: March 21, 2021, Masters of the Heart, volume 73, no. 1
A huge role in the life of our body is played by the autonomic (autonomous) nervous system, which, like an octopus, has spread its “tentacles” throughout the body. Innervating internal organs such as the heart, intestines, endocrine glands, etc., based on feedback, it regulates the most important functions of the body, from breathing to reproduction. Many cardiovascular pathologies are associated with disruptions in the functioning of this system. Specialists of the Center for Interventional Cardiology of the Siberian Federal Biomedical Research Center named after. acad. E. N. Meshalkina was one of the first in the world to use minimally invasive technology for the treatment of ventricular arrhythmias by blocking nerve impulses coming from the kidneys
A healthy heart beats in a certain rhythm that corresponds to the physiological state of the body. However, diseases of the cardiovascular, nervous and endocrine systems, as well as severe stress, excess weight, alcohol and smoking abuse, and even a drop in potassium levels in the blood, can cause a whole range of cardiac disorders, from arrhythmia to extrasystole, characterized by extraordinary contractions.
Arrhythmias are divided into groups depending on in which part of the heart the malfunctions occurred: in the atria, the sinus-atrial node (the “driver” of the heart rhythm) or the ventricles, which play the role of a pressure pump. Most of these disorders are closely related to the state of the autonomic nervous system, which regulates the activity of all internal organs.
Ventricular heart rhythm disturbances can be either congenital or acquired. For example, they may be a consequence of a structural pathology of the heart - a scar that appears as a result of myocardial infarction. In any case, they are life-threatening types of arrhythmia and, without emergency medical care, can cause sudden death.
What is the essence of renal denervation?
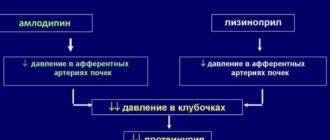
The kidneys play a key role in regulating blood pressure. Medicines that lower blood pressure affect the renal mechanisms to varying degrees. But in some cases, even a combination of three or four drugs with different mechanisms of action does not allow normalization of blood pressure. In such cases, they speak of refractory arterial hypertension. It turned out that in refractory hypertension, maintaining a high level of blood pressure occurs due to the excessive release of norepinephrine, a hormone that increases hypertension. The nerve cells that produce norepinephrine are found in the arteries that supply blood to the kidneys. If the activity of these cells is suppressed, blood pressure normalizes.
Radiofrequency ablation (denervation) of the renal arteries without taking into account the cost of consumable instruments - 60,000 - 120,000 rubles.
Denervation of the renal arteries using a Vessix catheter - RUB 250,000.
Included in the price:
manipulation, hospital stay, dressings, postoperative observation by the attending physician, medications and nutrition
20-30 minutes
(duration of procedure)
1 day in hospital
Indications
- refractory arterial hypertension, i.e. inability to achieve the target blood pressure level (BP below 140/90 mm Hg), despite taking three or more antihypertensive drugs, including diuretics;
- a large number of medications taken by a patient with arterial hypertension for other diseases;
- inability to adequately take medications to reduce arterial hypertension due to side effects.
Contraindications
- allergy to iodine-containing contrast agent;
- pregnancy;
- severe renal failure;
- acute inflammatory diseases.
Main results
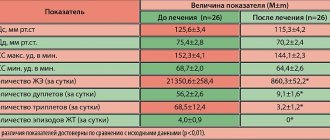
- Patients who underwent renal denervation showed a statistically significant decrease in daytime, nighttime, and 24-hour SBP compared with the control group (mean difference, -6.0 mmHg)
- The smoothing index was significantly higher in patients in the renal denervation group (1.4 ± 1.2) compared with the control group (0.9 ± 0.6, P = 0.02), while no statistically significant differences were found in the standard deviation of SBP , DBP, stiffness index and percentage of non-dippers.
- The number of patients who responded to therapy was significantly higher in the study group (44.5% vs. 20.8%; P=0.01).
- The number of patients with isolated systolic hypertension did not differ significantly between responders and non-responders to treatment (25% vs. 37%).
- In stepwise discriminant analysis, baseline mean nighttime SBP and standard deviation of nighttime SBP were significant predictors of treatment response (P=0.005).
- Area under the curve (AUC) was 0.65 (95% CI: 0.486–0.816; P=0.07) for baseline mean nighttime SBP and 0.72 (95% CI: 0.565–0.874; P=0.005) for baseline mean nighttime SBP deviation time.
