Registration number
LP-002321
Dosage form
film-coated tablets
Compound
1 film-coated tablet contains:
dosage 0.2 mg g: active substance
: moxonidine 0.2 mg
excipients (core)
: croscarmellose sodium (primellose) - 3.0 mg; lactose monohydrate (lactopress) (milk sugar) -; 95.3 mg; colloidal silicon dioxide (aerosil) -; 0.5 mg; sodium stearyl fumarate -; 1.0 mg;
excipients (shell):
Opadry II (polyvinyl alcohol, partially hydrolyzed -; 1.32 mg; titanium dioxide E 171 -; 0.6027 mg; talc -; 0.6 mg; macrogol (polyethylene glycol 3350) -; 0.3705 mg; soy lecithin E 322 -; 0.105 mg; dye iron oxide (II) yellow -; 0.0003 mg; dye iron oxide (II) red -; 0.0015 mg).
dosage 0.3 mg: active substance
: moxonidine 0.3 mg
excipients (core)
: croscarmellose sodium (primellose);
3.0 mg; lactose monohydrate (lactopress) (milk sugar) -; 95.2 mg; colloidal silicon dioxide (aerosil) -; 0.5 mg; sodium stearyl fumarate; 1.0 mg;
excipients (shell):
Opadry II (polyvinyl alcohol, partially hydrolyzed -; 1.32 mg; titanium dioxide E 171 -; 0.6003 mg; talc -; 0.6 mg; macrogol (polyethylene glycol 3350) -; 0.3705 mg; soy lecithin E 322 -; 0.105 mg; aluminum varnish based on crimson dye [Ponceau 4R] -; 0.0039 mg; aluminum varnish based on sunset yellow dye 0.0003 mg).
dosage 0.4 mg g: active substance
: moxonidine 0.4 mg
excipients (core)
: croscarmellose sodium (primellose) -;
3.0 mg;
lactose monohydrate (lactopress) (milk sugar) -; 95.1 mg; colloidal silicon dioxide (aerosil) -; 0.5 mg; sodium stearyl fumarate -; 1.0 mg; excipients (shell):
Opadry II (polyvinyl alcohol, partially hydrolyzed -; 1.32 mg; titanium dioxide E 171 -; 0.5751 mg; talc -; 0.6 mg; macrogol (polyethylene glycol 3350) -; 0.3705 mg; soy lecithin E 322 -; 0.105 mg; aluminum varnish based on indigo carmine -; 0.0018 mg; aluminum varnish based on azorubine dye -; 0.0153 mg; aluminum varnish based on crimson dye [Ponceau 4R] -; 0. 0123 mg).
Description
Light pink, film-coated tablets, round, biconvex. Tablets with a break are white or almost white in color (dosage 0.2 mg). Tablets, film-coated, pink, round, biconvex. Tablets with a break are white or almost white (dosage 0.3 mg). Tablets, film-coated, dark pink, round, biconvex. Tablets with a break are white or almost white (dosage 0.4 mg).
ATX code
[C02AC05]
Pharmacological properties
Composition and release form
The drug is sold in pharmacies in the form of small tablets for oral administration. Externally, they are white in color with a soluble thin shell. Packaged in blisters of 14 pieces and secondary cardboard packaging. One pack contains 1-2 cells of 14-28 tablets and includes instructions for use.
The active component of the drug is moxonidine. Its amount in 1 tablet is 200 mcg.
Additional substances: castor oil, cellulose, magnesium stearate, Tween 80, Klucel and Aerosil.
pharmachologic effect
The drug belongs to the group of antihypertensive drugs. It is a direct agonist of imidazoline receptors. When used once, it helps to simultaneously restore the level of diastolic and systolic pressure. At the same time, it does not change the activity of the heart and does not affect the heart rate.
The drug is highly digestible, regardless of the time of meal. The biological availability of the drug is at least 88%. The highest concentration of the drug in the red channel is observed after 30 minutes or a maximum of 3 hours.
Pharmacokinetics
Van suctions:
After oral administration, moxonidine is rapidly and almost completely absorbed into the
upper parts of the gastrointestinal tract. Absolute bioavailability is approximately 88%. Time to reach maximum concentration -; about 1 hour. Food intake does not affect the pharmacokinetics of the drug.
