Anemia
or
“anemia”
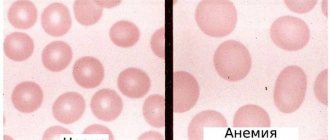
- a decrease in the concentration of hemoglobin in the blood below established standards, most often, with a simultaneous decrease in the total volume of red blood cells (red blood cells that carry oxygen). Anemia, as a secondary symptom, can accompany various diseases, causing the development of oxygen starvation of tissues. The patient experiences chronic fatigue and weakness, constant drowsiness and loss of strength, dizziness and shortness of breath.
Anemia in men and women
Anemia is one of the most common diseases among the adult population of the Earth today. Risk groups for developing anemia include:
- lovers of vegetarian cuisine.
- patients suffering from large blood losses due to the physiological characteristics of the body or a number of chronic diseases.
- pregnant women.
- professional athletes.
Anemia in men is diagnosed in the presence of malignant neoplasms or hidden bleeding of the gastrointestinal tract, peptic ulcer, hemorrhoids and other pathologies. A decrease in the level of hemoglobin in a woman’s blood can be associated with heavy menstruation, pregnancy and lactation, and a period of hormonal changes during menopause. Varying degrees of anemia also appear in children due to lack of adequate nutrition, impaired absorption of iron in the gastrointestinal tract, gastritis or parasitic diseases, limited exposure to fresh air and physical inactivity.
Prerequisites for the emergence
There are several reasons for the development of pathology.
- Rheumatoid arthritis and anemia. What you need to know
- Mature age. Women over 85 years of age are more susceptible to the disease.
- Chronic inflammation, infections and malignant tumors.
- Iron deficiency due to constant blood loss caused by pathologies such as colon cancer or stomach ulcers.
- Heredity.
- Pathological condition of the kidneys.
Principles of classification of anemia
There are several types of classifications of anemia, based on a number of signs - the cause of the disease, the mechanism of its development, stages, symptoms and other parameters. The following groups are distinguished:
Sign up for an anemia screening
Make an appointment
Classification of anemia by severity
The severity of anemia, determined by blood parameters depending on the age and gender of the patient, is conventionally divided into mild, moderate and severe. The mild form is characterized by a decrease in hemoglobin concentration to 90 g/l (the patient may experience general weakness and increased fatigue). The average degree is determined by the range from 70 to 90 g/l (patients complain of shortness of breath, tachycardia, headache, sleep disturbance, tinnitus, loss of appetite), and severe - below the limit of 70 g/l (the main danger of this condition is the development heart failure).
Classification of anemia by color index
The color index determines the level of saturation of red blood cells with hemoglobin. It is calculated during a laboratory blood test using a special formula. Depending on the results obtained, there are:
What is ZhDA
IDA is a condition in which the body is deficient in iron, which causes a decrease in the number of red blood cells. As a result, various disturbances in the functioning of the body develop, primarily associated with inadequate gas exchange. Therefore, iron deficiency anemia is characterized by weakness, dizziness and even loss of consciousness, as well as a number of other changes in the condition. This may be a consequence of both insufficient intake of iron from food, and a violation of its absorption in the body or excessive consumption.
Therefore, iron deficiency anemia cannot be a primary disease. It is always a consequence of the occurrence of certain violations. At the same time, it accounts for about 80% of all anemia, which requires careful attention to this problem and its detailed consideration.
WHO statistics show that more than 2 billion people worldwide suffer from iron deficiency anemia. But this is only according to official data. In reality, their number is significantly higher.
Normally, iron enters the body along with plant and animal foods. In plant sources it is found in the form of ferric iron, and in animal sources - ferrous. These forms of iron differ in different rates and degrees of absorption. Iron from animal food sources, or heme, is easily absorbed. But trivalent or non-heme iron obtained from plant foods must first be transformed under the action of hydrochloric acid of the stomach into divalent, and after entering the initial parts of the small intestine with the food bolus, it must again transform into the trivalent form.
Some of the iron accumulates in the mucous membrane of the small intestine, and the rest is absorbed into the blood. Moreover, no more than 2.5 mg of iron can be absorbed per day. In the blood it is bound by the protein transferrin, the production of which is responsible for the liver. The amount of iron absorbed and deposited in the intestines is regulated depending on its level in the body. If excess iron comes from food, it is retained in a larger volume in the cells of the mucous membrane of the small intestine, which are subsequently naturally exfoliated and excreted along with feces.
Iron absorbed into the bloodstream is transported by transferrin in two main directions:
- through the portal vein it enters the liver, where it is deposited in the form of the protein ferritin;
- is delivered to red bone marrow cells, where it is used for the synthesis of hemoglobin and takes part in tissue redox reactions.