- For the initial average SBP at night, the threshold is 136 mm Hg. Art. was the best compromise between sensitivity (75%) and specificity (54%) for predicting response to therapy.
- For the standard deviation of SBP at night, the threshold is 12 mmHg. Art. was the best compromise between sensitivity (55%) and specificity (83%) for predicting treatment response.
Reviews of doctors providing the service – Denervation of the renal arteries
I had surgery on 2 legs with Yuri Stanislavovich Malakhov.
I want to express my deep gratitude to him for a new breath of life, lightness on my feet, one might say, a completely different standard of living. Yuri Stanislavovich, you have golden hands and you are a doctor from God! I recommend it to everyone, women and men - don’t be afraid and... Read full review Irina Nikolaevna G
11.06.2021
I would like to sincerely thank the surgeon-phlebologist Yuri Stanislavovich Malakhov for the high-quality treatment of varicose veins using a modern method: no incision, no hospitalization, high cosmetic effect. The very next day I went to work. Yuri Stanislavovich is a professional... Read full review
Natalia Viktorovna F
18.04.2021
Treatment options for resistant arterial hypertension
Today, a cardiologist has about 40 antihypertensive drugs in his arsenal, however, even when rational combinations are used, it is not always possible to achieve target blood pressure.
Even with rational pharmacotherapy, target blood pressure can be achieved in no more than 35% of patients. The exact prevalence of resistant hypertension is unknown. According to large centers, its frequency can reach 10–13% [4, 5], and this figure remains high even after excluding pseudo-resistant hypertension associated with “white coat” hypertension, errors in blood pressure measurement, etc.
For many years, the only way to normalize blood pressure in patients with true resistant hypertension was the prescription of polypharmacotherapy with the simultaneous use of 4–6 or more drugs. However, such treatment tactics often led to the development of serious side effects.
As is known, the sympathetic nervous system (SNS) is one of the main pressor mechanisms, and its activation is a key factor in the development of essential hypertension. Hyperactivation of the SNS and a progressive increase in blood pressure mutually reinforce each other and participate in the formation of a vicious circle. Increased activity of the SNS most affects the kidneys. With hyperactivation of the SNS in the kidneys, vasoconstriction occurs, blood flow and filtration decrease, renin secretion increases, and sodium and water reabsorption increases. Afferent impulses from the kidneys enter first the lateral horns of the spinal cord, and then to the vascular center in the central nervous system, contributing to an increase in blood pressure. It increases with stretching of mechanoreceptors, renal ischemia, and under the influence of hypoxia [6].
The search for non-drug methods of treating hypertension, allowing to control the effects of the SNS and regulate its excessive activity, has been going on for quite some time. Manipulation of the sympathetic nerves as one of the types of treatment tactics was considered even before the advent of modern antihypertensive pharmacotherapy. Radical surgical methods of thoracic, abdominal and pelvic sympathetic denervation, and later partial sympathectomy, were relatively successfully used to lower blood pressure in patients with so-called malignant hypertension in the first half of the 20th century. However, these operations were associated with high mortality and the risk of complications both immediately after the intervention and delayed ones, including gastrointestinal dysfunction and pelvic disorders [7–9]. It is not surprising that with the advent of effective antihypertensive drugs, such surgical interventions have become very unattractive for both doctors and patients.
At the beginning of the 21st century, researchers again turned to the idea of influencing the renal sympathetic nerves, but using minimally invasive technologies.
How is renal denervation performed at the CELT clinic?
The procedure is performed without anesthesia, with local anesthesia. In this case, a special catheter in the form of a balloon is inserted through a puncture of the radial or femoral artery under angiographic control, on which point electrodes are located. The essence of the procedure is short-term radiofrequency destruction (ablation) of cells that secrete norepinephrine. The balloon is inserted into the trunk of each renal artery in turn, delivering high-frequency wave energy. The high-frequency impulse destroys the fibers of the nerves passing through the wall of the vessel, as a result of which irritating impulses do not reach the brain, and blood pressure is normalized. The duration of the intervention is 20-30 minutes. The patient can leave the hospital on the same day.
