Heart blocks are pathological conditions in which the conduction of nerve impulses inside the heart muscle is disrupted or completely stopped. In a normal heart, electrical impulses occur at a certain frequency in the natural pacemaker, the so-called. sinus node. The impulse originating in the sinus node spreads through the conduction system of the heart, passing through the atria and ventricles. The function of the conduction system is to ensure coordinated work of different parts of the heart, ensuring maximum contraction efficiency.
Causes of heart block
Heart blocks can occur with almost any damage to the heart: coronary heart disease, myocardial infarction, myocarditis, cardiosclerosis, increased stress on the heart
muscle (for example, in athletes or with high blood pressure), as well as in overdose and misuse of certain medications.
Heart blocks can be caused by a hereditary predisposition or a disorder of intrauterine development.
At CELT you can consult a cardiologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
Bundle branch block, how dangerous is it?
Sometimes in the transcript of the cardiogram you can see the inscription “bundle branch block”. How dangerous is it and what is it like?
To answer the question posed, it is necessary to say a few words about the electrophysiology of the heart muscle.
As you know, the heart consists of four chambers - the left and right atrium, the left and right ventricle. Each chamber has different nerves. But the heart also has a distinctive feature: in the area of its right atrium there is a special zone called the sinus node, in which an electrical impulse is generated that causes the human heart to contract. From this sinus node there are three branches, called bundles, through which, in fact, the electrical impulse is transmitted. These bundles cover the right and left atrium, and are called the bundles of Wenckebach, Thorel and Bachmann. Next, the bundles gather into the so-called atrioventricular node (AV node), after which they spread to the right and left ventricles, forming two branches - the left branch of the His bundle and the right branch of the His bundle.
In turn, the left bundle branch branches into the anterosuperior branch of the left bundle and the posteroinferior branch of the left bundle.
In some cases, a person develops pathologies in which the transmission of an electrical impulse along one or another bundle or leg is stopped or modified. Such pathological conditions are called blockades. Some of these blockades are relatively harmless to human health, and some require urgent medical intervention.
Right bundle branch block (RBBB) is divided into complete or RBBBB and incomplete or IRBBB, this is assessed by certain criteria on the ECG.
If it is not caused by another disease, then RBBB itself is not very dangerous and does not require any treatment. However, in some cases it can be a harbinger of quite dangerous complications, for example, developing as a result of overload of the right side of the heart. In such cases, it is necessary to conduct additional studies, primarily echocardiography or echocardiography, which will give an answer about the presence or absence of the above pathology. On EchoCG, the doctor will see all parts of the heart, whether there are signs of pulmonary hypertension, whether the cavities are enlarged, whether there are any pathological changes in the valves that lead to overload of the heart. Also, complete blockade of the right leg may be a limitation for taking certain antiarrhythmic drugs, which is also important. But the blockade of the right leg in itself does not do anything bad and the person does not die from it.
Incomplete blockade of the right leg, especially if it is detected for the first time, also requires additional studies in the form of echocardiography to exclude the same causes.
Complete left bundle branch block (LBBB) is a more serious pathology. If it is detected for the first time, according to the recommendations of Russian Healthcare, the patient should be urgently hospitalized. This precaution is due to the fact that PBLBB can be a consequence of transmural infarction of the anterior wall or apex of the left ventricle, which is a very large infarction. In order to determine the presence or absence of a heart attack, it is necessary to conduct additional studies in a hospital setting.
Among other studies, an echocardiography is performed, during which the doctor monitors the contraction of the heart walls. If no signs of a heart attack are found, then most likely, PBLBB is not caused by any pathology of the coronary arteries, but is an independent disease.
The blockade can be transient, transient or tachydependent, that is, appear on the ECG or 24-hour monitor only when the pulse accelerates. Such a blockade is not treated in any way, but is only observed or symptomatic measures are taken, for example, slowing down the pulse with the help of certain medications. Such blockades may limit the use of certain antiarrhythmic drugs.
A special feature of PBLBB is the fact that it is often more difficult to track possible deterioration in the blood supply to the heart and other signs of changes in heart function against its background using an ECG. Therefore, such patients, for example, can no longer undergo an ECG stress test in the form of a bicycle ergometry or treadmill test, but only need a stress echocardiography, during which an ultrasound of the heart is performed under stress, since an ECG against the background of a complete block of the left leg is no longer very informative.