Distribution
The connection with blood plasma proteins is 7.2%.
Metabol Meas.
The main metabolite is; dehydrogenated moxonidine. Pharmacodynamic activity of dehydrogenated moxonidine -; about 10% compared to moxonidine.
Output
The half-life (T1/2) of moxonidine and metabolite is 2.5 and 5 hours, respectively. Within 24 hours, over 90% of moxonidine is excreted by the kidneys (about 78
% unchanged and 13% in the form of dehydri-romoxonidine, other metabolites in the urine do not exceed 8% of the dose taken). Less than 1% of the dose is excreted through the intestines.
Pharmacokinetics in patients with arterial hypertension:
Compared with healthy volunteers, patients with arterial hypertension show no changes in the pharmacokinetics of moxonidine.
Farmak okin etika in old age
Clinically insignificant changes in the pharmacokinetic parameters of moxonidine were noted in elderly patients, probably due to a decrease in the intensity of its metabolism and/or slightly higher bioavailability.
Farmak okinetics in children
Moxonidine is not recommended for use in patients under 18 years of age, and therefore pharmacokinetic studies have not been conducted in this group.
Pharmacokinetics for renal failure
Moxonidine excretion is significantly correlated with creatinine clearance (CC). In patients with moderate renal failure (creatinine clearance in the range of 30-60 ml/min), steady-state plasma concentrations and final T1/2 are approximately 2 and l.5 times higher than in patients with normal renal function (creatinine clearance more than 90 ml/min). min.).
In patients with severe renal failure (creatinine clearance less than 30 ml/min.), steady-state plasma concentrations and final T1/2 are 3 times higher than in patients with normal renal function. The administration of multiple doses of moxonidine leads to predictable accumulation in the body of patients with moderate and severe renal failure. In patients with end-stage renal failure (creatinine clearance less than 10 ml/min) on hemodialysis, steady-state plasma concentrations and final T1/2 are 6 and 4 times higher, respectively, than in patients with normal renal function. In all groups, the maximum concentration of moxonidine in blood plasma was 1.5 - 2 times higher. U
For patients with impaired renal function, the dosage should be adjusted individually. Moxonidine is excreted to a small extent during hemodialysis.
Indications for use
Arterial hypertension.
Contraindications
- hypersensitivity to the active substance and other components of the drug;
— sick sinus syndrome;
— severe bradycardia (resting heart rate less than 50 beats/min);
— atrioventricular block II and III degrees;
- severe heart rhythm disturbances;
— acute and chronic heart failure (III-IV functional class according to the NYHA classification);
- simultaneous use with tricyclic antidepressants (see section
“Interaction with other drugs”);
- severe renal failure (creatinine clearance less than 30 ml/min);
- hemodialysis;
- lactation period;
- hereditary lactose intolerance, lactase deficiency or glucose-galactose malabsorption;
— age over 75 years;
- age under 18 years (due to the lack of data on safety and effectiveness).
Particular caution should be exercised when using moxonidine in patients with
atrioventricular block of the first degree (risk of developing bradycardia); severe coronary artery disease, severe coronary heart disease or unstable angina (insufficient experience), chronic heart failure, severe liver failure, with impaired renal function (creatinine clearance more than 30 ml/min).
Pregnancy
There are no clinical data on the use of Moxonidine in pregnant women.
In animal studies, the embryotoxic effect of the drug was established. Moxonidine should be prescribed to pregnant women only after a careful assessment of the risk-benefit ratio, when the benefit to the mother outweighs the potential risk to the fetus.
Lactation period
Moxonidine passes into breast milk and should therefore not be given during breastfeeding. If it is necessary to use Moxonidine during lactation, breastfeeding should be stopped.
Directions for use and doses
Inside, regardless of food intake. In most cases, the initial dose of the drug
Moxonidine is 0.2 mg per day. The maximum single dose is 0.4 mg. The maximum daily dose, which should be divided into 2 doses, is 0.6 mg. Individual adjustment of the daily dose is necessary depending on the patient’s tolerance to the therapy. No dose adjustment is required for patients with hepatic impairment. The starting dose for patients with moderate or severe renal impairment is 0.2 mg/day. If necessary and if well tolerated, the daily dose can be increased to a maximum of 0.4 mg.