The way to the heart is through the kidneys
Today, ventricular arrhythmias are treated medically or surgically through elective open-heart surgery. For example, when performing coronary artery bypass surgery, the post-infarction scar that causes arrhythmia is also removed. When using a minimally invasive radiofrequency ablation method
A special catheter is inserted into the left ventricle, using special imaging systems, areas causing arrhythmias are identified and destroyed by applying high-frequency electric current.
However, 10–20% of patients suffering from ventricular arrhythmias are not helped by any currently known treatment methods. The fact is that a scar on the heart can have a very complex structure, and then even the most advanced medical navigation system, which determines the internal contour of the heart with millimeter accuracy, cannot accurately indicate the pathological zone.
Since the 1990s. such patients are implanted under the skin in the upper part of the chest with a special electronic device - a cardioverter-defibrillator
, connected to a system of electrodes in contact with the heart. This emergency “watchman” for arrhythmia not only monitors the rhythm of contractions, but also generates life-saving shock electrical discharges in the event of an arrhythmia. But this method does not relieve a person from the disease, but only prevents its fatal consequences. In addition, frequent electrical impulses make the heart muscle flabby, hastening the development of heart failure.
Nevertheless, a way out of this seemingly dead-end situation was found. renal denervation, began to be introduced into clinical practice.
, proposed by M. Levin and D. Gelfand in 2003. And a few years later, the first publication on clinical renal denervation was published (Krum
et al.
, 2009).
The essence of this method is to interrupt the conduction of nerve impulses along the fibers of the autonomic nervous system, which pass not to the heart, but directly to the kidneys. Located in close proximity to the renal arteries, the nerves form the so-called perivascular plexuses
. During the renal denervation procedure, a special balloon is inserted into each renal artery through a puncture in the femoral artery, on the surface of which there are electrodes that block the lumen of the vessels. A series of radiofrequency electrical pulses with a power of 0.5–1.0 W is applied to the electrodes for 30 s. The temperature in this place rises to 70 °C, and this thermal effect blocks the conduction of nerve impulses along the nerve fibers passing along the upper vascular walls.
This method was first used to treat patients with arterial hypertension. Experiments have shown that interrupting the nerve impulses of the autonomic nervous system coming from the kidneys, signaling the brain about increased vascular tone and an increase in blood pressure, leads to a decrease in the latter. Left without feedback from the higher brain center, the kidneys begin to “think” that the pressure is actually normal. As a result, the parameters of the renin-angiotensin-aldosterone system
– a set of enzymes and hormones involved in the regulation of water and electrolyte balance.
Ultimately, the brain begins to receive signals that everything is fine with the pressure, and it, in turn, “agrees.” In essence, the result is achieved by interrupting the pathological feedback, in which the kidneys and the brain mutually “spur” each other with information that “everything is bad.”
Rules for preparing for RFD
Obtaining positive dynamics largely depends on a complete preoperative examination, which includes:
- X-rays of light.
- neurologist's report;
- MRI;
- general blood and urine test, blood test for RW, hepatitis, HIV;
- ECG.
Radiofrequency denervation of joints requires the following precautions:
- some restrictions on food intake - you can’t eat for eight hours before the procedure and drink for two;
- when using insulin, the dose administered on the day of the procedure should be adjusted;
- the decision to stop taking medications is made by a specialist;
- there is a need to refrain from driving vehicles for 12 hours after the procedure.
Pain in the spine is an important socially significant problem in medicine. The prevalence of vertebrogenic pain is about 15% among the adult population.
Vitaly Boyarchik, neurosurgeon, Republican Scientific and Practical Center of Neurology and Neurosurgery A common cause of chronic pain in the cervical and lumbar spine is the pathology of the facet joints - up to 40% of cervicalgia and lumbodynia without the manifestation of radiculopathy.
In the scientific literature you can find many names characterizing this pathology: facet syndrome, facet syndrome, arthrosis of the intervertebral joints, arthrosis of the facet joints, spondyloarthropathic syndrome. Despite the fact that in the international classification of diseases facet syndrome does not have its own code and is coded as “other dorsopathies” (M53.8), a huge number of publications and studies confirm the relevance of this problem. In the United States, denervation of intervertebral joints is the second most frequently performed procedure among all procedures in clinics treating chronic pain.
Pathophysiology
The facet joint is a true synovial joint that contains a separate joint space capable of holding 1 to 1.5 ml of fluid, a synovial membrane, hyaline cartilage surfaces, and a fibrous capsule. Each facet joint receives dual innervation from medial branches arising from the posterior primary rami at the same level and one level above (Luschka nerves). The joint capsules contain mechanoreceptors and nociceptors that quickly respond to mechanical and chemical stimulation. They cause pain and reflex responses of striated and smooth muscles.
