension includes a wide range of hemodynamic and neuroendocrine features. Thus, plasma renin activity partially determines individual sensitivity to β-blockers, ACE inhibitors, and angiotensin II receptor antagonists. The connection between changes in the angiotensinogen gene and salt sensitivity is widely known. Genetically determined changes in drug metabolism, such as accelerated metabolism (hydralazine), have been described, but significant genetic features of metabolism have not been confirmed for the main classes of antihypertensive drugs. It is generally accepted that sensitivity to diuretics is high and relatively low to ACE inhibitors, β-blockers, and angiotensin II receptor antagonists in black patients.
Secondary forms of hypertension
Progression of renal failure is the most common and easily diagnosed cause of hypertension resistance. Renovascular disease is common among patients with previously controlled hypertension, especially if atherosclerotic lesions were present in other vascular territories. Over the past few years, the understanding of the impact of primary hyperaldosteronism (PHA) on the prevalence of RAH has changed significantly. Researchers have noted a high incidence of PHA. Many of these patients have normal plasma potassium levels but elevated plasma aldosterone relative to renin. Most of them are diagnosed with bilateral adrenal hyperplasia, for which surgical treatment is not indicated. The drug of choice in this case is spironolactone.
Obstructive sleep apnea syndrome (OSAS) . According to H. Issakson et al., among patients with refractory OSA is detected in 56% of cases.
Typical “morning” hypertension caused by OSA, predominantly diastolic, is difficult to correct with conventional antihypertensive drugs. Clinicians often underestimate the significance of this condition and do not include questions regarding the patient’s snoring and the presence of sleep apnea in the traditional history-gathering scheme. And this is necessary especially in obese patients.
There are quite contradictory data regarding the effectiveness and safety of antihypertensive drugs of various groups in patients with OSA. Thus, a number of side effects have been identified during treatment with certain antihypertensive drugs, in particular, inhibition of muscle tone in the upper respiratory tract during treatment with β-blockers, α-methyldopa, as well as as a result of metabolic alkalosis caused by diuretics. Other studies confirm the positive effects of diuretics in the form of a reduction in the number of episodes of breathing disorders during sleep. Clearly positive data have been obtained with the use of calcium antagonists and ACE inhibitors.
However, for successful treatment of hypertension in OSA, it is necessary to carry out a set of therapeutic measures aimed at eliminating OSA. The most effective treatments currently are uvulopalatopharyngoplasty and CPAP therapy (continuous positive airway pressure).
The diagnostic algorithm for RAG is presented in Figure 2.
It must be remembered that the cause of hypertension resistance can be a combination of several exogenous factors and also secondary forms of hypertension. Treatment of RAG involves the elimination of exogenous factors and the use of maximum tolerated doses of drugs in a multicomponent treatment regimen, including long-acting diuretics. Many studies prove the necessity and advisability of adding spironolactone to a 3- or 4-component therapy regimen in patients with RAG.
Literature
- Oparil S., Michael A. Weber. Hypertension: A Companion to Brenner and Rector's The Kidney, 2000.
- Erdine S. Resistant hypertension. ESH. Scientific Newsletter, 2003; 4: N15.
- Hypertension Primer, Third Edition, 2003 American Heart Association.
- European guidelines for the diagnosis and treatment of arterial hypertension, 2003.
T. V. Adasheva, Candidate of Medical Sciences, Associate Professor MGMSU, Moscow