There are some other types of blockades of the legs of His, such as blockades of the anterior branch and posterior branch of the bundle of His. These branches arise from the left bundle branch, which was mentioned above, and they can also become blocked.
These types of blockades can also be a manifestation of certain pathological changes in the heart: for example, ventricular hypertrophy or changes in the position of the heart. If the diseases described above are excluded, they themselves do not have much significance. For example, combined anterior-superior branch blockade and right leg block, or a combination of anterior-superior branch block and left leg block, have clinical significance in the form of restrictions on the prescription of certain classes of antiarrhythmic drugs or in increasing the risk of developing serious complications such as a complete three-bundle block that requires installation pacemaker. But again, there is no specific drug treatment for such blockades.
You can also find the phrase in the ECG report: local intraventricular block or local disturbances of intraventricular conduction; these phrases do not have important clinical significance and are not dangerous.
Thank you for your attention!
Classification of blockades
Heart blocks are classified either by the area where the signal does not pass, for example, between the atria and ventricles, or by the degree to which conduction within the ventricles is slowed down.
Atrioventricular blockade comes in three degrees:
- 1st degree blockade - impulses, for example, from the atrium to the ventricle are conducted more slowly than normal (impulse delay);
- 2nd degree blockade - only part of the impulses are not carried out;
- 3rd degree block - when all impulses from the atria to the ventricles are not carried out, the chambers of the heart contract uncoordinatedly (complete transverse block). The heart rate can drop to 30 per minute and intervals between contractions can reach several seconds and loss of consciousness is possible (Morgagni-Adams-Stokes attacks), which can result in a life-threatening condition.
When the propagation of impulses inside the ventricles slows down, they speak of blockade of the branches or branches of the bundle of His (named after the anatomist who described the nerve bundles of the heart).
All blockades can be transient (appear briefly) or persistent (exist permanently).
Classification
There are several classifications. According to the degree of violation there are:
- Incomplete blockade (partial), when the passage of the impulse only slows down, and the QRS complex has a length of 0.10-0.11.
- Complete blockade, when the conduction of the impulse completely stops and the QRS complex expands more than 0.12.
- According to the location of the violation, they are distinguished:
- Monofascicular or single-start, when a conduction disorder is formed in one branch of the His bundle - in the right leg, the left leg of the anterior branch, or the left leg of the posterior branch.
- Bifascicular or bifascicular block, when conduction is disrupted in the left leg, the left leg of the anterior branch and the right leg, or the left leg of the posterior branch and the right leg.
- Trifascicular or three-fascicle blockade, when the disorder occurs in all three branches.
- Local, peri-infarction or focal blockade, when local splitting of the QRS complex occurs. That is, the lesion occurs in some limited area of the left ventricle, in a certain area. As a rule, a lesion forms in the area adjacent to the resulting necrotic area during myocardial infarction. In other words, it arises distal to the main branches of the left and right bundle of His.
- Peripheral intraventricular block is called if the peripheral branches of the legs are involved in the process.
- Proximal, when the lesion is located inside the His bundle.
- Distal blockade is called if the lesion is localized at the level of the branches of the left leg or in the right.
By nature, intraventricular blockades are divided into:
- Permanent, when there is a constant disturbance in the conduction of the impulse.
- Variable or intermittent. You can also find names such as alternating, transitional or latent. All these are names of the same disorder, when the passage of the rhythm slows down, less often stops, for some reason, and then is restored again.