The basic anatomical unit of the spine, often called the triarticular complex, consists of paired facet joints and an intervertebral disc. Together, these joints support and stabilize the spine and prevent injury by limiting movement in all planes. Changes in any component of this complex lead to predictable changes in other components. It has been shown that degeneration and loss of structural integrity of the intervertebral discs is accompanied by concomitant degenerative changes in the facet joints.
In young people, the facet joints are quite strong and can support almost twice the body weight. As we age, the joints become weaker and biplanar, moving from a predominantly coronal orientation to a more prominent sagittal position. The load on the facet joints normally in a standing position in the lumbar region is approximately 16% of the total load on the spine. In a sitting position, the load is reduced to zero.
When discs are damaged, the main weight load gradually shifts to the intervertebral joints, reaching 47–70% over time. Overload leads to changes in them: synovitis with the accumulation of synovial fluid between the facets; degeneration of articular cartilage; stretching of the joint capsule and subluxation in them, which leads to pain from stretching of the joint capsule.
Enlargement of the glenoid sockets may also compress the exiting nerve root in the neural foramen or spinal canal. Continued degeneration due to repeated microtrauma, weight-bearing and rotatory overloads leads to periarticular fibrosis and the formation of subperiosteal osteophytes. Eventually the joints degenerate dramatically and lose almost all cartilage.
With inflammation in the facet joints, inflammatory mediators such as nitric oxide, interleukin 6, and prostaglandin E2 increase. A persistent nociceptive stimulus invariably leads to peripheral sensitization, and if the cause persists, central sensitization may develop.
Clinical picture and diagnosis
The main complaint is back pain, localized paravertebrally, without irradiation far from the affected area. The onset of pain may be associated with rotation; the pain intensifies in static positions. Characterized by stiffness in the morning, pain reduction after exercise and when unloading the spine. The use of support, a sitting position, and slight flexion reduce pain. Patients report gradual worsening over time. Pain is more often localized in the lumbar spine, 4 times less often in the cervical spine and 10 times less often in the thoracic spine.
Neuroimaging. The leading methods in this case are CT and MRI. The sensitivity and specificity of the studies reaches 80–90%. Tomography allows for differential diagnosis with other diseases of the spine. Radiography can be used as a screening diagnostic method due to its lower sensitivity and specificity.
Diagnostic blockade. Intra-articular and periarticular blocks are equally effective for diagnosing facet syndrome.
In order to increase sensitivity and reduce the number of false-positive results, the following recommendations must be followed: placebo control; injection of the drug into the lowest point on the transverse process of the vertebra, the injection volume should be no more than 0.5 ml; Subcutaneous and intramuscular injection of anesthetic must be avoided; use only single-needle injection; resort to CT navigation when introducing drugs into the facet joint; Do not use sedation or systemic opioids during the procedure.
A positive response occurs when the patient experiences pain relief that lasts at least as long as the anesthetic. In doubtful cases, it is possible to carry out a repeated diagnostic blockade with an anesthetic, the duration of action of which differs from the drug used in the first blockade.
Carrying out a diagnostic blockade also has a prognostic function for determining indications for surgical treatment and assessing the likelihood of success of denervation of the facet joints.
Treatment options
Conservative therapy for facet syndrome involves the combined use of medicinal and non-medicinal treatment methods.
It has been proven that moderate physical activity associated with everyday household activities helps reduce the intensity of pain in facet syndrome. It is recommended to avoid static and heavy physical activity. Physical therapy exercises can contribute to the speedy rehabilitation of patients with chronic back pain. The increase in load intensity should be gradual, under the supervision of a specialist. The guideline for limiting the force of the load is the intensity of the pain syndrome.
Therapeutic massage has a short-term analgesic effect. Manual therapy is more effective when performing the procedure at the thoracic and cervical levels compared to the lumbar spine. Performing manual therapy is contraindicated in the presence of instability of spinal segments or degenerative changes in the intervertebral discs.
Acupuncture, kinesiotherapy, cognitive-behavioral and other types of psychotherapeutic techniques have a moderate short-term analgesic effect.