Side effect
The frequency of side effects listed below was determined accordingly
the following: very often (>1/10); often (>1/100, <1/10); uncommon (>1/1000, <1/100); including individual messages.
From the central nervous system:
Common: headache*, dizziness (vertigo), drowsiness. Uncommon: fainting*.
From the cardiovascular system:
Uncommon: marked decrease in blood pressure, orthostatic hypotension*, bradycardia.
From the gastrointestinal tract:
Very common: dry mouth. Common: diarrhea, nausea, vomiting, dyspepsia.
From the skin and subcutaneous tissues: Often: skin rash, itching.
Uncommon: angioedema.
Mental disorders:
Common: insomnia. Uncommon: nervousness.
Hearing and labyrinthine disorders: Uncommon: ringing in the ears.
Musculoskeletal and connective tissue disorders: Common: back pain.
Uncommon: neck pain.
General disorders and disorders at the injection site:
Often: asthenia.
Uncommon: peripheral edema.
(* - frequency comparable to placebo).
Overdose
There have been several reports of non-fatal overdoses when
Doses up to 19.6 mg were used simultaneously.
Symptoms:
headache, sedation, marked decrease in blood pressure, dizziness, asthenia, bradycardia, dry oral mucosa, vomiting, fatigue, pain in the epigastric region, respiratory depression and impaired consciousness. In addition, short-term increases in blood pressure, tachycardia and hyperglycemia are also possible, as shown in several high-dose animal studies.
Treatment
There is no specific antidote. In the case of a pronounced decrease in blood pressure, it may be necessary to restore the volume of circulating blood by introducing fluid and dopamine (injection).
Bradycardia can be stopped with atropine (injection).
In severe cases of overdose, it is recommended to carefully monitor disturbances of consciousness and avoid respiratory depression.
Alpha-adrenergic antagonists may reduce or eliminate the paradoxical hypertensive effects of moxonidine overdose.
Moxonidine is excreted to a small extent during hemodialysis.
Interaction with other drugs
The combined use of moxonidine with other antihypertensive drugs leads to an additive effect. Tricyclic antidepressants may reduce the effectiveness of centrally acting antihypertensive drugs, and therefore their use together with moxonidine is not recommended.
Moxonidine may enhance the effect of tricyclic antidepressants, tranquilizers, ethanol, sedatives and hypnotics.
Moxonidine may moderately improve impaired cognitive function in patients receiving lorazepam.
Moxonidine may enhance the sedative effect of benzodiazepine derivatives when administered simultaneously.
Moxonidine is released by tubular secretion. Therefore, its interaction with other drugs released by tubular secretion is not excluded. Beta-blockers increase bradycardia and the severity of negative ino- and dromotropic effects.
special instructions
If it is necessary to cancel beta-blockers and the drug Moxonidine taken simultaneously, first cancel the beta-blockers and only after a few days Moxonidine.
There is currently no evidence that stopping Moxonidine leads to an increase in blood pressure. However, it is not recommended to stop taking Moxonidine suddenly; instead, you should gradually reduce the dose of the drug over two weeks.
Avoid drinking alcohol during treatment.
During treatment, regular monitoring of heart rate and electrocardiography is necessary.
Impact on the ability to drive vehicles and operate machinery
The effect of Moxonidine on the ability to drive vehicles or operate machinery has not been studied. However, taking into account the possibility of dizziness and drowsiness, patients should be careful when engaging in potentially hazardous activities that require increased attention, such as driving a vehicle or operating equipment that requires increased concentration.
Release form
Film-coated tablets, 0.2 mg, 0.3 mg and 0.4 mg
10, 14 or 30 tablets per blister pack.
60 tablets in polymer jars or polymer bottles.
Each jar, bottle, 3 blister packs of 10 tablets, 1 or 2 blister packs of 14 tablets each, or 1 or 2 blister packs of 30 tablets, together with instructions for use, are placed in a cardboard box.
Best before date
3 years. Do not use after the expiration date stated on the packaging.
Storage conditions
In a dry place, protected from light, at a temperature not exceeding 25 C.
Keep out of the reach of children.
Vacation conditions
On prescription
Contraindications
It is prohibited to take the medicine for the following conditions:
- Individual intolerance to the active or auxiliary components.
- Acute form of bradycardia.