There is also the concept of nonspecific intraventricular blockades or arborization ones, when the electrocardiogram data in any one or several branches does not fit the currently available signs. At the same time, the width of the QRS complex does not change significantly. This picture is observed when the patency of the impulse along the distal (terminal) branches of the legs is impaired. However, with diffuse lesions of the heart muscle, the ventricular complex always expands. They are also distinguished by the degree of damage: first, second, third and fourth degrees. All types of intraventricular blockades can be combined with each other. In clinical cardiology, it is customary to indicate in detail what type of disorder. This further helps in prescribing adequate treatment. Symptoms As a rule, the disease does not have pronounced symptoms, except for general fatigue and tiredness. With transverse incomplete blockades, loss of pulse and/or heart sounds may occur. Patients sometimes complain of a feeling of a sinking heart. In cases of complete transverse blockades, persistent bradycardia occurs with all its clinical manifestations. In these cases, Dahms-Stokes-Morgagni syndrome often occurs. If the transverse complete block is also distal, then the risk of developing angina or heart failure, and sometimes sudden death, increases. Diagnostics Usually one ECG is enough to make a diagnosis. If necessary, the doctor may prescribe an ultrasound of the heart. And for intermittent blockades - Holter ECG monitoring. Causes
- Myocarditis.
- Ischemic myocardial disease (CHD).
- Congenital heart defects.
- Cardiomyopathies.
- COPD
- Aortic stenosis, especially complicated by calcification.
- Heart bruise.
- Hyperkalemia.
- Hypertonic disease.
- Heart operations.
- Neoplasms of the heart.
- Muscular progressive dystrophy.
- Lenegra's disease.
- Syphilitic gumma.
- Lev's disease.
- Overdose of procainamide, quinidine, strophanthin K.
- Acquired defects, especially with rheumatoid lesions, usually cause the formation of a right leg.
- Cor pulmonale also usually causes damage to the right leg.
Treatment Mild bundle branch block usually does not require any treatment. Moreover, it is not amenable to drug therapy. It should only be taken into account when prescribing medications. For proximal blockades, atropine or its analogues are sometimes prescribed, but the effect is short-lived. Therefore, all therapy ultimately comes down to treating the disease that caused the blockade. In other words, to eliminate the cause. In case of Dams-Stokes-Morgagni syndrome or the occurrence of heart failure and/or peripheral circulation, as well as angina, permanent or temporary ventricular stimulation is prescribed. Treatment prognosis and prevention. The prognosis of treatment largely depends on the degree of damage to the myocardial conduction system and the timely administration of adequate treatment for the causative disease. Prevention consists of timely treatment of the disease, which can lead to intraventricular blockades, maintaining a healthy lifestyle and regular professional activities. examinations by a doctor.
consultation with a cardiologist
Treatment
Blockades of individual branches of the cardiac conduction system sometimes do not require special treatment, but may indicate the presence of some kind of heart disease that requires therapy. Some blockages are eliminated by prescribing medications. On the other hand, there are medications that themselves contribute to the occurrence of blockades. Therefore, before “treating” the blockade, it is necessary to clarify whether the patient is taking any medication, or a combination of drugs that affects intracardiac conduction, their dosage and time of administration.
Blockades of the 3rd degree, or complete blockades, as a rule, significantly worsen the patient’s well-being and also affect the prognosis of the disease. In these cases, implantation of an artificial pacemaker (pacemaker) is absolutely necessary.
In the multidisciplinary CELT clinic, a complete examination of the patient is possible to identify and timely treat blockades and, if necessary, implantation of an artificial pacemaker (PAC).
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Publications in the media
Intraventricular block - a slowdown or complete cessation of the conduction of excitation to the ventricular myocardium, caused by damage to the conduction system of the heart at the level of the legs of the His bundle and their branches • There is partial or complete blockade of one or two branches of the His bundle - respectively, single-fascicular block (monofascicular) and double-fascicular block (bifascicular ) • Complete blocking of the depolarization wave along the three branches of the His bundle (trifascicular, trifascicular block) leads to third-degree AV block • Various combinations of partial and complete blockades of the branches of the His bundle are also possible.
Classification • Single-beam (monofascicular) •• right leg •• anterior branch of the left leg •• posterior branch of the left leg • Double-beam (bifascicular) •• left leg •• right leg and anterior branch of the left leg •• right leg and posterior branch of the left leg • Three-bundle (trifascicular) • Arborization (nonspecific intraventricular block) • Focal (peri-infarction) • Blockades are also distinguished between complete and incomplete (partial), persistent and transient (transient).