If disturbances occur at any of these stages, the body develops iron deficiency. Thus, with a decrease in the acidity of gastric juice, which may be a consequence of atrophic gastritis, the use of antacids, or gastric resection, the body’s ability to convert ferrous iron into ferric iron decreases. This means that it cannot be fully absorbed and subsequently participate in biochemical transformations.
With the development of chronic pathologies affecting the intestinal mucous membranes, their ability to absorb iron also decreases. Therefore, it cannot enter the blood in sufficient quantities.
If the binding process of iron by transferrin is disrupted, it cannot be transported effectively throughout the body. Therefore, it does not enter the red brain cells in the required quantities.
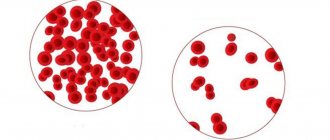
In any of these cases, the consequence is a decrease in the ability to form hemoglobin and other iron-containing proteins, i.e., the development of iron deficiency anemia and other metabolic disorders. As a result of a decrease in hemoglobin production, the resulting young red blood cells are smaller in size, and their total number decreases.
Classification of anemia according to the mechanism of development of the pathological process
The following states are distinguished:
Iron-deficiency anemia
– the name indicates the cause of the pathology. Due to a deficiency of an important microelement, hemoglobin synthesis in the body is disrupted. The supply of oxygen to tissue cells, the stability of redox processes, and the functioning of the immune, nervous and cardiovascular systems depend on the level of iron. Clinical manifestations of iron deficiency anemia are dizziness, fainting, weakness and lethargy, shortness of breath with any exertion, palpitations. Pallor of the skin, brittle nails, thinning hair, and cracks in the corners of the lips are also typical for this disease.
Hemolytic anemia
occurs as a result of the accelerated destruction of erythrocytes (red blood cells) and the rapid accumulation of their breakdown products in the body. The main manifestations are an increased amount of indirect bilirubin in the blood. The patient experiences the development of anemic and icteric syndromes with an enlarged spleen and liver, as well as characteristic staining of feces and urine.
Posthemorrhagic anemia
– hematological changes that appear after acute or prolonged chronic blood loss as a result of external or internal bleeding (trauma, heavy menstruation, hemorrhagic diseases, gastrointestinal and pulmonary bleeding). The main manifestations of posthemorrhagic anemia are palpitations, shortness of breath, severe dizziness, darkening of the eyes, and lethargy. In severe cases - loss of consciousness.
Sideroblastic (sideroachrestic) anemia
occurs as a result of a violation of iron synthesis, causing its deficiency in red blood cells. Due to a failure in the processes of getting this microelement into the hemoglobin molecule, iron in the cells is replaced by sideroblasts (red blood cell precursor cells interspersed with iron in the form of a ring). This condition can be congenital or acquired. Experts believe that the main reason for the development of such anemia is a lack of the substance protoporphyrin. This organic component, combining with iron, turns into heme - part of the hemoglobin molecule. The main symptoms of the disease are disturbances in the functioning of the heart and blood vessels, indigestion, pale skin, dizziness, and memory loss. There is a danger of iron accumulation in various organs, which contributes to the occurrence of serious complications (liver cirrhosis, diabetes mellitus).
B12 deficiency anemia
– a disorder of hematopoiesis as a result of a lack of vitamin B12 in the human body. The main reasons for the development of such anemia are lack of adequate nutrition, impaired absorption of B12 due to inflammatory processes in the gastrointestinal tract, alcoholism, and hereditary predisposition. The pathology develops gradually, causing damage to the digestive organs and disturbances in the functioning of the nervous system.
Publications in the media
Anemia is a decrease in the Hb content per unit volume of blood, often with a simultaneous decrease in the number of red blood cells (or the total volume of red blood cells). The term “anemia” without detail does not define a specific disease, but indicates changes in blood tests, i.e. anemia should be considered one of the symptoms of pathological conditions. Frequency. 157 per 100,000 population in 2001
General signs • Hb content <100 g/l, erythrocyte count <4.0´1012/l, serum iron content <14.3 µmol/l • The isolated existence of one symptom or their combination is possible. For example, thalassemia is not characterized by a decrease in the number of red blood cells.