- Severe arrhythmia.
- Glaucoma.
- Mental disorders.
- Cardiac failure.
- Previous Quincke's edema.
- The period of bearing a child and breastfeeding.
- Children under 18 years of age.
- Disturbance of the liver and kidneys.
- Angina pectoris.
- Lactose deficiency or intolerance.
- Various pathologies of the circulatory system.
Side effects
As a result of treatment with Moxonidine, patients may experience the following adverse reactions:
- High fatigue, malaise.
- Migraine.
- Sleep disorder - insomnia or drowsiness.
- Dizziness, headache.
- Dyspeptic manifestations - dry mouth, discomfort in the epigastrium, nausea, vomiting, abnormal stool.
- Increased nervousness and irritability.
- Swelling of peripheral tissues.
- A sharp decrease in pulse and blood pressure.
- Allergic signs are skin rash and severe itching.
Centrally acting drug moxonidine in the treatment of arterial hypertension
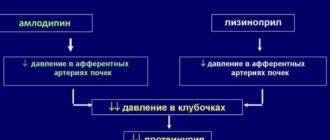
According to epidemiological studies, the prevalence of arterial hypertension (AH) among adults in developed countries ranges from 20% to 40% and increases with age [3]. Elevated blood pressure is found in more than 50% of men and women over 60 years of age [4]. The relevance of the problem is supported by the increasing processes of urbanization of society, which create the preconditions for the emergence of risk factors such as stress, physical inactivity, obesity, bad habits and disturbed ecology. High blood pressure is one of the main risk factors for the development of cerebral stroke, coronary heart disease (CHD) and other cardiovascular diseases of atherosclerotic origin, which are associated with more than 50% of all deaths [5]. According to modern national recommendations [6], recommendations of the European Society of Arterial Hypertension and the European Society of Cardiology [7], the treatment tactics for essential hypertension depend on the level of blood pressure and the degree of risk of cardiovascular complications. The main goal of treatment is to minimize the risk of developing cardiovascular complications and death from them. The main objectives are normalization of blood pressure levels in order to prevent complications in the absence or minimal level of adverse drug reactions, correction of all modifiable risk factors (smoking, dyslipidemia, hyperglycemia, obesity), prevention, slowing down the rate of progression and/or reducing target organ damage, as well as treatment of associated and concomitant diseases - ischemic heart disease, diabetes mellitus (DM), etc. [6, 7]. When treating patients with hypertension, blood pressure should be less than 140/90 mm Hg. Art., which is its target level. If the prescribed therapy is well tolerated, it is advisable to reduce blood pressure to lower values. In patients with a high and very high risk of cardiovascular complications, it is necessary to reduce blood pressure to 140/90 mmHg. Art. or less within 4 weeks. In the future, subject to good tolerance, it is recommended to reduce blood pressure to 130/80 mmHg. Art. and less. In patients with coronary artery disease, blood pressure should be reduced to the target value of 130/85 mm Hg. Art. In patients with diabetes and/or kidney disease, the target blood pressure level should be less than 130/85 mmHg. Art. [6]. There are no uniform recommendations regarding which drugs should be used to start treating a patient. The choice of drug depends on many factors, including age, gender and the presence of concomitant diseases. Currently, 5 main classes of antihypertensive drugs are recommended for the treatment of hypertension: angiotensin-converting enzyme inhibitors (ACEIs), AT1 receptor blockers (ARBs), calcium antagonists (CAs), β-blockers (BABs), and diuretics. α-blockers, imidazoline I1 receptor agonists, and direct renin inhibitors can be used as additional classes for combination antihypertensive therapy [6, 7].