Etiology • Congenital heart defects (VSD, pulmonary artery stenosis) • COPD • Hypertension • Aortic stenosis with calcification • Cardiomyopathies • Myocarditis • IHD • Cardiac contusion • Hyperkalemia • Progressive muscular dystrophy • Overdose of quinidine, procainamide, strophanthin K • Surgical operations on heart • Syphilitic gumma • Neoplasms of the heart • Lenegra's disease • Lev's disease, etc.
LEFT BUNCH BLOCK
complete cessation of conduction of excitation along the left leg of the His bundle or simultaneously along its anterior and posterior branches. Always a sign of pathology; observed with a frequency of 0.5–2%, extremely rarely develops in children (0.005%). In 90% of cases it occurs after 50 years, the main causes are ischemic heart disease and arterial hypertension; often masks ECG signs of MI.
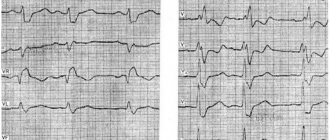
ECG identification
• Complete blockade of the left bundle branch •• Widening of the QRS complex ³0.12 s in all leads •• Monophasic positive without q wave, deformed R in leads V5–6, I, aVL •• In leads V1–2 QRS type rS or QS • • Shift of the transition zone to the left •• Increased amplitude of the QRS complex waves in the left precordial leads •• Discordant deviation of the ST segment and T wave in all leads •• The electrical axis of the heart (EOS) is deviated to the left (not necessarily).
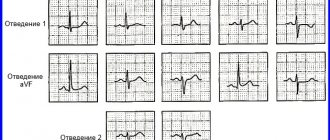
• Partial (incomplete) blockade of the left bundle branch •• QRS >0.12 s •• The q wave is absent in I, aVL, V5–6 • In V1–2 QRS type rS or QS •• Changes in the ST segment and T wave are uncharacteristic •• Often combined with severe left ventricular hypertrophy •• Blockade of the anterior branch of the left bundle of His. The main diagnostic sign is deviation of the EOS to the left, angle a ³(–30°) (the S wave in standard lead III is greater than the S wave in standard lead II, RI< SIII, RII=SII), QRS £0.11 s •• Posterior blockade branches of the left leg of the His bundle. The main diagnostic sign is deviation of the EOS to the right, angle a ³ (+90°) (pronounced S wave in standard leads), QRS £0.11 s. It should also be taken into account that in older people, deviation of the EOS to the right is most often a sign of pathology. The specificity of ECG signs of blockade of the posterior branch of the left bundle branch of His is low, so it is necessary to exclude hypertrophy or acute overload of the right ventricle.
BLOCK OF THE RIGHT BAND OF HIS BUNCH
Complete cessation of conduction of excitation along the right branch of the AV bundle. In young people it is observed in 0.15–0.20%, and in 50% of cases the blockade is not associated with organic changes in the heart muscle. In the age group over 40 years old, the frequency reaches 5%. May hide ECG signs of large-focal myocardial changes.
• ECG identification •• Widening of the QRS complex ³0.12 s in all leads •• In lead V1 (sometimes V2) the shape of the ventricular complexes is Rs or rSR' (qR - more often when combined with right ventricular hypertrophy) •• Discordant deviation of the ST segment and T waves in the right precordial leads •• Deviation of the EOS to the right (optional).
• Incomplete (partial) form of right bundle branch block is characterized by the same morphological criteria as right bundle branch block, but the duration of the QRS complex is £0.11 s.
Treatment of the underlying disease.
ICD-10 • I44 Atrioventricular [atrioventricular] block and left bundle branch block [Hisa] • I45 Other conduction disorders
Notes • Arborization heart block is a violation of the transition of excitation from the terminal branches of the conduction system of the heart to the contractile myocardium (for example, with diffuse myocardial lesions); manifested on the ECG by expansion of the ventricular complex • Peri-infarction heart block - transient heart block in parts of the conduction system adjacent to the necrotic area during MI.
Diagnostics
First, the cardiologist will review the patient's medical history and ask questions about your general health, diet and activity level, and family medical history.
In addition, he will ask about the medications the patient is taking, as well as about bad habits. The doctor will then listen to your heart and check your pulse for signs of heart failure, such as fluid retention in your legs and feet.