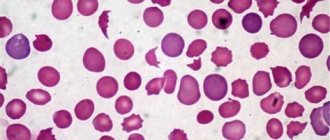
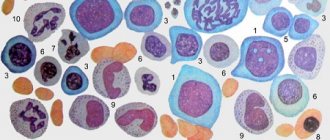
Classification criteria • Based on the morphology of erythrocytes, microcytic, normocytic and macrocytic anemias are distinguished (-cytic indicates the size of erythrocytes). An objective evaluation criterion is the average erythrocyte volume (MEV); normal is 80–94 femtoliters (fl) • Based on the degree of saturation of erythrocytes Hb (or serum iron content), hypochromic, normochromic and hyperchromic anemias are distinguished (-chromic indicates the color of erythrocytes). An objective assessment criterion is the average Hb content in the erythrocyte (ASGE); Normal is 27–33 picogram (pg).
Based on the combination of the first and second criteria, anemia is distinguished: •• Hypochromic microcytic (low SER and SSGE) •• Macrocytic (increased SER) •• Normochromic normocytic (SER and SSGE within normal limits) • Based on the degree of erythrocyte regeneration, anemia is distinguished between hyporegenerative (regenerative) and hyperregenerative. Determined by the number of blood reticulocytes or reticulocyte index • By the degree of hematopoietic effect of erythropoietin. Both the content of erythropoietin and the sensitivity of immature erythroid cells to it are taken into account.
Pathogenetic classification • Anemia due to impaired Hb synthesis and iron metabolism (hypochromic microcytic) •• Iron deficiency anemia (IDA) •• Thalassemia •• Sideroblastic anemia •• Anemia in chronic diseases (60% normochromic normocytic) • Anemia due to impaired DNA synthesis (hyperchromic macrocytic with megaloblastic type of hematopoiesis) •• Pernicious anemia and other B12-deficiency anemias •• Folate deficiency anemia • Other pathogenetic mechanisms (usually normochromic normocytic anemia) •• Anemia combined with a decrease in the bone marrow response to erythropoietin ••• Aplastic anemia • •• Disorders characterized by cellular infiltration of the bone marrow (myelophthisic anemia) ••• Anemia due to erythropoietin deficiency •• Hyperregenerative anemia ••• Acute posthemorrhagic anemia ••• Hemolytic anemia.
Abbreviations • SSGE - average Hb content in erythrocytes • SEV - average erythrocyte volume.
ICD-10 • D50–D53 Nutrition-related anemias • D55–D59 Hemolytic anemias • D60–D64 Aplastic and other anemias
APPLICATIONS
Congenital dyserythropoietic anemia • Type I (*224120, 15q, CDAN1, r gene). Clinical picture: moderate developmental delay, macrocytic dyserythropoietic anemia, mild hemochromatosis, bone marrow Gaucher cell-like macrophages. Laboratory tests: N-acetylglucosaminyl transferase II deficiency • Type II (*224100, 20q, CDAN2 gene, HEMPAS, r). Clinical picture: dyserythropoietic anemia, multinucleated erythroblasts, lysis of red blood cells upon serum acidification, bone marrow Gaucher cell-like macrophages. Laboratory tests: N-acetylglucosaminyl transferase II deficiency (EC 2.4.1.138) • Type III (*105600, 15q21, CDAN3, Â, r gene). Clinical picture: congenital dyserythropoietic anemia, macrocytosis, giant multinucleated bone marrow erythroblasts, jaundice; increased risk of myeloma or monoclonal gammopathy. Laboratory findings: hemosiderinuria, abnormal nuclei and intracytoplasmic inclusions in erythroblasts, highly polyploid giant mononuclear erythroblasts, elevated serum thymidine kinase levels. ICD-10 • D64.4 Congenital dyserythropoietic anemia
Megaloblastic thiamine-sensitive anemia (*249270, 1q23.2–q23.3, TRMA gene, r) is combined with diabetes and sensorineural hearing loss. Clinical picture: megaloblastic anemia, sensitive only to thiamine, ring-shaped sideroblasts, diabetes, sensorineural hearing loss, dysphonia, progressive optic atrophy, transposition of internal organs, generalized edema, congenital septal heart defects. Laboratory tests: aminoaciduria, a-ketoglutarate dehydrogenase deficiency, iron accumulation in erythroblast mitochondria. ICD-10. D53.1 Other megaloblastic anemias, not elsewhere classified
Anemia myelophthisis is a normochromic normocytic anemia that occurs when normal bone marrow is replaced by pathological tissue. Etiology • Lymphoma • Leukemia • Multiple myeloma • Tuberculosis • Granulomatosis • Metastasis of a malignant tumor to the bone marrow. Diagnostics. The appearance of immature leukocytes and nucleated red blood cells in the peripheral blood in a disproportionately large number relative to the severity of anemia, metastatic cells (solid tumor metastases). Bone marrow puncture and trephine biopsy confirm the diagnosis. Treatment is etiotropic and symptomatic. Synonyms • Myelopathic anemia • Leukoerythroblastosis. ICD-10 • D61.9 Aplastic anemia, unspecified