Agonists of imidazoline receptors (moxonidine, rilmenidine) are modern drugs with a central mechanism of action - they reduce the activity of the vasomotor center of the medulla oblongata. Centrally acting antihypertensive drugs also include clonidine, guanfacine, and methyldopa [1, 2]. Moxonidine (Moxarel, JSC "Vertex", Russia) is a highly selective agonist of imidazoline I1 receptors located in the rostral ventrolateral part of the medulla oblongata. Stimulation of these receptors reduces sympathetic flow and, accordingly, blood pressure by reducing vascular resistance. In addition, the activity of the vasomotor center decreases, cardiac output and peripheral sympathetic activity decrease. Taking moxonidine leads to a decrease in systemic vascular resistance and blood pressure. Moxonidine reduces the levels of renin, angiotensin II and aldosterone in the blood plasma [20]. After oral administration, the peak concentration is reached within 1 hour. The half-life in plasma is 2 hours and increases with renal failure. Despite the relatively short half-life, blood pressure is effectively regulated with a single dose of the drug per day. The antihypertensive effect lasts much longer, which is due to the retention of the drug in the central nervous system. The sympathoinhibitory effect of moxonidine is probably mediated almost entirely by its effect on I receptors. Moxonidine differs from other sympatholytic antihypertensive drugs in its lower affinity for central α2-adrenergic receptors, which explains the lower likelihood of developing sedation and dry mouth compared to clonidine. The antihypertensive effectiveness of moxonidine in essential hypertension has been proven in large-scale, double-blind, placebo-controlled, randomized studies and is comparable to that of most other antihypertensive drugs [8].
Food intake does not affect the pharmacokinetics of the drug. The drug is well absorbed from the gastrointestinal tract and is almost completely absorbed in its upper sections. Absolute bioavailability is approximately 88%. The maximum concentration in the blood is recorded after 0.5–3 hours. The connection with blood plasma proteins is 7.2%. 90% of the drug is excreted by the kidneys, mainly (70%) unchanged. The half-life (T1/2) of moxonidine and metabolite is 2.5 and 5 hours, respectively. Despite its short half-life (about 3 hours), it controls blood pressure throughout the day [9]. Moxonidine is effective in monotherapy for hypertension, but it is optimal to prescribe it as part of combination therapy, for example, with ACE inhibitors, sartans (ARBs), thiazide diuretics and other main antihypertensive drugs. The combination of moxonidine with other antihypertensive drugs enhances their antihypertensive effect. Moxonidine, when added to therapy with an ARB II (eprosartan), normalizes blood pressure and sympathetic hyperactivity in hypertensive normovolemic patients with chronic renal failure. In terms of antihypertensive effectiveness, moxonidine is not inferior to diuretics, beta blockers, AK and ACE inhibitors, and in terms of tolerability it is significantly superior to previous centrally acting drugs. It is safer than clonidine, propranolol, captopril, nifedipine. Moxonidine improves the insulin sensitivity index by 21% (compared to placebo) in patients with obesity, insulin resistance and moderate hypertension. The sedative effect is significantly less pronounced than that of other centrally acting drugs. The drug potentiates the effects of central nervous system depressants - ethanol, tranquilizers, barbiturates. Moxonidine may moderately improve impaired cognitive function in patients receiving lorazepam. Prescribing moxonidine together with benzodiazepines may be accompanied by an increase in the sedative effect of the latter [1, 6, 8–10, 13–19].
The TOPIC (Trial Of Physiotens In Combination) study, conducted in the UK at 138 clinical sites, included 566 patients with hypertension aged 18–80 years. When prescribing moxonidine at a dose of 0.2 or 0.4 mg/day, reliable control with monotherapy was achieved in 294 (52%) patients, in the rest - with combination therapy (in combination with amlodipine or enalapril). During the study, the drug proved to be effective and well tolerated both in monotherapy and combination therapy [10, 11]. When using moxonidine in patients with hypertension, a dual mechanism of action is observed - the drug provides both short-term (mainly due to its effect on the sympathetic centers of the brain) and long-term (by suppressing the release of renin and improving excretory function of the kidneys) blood pressure control. Thus, a single oral dose of moxonidine (0.4 mg) caused a statistically significant decrease in blood pressure in patients with hypertension from an average of 176/105 mm Hg. Art. up to 158/95 mm Hg. Art. [10, 11].