For drug therapy of spondyloarthrosis with pain, the following groups of drugs are used: non-narcotic analgesics, including non-steroidal anti-inflammatory drugs; glucocorticoids; antiepileptic drugs used to relieve neuropathic pain; muscle relaxants; antidepressants; B vitamins; correctors of bone and cartilage tissue metabolism; neuroprotective drugs. Prescribing opioid analgesics has a short-term, up to 3 months, positive effect. There is no evidence that opioids are effective over long-term use. In general, drug therapy is identical to the treatment of nonspecific back pain. It should be remembered that long-term use of non-steroidal anti-inflammatory drugs is associated with a high risk of side effects, especially in older people.
Interventional treatment methods include intra-articular and periarticular blockades with anesthetics and glucocorticoids. The evidence of the effectiveness of intra-articular administration of glucocorticoids for facet syndrome is low, as is that of hyaluronic acid preparations. Most researchers prefer periarticular blocks, with up to 80% of patients reporting sustained improvement over an average of 2 to 3 months.
Denervation of the facet joints
The main method of surgical treatment of facet syndrome is radiofrequency denervation (RFD) of the facet joints. A synonym for RFD is the term “high-frequency selective neurotomy.” To denervate each joint, the medial branches of the posterior branches of the same and overlying spinal nerves are coagulated. With this type of denervation, a high-frequency current passing through the non-insulated section of the electrode, due to the resistance of the surrounding soft tissues, heats and damages them, causing coagulation of the nerve and its endings involved in the pathological process.
Controlled limited thermal destruction with specified time and temperature parameters allows you to interrupt the nociceptive pathway. After RFD of peripheral nerves in pain syndromes, no terminal neuroma is formed, and the risk of worsening pain and developing neuropathy is minimal. It should be noted that RFD does not affect the condition of the facet joints, but only has a symptomatic effect, leading to pain regression. Moreover, the effect is longer and more stable than with drug blockades. It has been proven that RFD of the facet joints has a more pronounced analgesic effect compared to pulsed radiofrequency ablation, which does not cause damage to the nervous tissue.
Increasing the effectiveness of RFD of facet joints can be done in two ways: improving the quality of patient selection and optimizing the denervation procedure itself. In the first case, differential diagnosis should be carefully performed, since if the pain is discogenic, denervation of the facet joints will be ineffective. In addition, it is necessary to exclude a somatoform pain disorder, when any intervention manipulations will not lead to improvement.
In the second case, the result depends on the experience of the specialist and the technique of the intervention performed. To increase efficiency, it is recommended to use a wide electrode, which will increase the area of destruction; install the electrode parallel to the nerve; conduct electrophysiological monitoring; carry out destruction at two points - along the upper and lower edges of the joint; administer a local anesthetic with a glucocorticoid after the procedure to prevent nerve degeneration and increase inflammatory changes in the postoperative period.
Analysis of the results of RFD of facet joints in the Republican Scientific and Practical Center of Neurology and Neurosurgery
Materials and methods
From 2021 to 2021, the Republican Scientific and Practical Center of Neurology and Neurosurgery performed neurosurgical treatment of facet syndrome in 12 patients (5 men and 7 women) aged from 43 to 78 years. All patients complained of moderate pain in the lumbar spine without radiation to the lower extremities, lasting more than 6 months. Two patients (16.7%) had previously undergone surgical interventions on the lumbar spine - microdiscectomy.
Conservative treatment was performed in all patients without a significant positive effect. One patient took tramadol at a dosage of 50 mg 2 times a day. For the purpose of differential diagnosis, all patients underwent MRI and functional radiography of the lumbar spine (in flexion and extension). No pathology of the intervertebral discs, instability of segments in the lumbar spine, or other disorders requiring surgical intervention were identified.
All patients underwent diagnostic blockade of the facet joints with local anesthetic (lidocaine) on both sides at the level of pain and at adjacent levels. Patients noted a decrease in pain by more than 50% lasting more than one hour, which was regarded as a positive result of the diagnostic blockade.
RFD of the facet joints was performed at the levels of the performed blocks. After infiltrative anesthesia of the skin with local anesthetic, the skin was punctured paravertebrally with insulated needles. The bare ends of the needles were brought to the facet joints under X-ray control (two for each level).