Anemia due to erythropoietin deficiency is normochromic (sometimes hypochromic) normocytic hyporegenerative anemia. Erythropoietin deficiency occurs in chronic renal failure when the level of end products of nitrogen metabolism in the blood increases and creatinine clearance is less than 45 ml/min. The severity of anemia usually depends on the severity of renal failure (it is most severe with primary damage to the glomerular apparatus). Etiology and pathogenesis • The synthesis of erythropoietin is suppressed by a high content of uremic toxins (in anemia as a result of chronic diseases, this effect is mediated by cytokines), which leads to the suppression of erythropoiesis • The sensitivity of the bone marrow to erythropoietin is reduced • The lifespan of erythrocytes is shortened (minor hemolysis) • Nutritional deficiency of folic acid is possible acid or iron • Uremic hemorrhagic diathesis; possible hemorrhages in the pleura, pericardium, brain •• When the endothelium of the renal vessels is damaged (malignant arterial hypertension, periarteritis nodosa, acute ischemia), microangiopathic hemolytic anemia occurs with fragmentation of erythrocytes and thrombocytopenia (in children it occurs acutely in the form of hemolytic-uremic syndrome). Treatment is etiotropic and pathogenetic • Recombinant erythropoietin is the drug of choice. Initial dose: 50–100 units/kg IV or SC 3 times a week. After 2–3 months of treatment, the erythrocyte count increases in most patients. It is necessary to monitor the concentrations of iron and folic acid in the blood, because their deficiency can lead to secondary complications • Blood transfusions (use with caution). ICD-10. B63.8 Anemia in chronic diseases classified elsewhere (specify the cause of chronic renal failure)
Microangiopathic hemolytic anemia is a secondary or congenital anemia that develops due to narrowing or obstruction of small blood vessels, which leads to mechanical damage to red blood cells during their interaction with the vascular endothelium. Etiology • Arterial hypertension • Chronic kidney disease • Prosthetic heart valves • Hemolytic-uremic syndrome • Disseminated intravascular coagulation (DIC) • Congenital microangiopathic hemolytic anemia (276850, r): polymorphic symptoms, possible involvement of the central nervous system; occurs due to fibrin deposition or the formation of platelet thrombi in the arterioles and capillaries of most organs; Characterized by thrombocytopenia, episodes of fever and petechial rash, glomerulopathy, megakaryocytosis (bone marrow). The clinical picture is determined by the underlying disease. The diagnosis is confirmed by identifying fragmented red blood cells in a peripheral blood smear in the form of schizocytes, spur cells and other abnormal forms of red blood cells. Treatment is etiotropic and restorative. ICD-10 • D59.4 Other non-autoimmune hemolytic anemias
Acute posthemorrhagic anemia is a normochromic normocytic hyperregenerative anemia that occurs as a result of acute blood loss over a short period of time. The minimum blood loss that poses a danger to the health of an adult is 500 ml. The severity of the clinical picture is determined by the amount of blood lost, the speed and source of bleeding. Etiology • Trauma • Surgical interventions • Ectopic pregnancy • Impaired hemostasis • Various diseases of internal organs accompanied by acute bleeding (for example, peptic ulcer of the stomach and duodenum). Clinical picture • General signs of anemia (tachycardia, shortness of breath, drop in blood pressure and venous pressure, pallor of the skin and mucous membranes). The severity of these changes does not correspond to the severity of anemia, because they often appear in response to a cause of bleeding (such as pain or injury) • Sudden dry mouth is an important sign of acute bleeding. Treatment is aimed at restoring blood volume • Surgical stop of bleeding • Blood transfusions. ICD-10 • D62 Acute posthemorrhagic anemia
Anemia in chronic, infectious and oncological diseases (as a rule, normochromic normocytic hyporegenerative anemia, in 40% of cases - hypochromic microcytic anemia) ranks second in frequency after IDA. Etiology and pathogenesis • Shortening of the period of circulation of mature forms of erythrocytes in the blood • Impaired utilization of iron (its release from the depot is impaired) • Relative deficiency of erythropoietin (the effect is mediated by the suppression of its production by cytokines - b- and g-IFN) • Altered bone marrow response to erythropoietin. The clinical picture is determined by the underlying disease (for example, rheumatoid arthritis, tuberculosis, cancer). Diagnosis • Moderate anemia (Hb concentration 80–100 g/l) • Serum ferritin concentration is normal or slightly increased (unlike IDA) • Fe2+ content in the blood serum is reduced, but TIVR is also reduced (unlike IDA) • Amount reticulocytes are reduced (hyporegenerative anemia). Treatment is etiotropic. ICD-10 • D63* Anemia in chronic diseases classified elsewhere •• D63.0* Anemia in neoplasms (C00-D48+) •• D63.8* Anemia in other chronic diseases classified elsewhere
Reticulocyte index. Calculation method: 0.5´(reticulocyte content´Ht of the patient/normal Ht). The content of reticulocytes is expressed as a percentage of the number of red blood cells; 0.5 — correction factor taking into account the severity of anemia; instead of Ht, you can use the volume of cell mass (BCV).