For the treatment of patients with mild and moderate hypertension, the recommended initial dose of Moxarel (moxonidine) is 0.2 mg/day. If the response to treatment is unsatisfactory, after 2 weeks. the dose is doubled. A dose of 0.2–0.4 mg/day in most cases was sufficient to maintain blood pressure at a satisfactory level. The high antihypertensive efficacy of moxonidine has been confirmed in the treatment of patients with uncomplicated hypertensive crisis. Thus, with sublingual administration of moxonidine at a dose of 0.4 mg, an effective reduction in blood pressure with good tolerability of the drug was achieved in 90% of patients. A significant decrease in systolic blood pressure and diastolic blood pressure after a single dose of the drug is observed after 20 minutes and reaches a maximum after 1.5 hours [1, 2, 10, 12]. Moxarel (moxonidine) occupies a special place in the treatment of hypertension combined with obesity. By activating imidazoline I1 receptors, it helps reduce fat hydrolysis, reduce free fatty acids, increase glucose metabolism and increase insulin sensitivity, reduce triglyceride levels, increase high-density lipoproteins and reduce plasminogen activator inhibitor-1 levels. Studies have provided evidence of the effect of moxonidine on reducing insulin resistance in overweight patients with impaired glucose tolerance. Thus, in the comparative study ALMAZ, the effect of moxonidine and metformin on glycemic control in patients with overweight, mild hypertension, insulin resistance and impaired glucose tolerance was assessed. The criteria for inclusion of patients in the study were: age over 40 years, body mass index (BMI) >27 kg/m2, fasting glucose >6.1 mmol/l. The ALMAZ study showed that moxonidine lowered fasting glucose levels, reduced patients' weight, increased the rate of glucose utilization, and reduced insulin resistance. With moxonidine, fasting glucose levels decreased less pronounced than with metformin, but insulin levels significantly decreased, while metformin had no effect on it, and BMI decreased equally with both drugs. Both drugs statistically significantly increase insulin sensitivity after a glucose load. Moxonidine affects the level of insulin in the blood, metformin regulates glucose levels, which is accompanied by a decrease in glycosylated hemoglobin. Both drugs statistically significantly reduce body weight while remaining metabolically neutral to lipids [21–26].
Long-term therapy with moxonidine in elderly patients with hypertension of 1-2 degrees provides an optimal reduction in blood pressure during the day and at night with good tolerability of the drug (low frequency and insignificant severity of side effects), leads to a significant reduction in left ventricular hypertrophy, and a decrease in the left ventricular myocardial mass index. Monotherapy with moxonidine for 24 weeks. has a positive effect on cognitive functions (memory and thinking), which indicates improved functioning of the frontal lobes of the brain. In the field of intellectual activity, positive dynamics were observed - the ability of patients to perform actions that require a higher level of generalization in the visual-figurative and visual-logical spheres increased. In addition, during the treatment, positive changes in memory were revealed - the productivity of memorization increased [27]. For patients with metabolic syndrome, it is also important to note the nephroprotective effect of moxonidine. Long-term use of moxonidine causes a significant decrease in microalbuminuria, concentrations of free thrombomodulin and plasminogen activator inhibitor in the blood. According to the results of a post-marketing review study, moxonidine effectively reduces blood pressure in patients with metabolic syndrome and at the same time promotes weight loss in obese patients. After 8 weeks treatment, patients recorded a decrease in body weight by an average of 1.4 kg, with the most pronounced decrease observed in obese patients. The frequency of use of combination antihypertensive therapy was 81.1% among patients with metabolic syndrome and 63.3% in the group as a whole. There was a significant decrease in systolic (26.9±15.1 mmHg, 95% CI 26.4–27.3) and diastolic (13.2±9.5 mmHg, 95% CI 12 ,9–13.5) BP. High efficacy of moxonidine (diastolic blood pressure reduction to <90 mm Hg and/or diastolic blood pressure reduction >10 mm Hg) was reported in 94% of patients. Similarly, a positive effect was observed in a large number of patients with metabolic syndrome - 94%, obesity - 93%, diabetes - 94% and those receiving monotherapy - 95% [28–31].
Conclusions. Moxarel (moxonidine) is the drug of choice among antihypertensive drugs with a central mechanism of action and is characterized by high antihypertensive efficacy and tolerability in patients with overweight, obesity, metabolic syndrome or without it, and also has additional metabolic properties and has a beneficial effect on body weight. Moxonidine is well tolerated, has little interaction with other drugs and can be used once a day in most patients. Moxarel (moxonidine) is indicated for the treatment of patients with mild to moderate hypertension, and especially as an additional drug in the treatment of patients with metabolic syndrome.