Then, intraoperative CT control was performed with three-dimensional reconstruction and correction of the position of the needles relative to the expected location of the Luschka nerves. Next, an electrode was inserted into the cannula and electrophysiological testing was performed to exclude effects on the motor part of the nerve. After testing, 0.5 mL of local anesthetic was injected through the needle for analgesia, followed by RFD at 80°C and exposure time of 80 seconds. The manipulation was carried out at the level of pain and at adjacent levels above and below on both sides.
Results and discussion
All patients noted a decrease in pain the next day after surgery, of which 83.3% (10 people) noted a decrease of more than 50% when assessed by VAS. At the follow-up examination after 6 months, no recurrence of the pain syndrome was detected. Our result is comparable to the data of foreign studies (67–77%). Despite the small group of patients in our study, taking into account the strict approach to their selection at the diagnostic stage, we attribute success to the use of intraoperative CT control, which can significantly improve the accuracy of electrode positioning before denervation. As the number of RFDs increases, it will be possible to determine correlations between positive outcome and the use of intraoperative CT.
We found no effect from RFD in 2 patients (16.7%). The pain syndrome decreased, but they remained dissatisfied with the result of the treatment. These are patients who have previously undergone spinal surgery. Foreign researchers also note the low frequency of positive results of RFD of the facet joints in patients with operated spine syndrome.
One of these patients underwent repeated denervation a month later, but no reduction in pain was achieved. The second patient noted a change in the nature of pain in the postoperative period and its displacement towards the sacroiliac joint on the right. After successful completion of the diagnostic blockade, it was decided to perform RFD of the sacroiliac joint under CT control. The patient noted significant improvement. Tramadol was discontinued in the postoperative period. At a follow-up examination after 6 months, the patient did not notice any increase in pain.
There were no complications after RFD in our study, neither in the postoperative nor in the long-term period.
Patient B., 53 years old. Vertebrogenic lumbodynia, persistent severe pain syndrome. Conservative treatment for a long time without effect. After the test blockade, the patient noted an improvement. Radiofrequency denervation of the facet joints was performed at the L3-S1 levels on both sides.
Result: reduction in pain by more than 50%, abolition of painkillers.
conclusions
1. Pathology of the facet joints is a common cause of vertebrogenic chronic pain syndromes. The number of publications addressing this issue is increasing, which confirms the relevance of the issue.
2. A reliable diagnostic criterion for facet syndrome is blockade with local anesthetics. A reduction in false-negative results can be achieved by performing double blockades with different anesthetics.
3. In the absence of effect from conservative therapy and blockades with glucocorticoids, as well as the duration of the pain syndrome for more than 3 months, it is necessary to consider the issue of surgical treatment.
4. The most effective method of neurosurgical treatment of facet syndrome is radiofrequency denervation of the facet joints. This method allows you to achieve a lasting reduction in pain intensity and improve the quality of life with a minimal risk of complications.
5. Criteria for the ineffectiveness of RFD are incorrect selection of patients, as well as violation of intervention technology.
6. The use of intraoperative electrophysiological and CT control can improve the effectiveness of RFD of the facet joints.
Indications for surgery
- Spondyloarthrosis. The most common cause of chest and neck pain is the facet joints. In treatment, injections are ineffective, they act for a short time or give partial results. RFD of the spine in this case is the preferred manipulation, blocking pain for a longer time.
- Discogenic pain. Its spread most often occurs in pathology of the lower spine, when the patient feels severe pain in the affected area, transmitted to the arms and legs. The situation is complicated by limited mobility. The use of RFD in such cases shows effectiveness if surgical intervention is not required.
- If the cause of pain is spinal stenosis, the use of RFD is the most effective and preferred measure.
- Pain in the coccyx area can also be relieved by RFD of the coccygeal nerve.
- Severe constant or paroxysmal headache.
Efficiency of the procedure
The therapeutic effect of the procedure is noticeable immediately, the pain syndrome disappears. The final result can be assessed after one and a half months, since in some cases effectiveness appears only after this period.
The effectiveness of such treatment in various cases can last up to several years. In many cases, the patient needs to engage in physical therapy to restore and develop the joint. If pain relief is not provided, a person will not be able to exercise - the pain will not allow him to move normally. After the procedure, patients begin to exercise, which helps avoid surgery altogether or postpone it for a long time.
If the necessary measures are not taken in a timely manner, pain will become a constant daily test for a person, and there can be no talk of an active lifestyle at all, because even the simplest movements will be difficult.