Cost of consultation for anemia?
| Name of service | Price, rub.) |
| Initial appointment with a cardiologist | 1800 rub. |
| Repeated appointment with a cardiologist | 1300 rub. |
| Primary appointment with a general practitioner | 1800 rub. |
| Repeated appointment with a general practitioner | 1300 rub. |
| Prescription of treatment (drawing up an individual treatment regimen) | 1000 - 2500 rub. |
All our services and prices
Diagnostic measures
To treat anemia, it is necessary to determine its type and cause of development. The main diagnostic method for this disease is laboratory blood tests (general and biochemical).
Changes that are observed in the general blood test:
small red blood cells (microcytosis).
Changes that are observed in the biochemical blood test:
In addition, a visual examination of the patient and a detailed history is required. Among the most common symptoms are pale skin and mucous membranes, cracks in the corners of the mouth, a “glossy” tongue, and an enlarged spleen.
To effectively correct the condition, instrumental examination methods may also be required:
computed tomography of the esophagus, stomach, duodenum. colonoscopy. Ultrasound of the liver, spleen, kidneys, genitals. X-rays of light.
Treatment of anemia
The course of medical therapy is carried out on the basis of the diagnosis and includes the prescription of a special diet and medications, as well as, if necessary, surgical intervention to eliminate the causes of blood loss.
A balanced diet is of great importance for anemia. It compensates for the lack of iron and microelements involved in hematopoiesis. Nutritionists recommend eating foods rich in vitamin B12, folic acid and iron. The diet must contain meat, offal (liver, heart, tongue), fish, egg yolks, mushrooms, buckwheat, legumes, black currants, pomegranate, strawberries, nuts, apples, rose hip decoction, dried fruits. Vitamin C accelerates the absorption of iron by the body, while strong tea, coffee, and calcium hinder it. Strong alcoholic drinks are harmful to a patient with anemia.
Iron supplements are considered the most effective for combating anemia. They are better absorbed, increase hemoglobin levels faster, restore its reserves in the body, and eliminate weakness and fatigue. Based on blood test data for each patient, depending on a number of indicators (type of anemia, severity of the disease and the cause of its development, age of the patient), an individual daily dose, course duration, and preventive measures are calculated. In severe cases, intramuscular and intravenous administration of ampoule iron preparations in a hospital setting is possible to avoid adverse reactions and allergies.
It is advisable to take iron supplements one hour before meals or two hours after meals. Medicines should not be taken with tea or coffee. These drinks reduce iron absorption. You must use water or juice.
The prognosis for iron deficiency anemia is favorable in most cases. The patients' condition improves significantly, the body's resistance increases, sleep and appetite normalize. The basis for preventing anemia is a balanced diet. Do not get carried away with protein foods and sweets. There should be vegetables, herbs and fruits on the table all year round. Another rule is to maintain a healthy lifestyle, exercise, walks in the fresh air, proper rest and good sleep.
Sign up for an anemia screening
Make an appointment
Disease prevention
To prevent the development of anemia, you need to eat right, following a balanced menu. To do this, you need to include beef liver and kidneys, quail and chicken eggs, fresh vegetables and fruits in your diet.
Since women are at risk for developing anemia, they should donate blood for clinical testing more often than men, which will allow timely detection of the disease. If a person, regardless of his gender and age, discovers signs of anemia, he should consult a doctor and begin treatment. Otherwise, it will not be possible to avoid serious health problems.
Author of the article:
Shutov Maxim Evgenievich |
Hematologist Education: Graduated from Kursk State Medical University in 2013 and received a diploma in General Medicine. After 2 years, he completed his residency in the specialty “Oncology”. In 2021, she completed postgraduate studies at the National Medical and Surgical Center named after N.I. Pirogov. Our authors