Literature 1. Clinical pharmacology and pharmacotherapy / Ed. V.G. Kukesa, A.K. Starodubtseva. M.: GEOTAR-Media, 2012. 832 p. 2. Clinical pharmacology: national guidelines (National Guidelines Series). M.: GEOTAR-Media, 2014. 976 p. 3. Oganov R.G., Timofeeva T.N., Koltunov I.E. and others. Epidemiology of arterial hypertension in Russia. Results of federal monitoring 2003–2010. // Cardiovascular therapy and prevention. 2011. No. 1. P. 9–13. 4. ABC Of Hypertension / Ed. by D. Gareth Beevers, Gregory H. Lip and Eoin O'Brien. 5th ed. Malden, Mass.: BMJ Books, 2007. P. 88. 5. Ezzati M., Lopez AD, Rodgers A. et al. Selected major risk factors and global and regional burden of disease // Lancet. 2002. Vol.360(9343). P.1347–1360. 6. Diagnosis and treatment of arterial hypertension. Recommendations of the Russian Medical Society on arterial hypertension and the All-Russian Scientific Society of Cardiologists. Fourth revision // Systemic hypertension. 2010. No. 3. P. 5–26. 7. ESH-ESC Guidelines Committee. 2013 guidelines for the management of arterial hypertension // J. Hypertens. 2013. Vol. 31. P. 1281–1357. 8. Neumann J., Ligtenberg G., Oey L. et al. Moxonidine normalizes sympathetic hyperactivity in patients with chronic renal failure receiving eprosartan // J. Amer. Soc. Nephrol. 2004. Vol.15. P. 2902–2907. 9. Instructions (TCFS) for the drug Moxarel. 10. Gaponova N.I., Abdrakhmanov V.R., Baratashvili V.L., Tereshchenko S.N. Analysis of the effectiveness and safety of moxonidine in patients with arterial hypertension and hypertensive crises // Practical Medicine. Cardiology. 2011. 04. 11. Waters J., Ashford J., Jager BA et al. Use of moxonidine as unitial therapy and in combination in the treatment of essential hypertension: results of the TOPIC (Trial of Physiotens in Combination) study // J. Clin Basic Cardiol. 1999. Vol. 2. P. 219–224. 12. Ruksin V.V., Grishin O.V. Emergency care for high blood pressure that is not life-threatening // Cardiology. 2011. No. 2. P. 45–51. 13. Frei M., Küster l., Gardosch von Krosigk PP. et al. Moxonidine and hydrochlorothiazide in combination: a synergistic antihypertensive effect // J. Cardiovasc. Pharmacol. 1994. Vol. 24. P. 25–28. 14. Prichard BNC, Simmons R, Rooks MJ et al. A double-blind comparison of moxonidine and atenolol in the management of patients with mild – to moderate hypertension // J. Cardiovasc. Pharmacol.1992. Vol. 20. P. 45–49. 15. Wolf R. The treatment of hypertensive patients with a calcium antagonist or moxonidine: a comparison // J. Cardiovasc. Pharmacol. 1992. Vol. 20. P. 42–44. 16. Lotti G., Gianrossi R. Moxonidin vs. captopril in mild to moderate hypertension (German) // Fortschr. Med. 1993. Vol. 111 (27). P. 429–432. 17. Kraft K., Vetter H. Twenty – four – hour blood pressure profiles in patients with mild – to – moderate hypertension; moxonidine versus captopril // J. Cardiovasc. Pharmacol. 1994. Vol. 24 (Suppl. 1). S. 29–S33. 18. Küppers HE, Jäger BA, Luszick JH et al. Placebo-controlled comparison of the efficacy and tolerability of once – daily moxonidine and enalapril in mild – to moderate essential hypertension // J. Hypertens. 1997. Vol.15. P. 93–97. 19. Prichard BNC, Kuster LJ, Hughes PR et al. Dose relation of blood pressure reduction with moxonidine: findings from three placebo – and active – controlled randomized studies // J. Clin. Basic. Cardiol. 2003. Vol. 6. P. 49–51. 20. Sanjuliani AE, Genelhu de Abreu V., Ueleres Braga J., Francischetti EA Effects of moxonidine on the sympathetic nervous system, blood pressure, plasma renin activity, plasma aldosterone, leptin and metabolic profile in obese hypertensive patients // J. Clin Basic Cardial. 2004. Vol. 7. P. 19–25. 21. Metabolic syndrome. M.: “MEDpres-inform”, 2007. 22. Mkrtumyan A.M., Biryukova E.V. The main approach to pharmacotherapy of metabolic syndrome // Consilium medicum. 2006. T. 8, No. 5. P.54–57. 