In addition, to diagnose heart block, use:
- ECG – this will show the heart rate and rhythm, as well as the timing of electrical signals as they pass through the heart;
- A Holter monitor is a portable ECG that is attached to the patient’s body and records heart activity from 24 to 48 hours;
- An event monitor is another type of portable ECG that is worn over an extended period, where the device records heart activity at specific times rather than continuously;
- Electrophysiology test - This test uses thin flexible wires (catheters) that are placed on the surface of the heart to record its electrical activity.
Treatment of intraventricular block
It is important to take into account the fact that blockade is not an independent disease. To begin therapy, the underlying pathology must be identified.
If a patient experiences atrioventricular block, a pacemaker is usually placed. The combination of complete left bundle branch block and heart failure is an indication for resynchronization therapy
Indications for patient hospitalization are:
- planned implantation of a stimulator;
- suspicion of myocardial infarction;
- acute occurrence of left bundle branch block;
- the need to select complex therapy for arrhythmia.
Important! Any disease of the cardiovascular system requires complex therapy. If medications do not give the desired result, surgical interventions are performed.
They may include installing:
- electrical pacemaker;
- stenting or bypass surgery.
Modern techniques make it possible to solve problems in a minimally invasive manner. Endovascular surgery, for example, allows a number of heart surgeries to be performed with minimal risk to patients' health.
Patient management includes:
- therapy of the underlying pathology;
- periodic recording of ECG;
- conducting a Holter study.
Are you interested in the prices of pathology therapy in Moscow? We have posted a price list on the website. You can find out the price of a consultation with a cardiologist and tests by calling specialists. We adhere to a loyal pricing policy. Thanks to this, everyone can use our services.
Popular questions and answers
Cardiologist Stanislav Snikhovsky answered our questions about heart block.
What complications can occur with heart block?
Clinically, all heart blocks are manifested by slowing of the pulse.
When the pulse rate decreases, fainting conditions associated with a lack of blood circulation to the brain may develop. Patients may complain of irregular heartbeat, headache and shortness of breath. With complete heart block (pulse about 40 beats per minute or less), Morgagni-Edams-Stokes syndrome develops, which is manifested by convulsions and loss of consciousness. Complete heart block causes rapid development of heart failure and can be fatal.
When to call a doctor at home if you have a heart block?
If there is sudden general weakness or fainting, a rare (less than 50 beats per minute) or very weak pulse, a feeling of irregular heartbeat, sudden shortness of breath and a feeling of lack of air, you should immediately call an ambulance.
Incomplete blockade of the anterior branch of the left leg (Dilation of the left ventricle)
Left anterior branch block is sometimes caused by left ventricular dilatation, which stretches this thin branch. This origin of the blockade may be the reason for its development in patients with aortic valve insufficiency. This blockage most often occurs with rapid or acute development of left ventricular dilatation.
In hypertension, anterior branch blockade may be due to hypertrophy and dilation of the left ventricle and the mechanical pressure of high blood pressure on the conduction system of the heart.
Rarely, blockade of the anterior branch of the left leg is a consequence of idiopathic isolated sclerosis and calcification of the conduction system. Blockade of this branch also occurs with congenital heart defects, more often with atrial or ventricular septal defects.
In an epidemiological study, blockade of the anterior branch of the left leg was detected in 1.5% of people aged 45–69 years. In 60% of them this was the only sign of myocardial damage. They indicate a high incidence of myocardial fibrosis in patients with this blockade, which was most often associated with cardiosclerosis and less often with hypertension, various cardiopathy or congenital heart diseases. However, such ECG changes can occasionally be observed in healthy people.
If blockade of the anterior branch of the left leg is recorded not in healthy people, but in patients with heart disease, it suggests the presence of pronounced changes in the myocardium.
“Guide to electrocardiography”, V.N. Orlov
Read further:
Incomplete blockade of the anterior branch of the left leg (displacement of the electrical axis of the heart to the left in dynamics)
Incomplete blockade of the anterior branch of the left leg can also manifest itself as a displacement of the electrical axis of the heart to the left in dynamics. This shift of the electrical axis of the heart to the left may be due to the progression of conduction disturbances in the anterior branch. For example, if a patient with a normal position of the electrical axis of the heart and Ða=+60° suddenly has a displacement of the electrical axis of the heart to 0°, then this indicates the appearance.