23. Mychka V.B., Chazova I.E. Metabolic syndrome. Possibilities of diagnosis and treatment. (Prepared on the basis of recommendations of VNOK experts on the diagnosis and treatment of metabolic syndrome), 2008. P. 1–16. 24. Chazova I.E., Almazov V.A., Shlyakhto E.V. Moxonidine improves glycemic control in patients with arterial hypertension and overweight compared with metformin: the ALMAZ study // Diabetes, Obesity and Metabolism. 2006. Vol. 8. P. 456–465. 25. Scarpello JH, Howlett HC Metformin therapy and clinical uses // Diab. Vase. Dis. Res. 2008. Vol. 5. P. 157–167. 26. Shilov A.M., Avshalumov A.Sh., Sinitsina E.N., Eremina I.V. Correction of risk factors in patients with excess body weight combined with insulin resistance and arterial hypertension // Breast Cancer. 2011. T. 19, No. 2. P.1–7. 27. Martynov A.I., Ostroumova O.D., Korsakova N.K. and others. The effect of the drug moxonidine (physiotens) on the state of the cardiovascular system and brain in elderly patients with arterial hypertension // Russian Journal of Cardiology. 2002. No. 4. 28. Hausberg M., Tokmak F., Pavenstadt H. Et al. Effects of moxonidine on sympathetic nerve activity in patients with end-stage renal disease // J. Hypertens. 2010. Jul 14. 29. Krespi PG, Makris TK, Hatzizacharias AN et al. Moxonidine effect on microalbuminuria, thrombomodulin, and plasminogen activator inhibitor-1 levels in patients with essential hypertension // Cardiovasc. Drugs Ther. 1998.Vol.12(5). P. 463–467. 30. Aleksanyan L.A., Polosyants O.B. Moxonidine in the modern treatment of cardiovascular diseases // Breast Cancer. 2010. No. 18. 31. Sharma AM, Wagner T., Marsalek P. Moxonidine in the treatment of overweight and obese patients suffering from metabolic syndrome: results of a post-marketing survey study (CAMUS) // Reviews of Clinical Cardiology. 2007. No. 10.
Drug overdose
If medical recommendations are not followed and the maximum volume of the drug is exceeded, an overdose may develop. The condition is determined by severe symptoms:
- Intense headache and dizziness.
- Nausea followed by vomiting.
- Painful sensations in the stomach area.
- Weakness and severe malaise.
- Extensive reduction in pressure.
- Dryness in the mouth.
If the above symptoms occur, you should definitely consult a doctor. Treatment involves relief of symptoms. Prescribed medication, gastric lavage, parenteral administration of saline. To suppress the symptoms of bradycardia, the use of Atropine is indicated.
special instructions
The use of an antihypertensive drug for therapeutic purposes requires constant monitoring of blood pressure, heart function and heart rate.
During the course of treatment, you should completely avoid alcoholic beverages. It is recommended not to drive vehicles or engage in activities that require concentration, memory and high mental activity.
You need to stop taking the drug gradually, gradually reducing the dose until complete withdrawal.
If the use of Moxonidine was combined with beta-blockers and it is necessary to discontinue both drugs, the latter are removed first. After some time, the antihypertensive drug is discontinued.
Pharmacodynamics
Moxonidine is an antihypertensive drug with a central mechanism of action. In the brainstem structures (rostral layer of the lateral ventricles), moxonidine selectively stimulates imidazoline-sensitive receptors that take part in the tonic and reflex regulation of the sympathetic nervous system. Stimulation of imidazoline receptors reduces peripheral sympathetic activity and blood pressure (BP).
Moxonidine differs from other sympatholytic antihypertensive drugs in its lower affinity for α2-adrenergic receptors, which explains the lower likelihood of developing sedation and dry mouth.
Taking moxonidine leads to a decrease in systemic vascular resistance and blood pressure. Moxonidine improves the insulin sensitivity index by 21% (compared to placebo) in patients with obesity, insulin resistance and moderate hypertension.