Symptomatic and asymptomatic, etiological and idiopathic myocarditis is called diffuse when a large area of the muscle is affected. If this is non-idiopathic myocarditis, then the platform for its development can be (this is important for recognizing and treating diffuse inflammation ) bacteria, fungus, virus, infection.
Due to the extensive (or diffuse) damage and clinical picture, often adjacent to the symptoms of acute respiratory viral infections / acute respiratory infections, myocarditis of this type is called a “heart cold”. From the point of view of manifestations of diffuse inflammation, this is justified. Approximately 2/3 of the signals of myocarditis are similar to those of influenza, especially in the acute, subacute phase.
- lethargy up to a subcopal (pre-fainting) state;
- CFS;
- regular elevated temperature during myocarditis with signs of diffuse inflammation often provokes the development of low-grade fever.
Diffuse myocarditis is distinguished from a cold by signs of cardiac conduction disturbances and degenerative processes. These include diffuse symptoms such as shortness of breath (including postopnea - lack of air in a horizontal position), a feeling of freezing, stopping, tightening of the heart in a vice, pain in the chest and chest.
Myocardial dystrophy as a consequence of physical overexertion
Myocardial dystrophy can be a secondary disease that manifests itself against the background of other heart diseases that are not fully cured.
But often the heart muscle weakens due to too intense stress on the body. Excessive exercise is not beneficial, as organs begin to work at an accelerated rate and quickly wear out. Each person has his own body and his own physical capabilities, which allow him to perform some kind of work, do complex exercises and win competitions. Negative changes in the work of the heart occur not just from constant sports training, but precisely from the discrepancy between the loads and the individual capabilities of the body. If these possibilities and their limits are not taken into account, very soon the heart and other organs will begin to suffer serious failures. Regardless of what factors provoke the development of myocardial dystrophy, you need to take into account your personal characteristics and know the limit of physical stress that should not be crossed. For example, the same changes in the work of the heart muscle will occur in a trained athlete who runs a marathon at speed and in an ordinary person who is not keen on sports, who had to catch up with a leaving minibus at a pace that is unusual for his body. This suggests that every person should sensibly assess the capabilities of their muscles, respiratory system and heart, so as not to create unbearable working conditions for themselves or get carried away with overly complex and long workouts.
There are two types of heart strain: acute and chronic. Acute is the most dangerous, as it sometimes entails irreversible changes and complications that, if you are not attentive to your condition, can lead to death. These are hemorrhages in the heart, myocardial dystrophy or even a heart attack. If this type manifests itself in a mild form, then it is possible to immediately notice and stop any stress on the heart until it returns to normal. Heart pain manifests itself, and serious changes will be observed during an ECG check. A person may suffer from shortness of breath during any exertion, which was not the case before, and may also experience disturbances in the rhythm of the heartbeat.
If we talk about the chronic form, then most often this is actually myocardial dystrophy. It often manifests itself in fully trained athletes who have not been cured of some infectious disease that causes complications on the heart. These are tonsillitis, cholecystitis, caries, which is usually chronic. At the very beginning of the manifestation of dystrophy, sports fans do not feel any health problems and therefore do not change their lifestyle, continuing to train at the same rhythm. This is the danger of the disease, that it is difficult to identify it in the initial stages without undergoing appropriate checks and studies of the body.
Etiology
The causes of dystrophy include:
- intoxication of the body;
- infectious foci;
- various disorders of the endocrine system (theriotoxicosis, thyroid diseases, hypothyroidism);
- hypovitaminosis and vitamin deficiency;
- anemia of various etiologies (insufficient amount of oxygen);
- obesity (cardiac obesity and general obesity - increasing body weight increases the load);
- angina pectoris;
- hypertension (insufficient blood supply to the heart muscles).
Intoxication is divided into exogenous and endogenous. Exogenous include industrial poisons and toxic substances. Endogenous include metabolic and functional disorders, liver and kidney diseases.
Myocardial dystrophy may not change pathologically or, on the contrary, may clearly manifest itself with various degeneralized changes - fatty, protein, waxy degeneration of muscle fiber, cloudy swellings, fatty infiltrates.
Causes
Changes in the functioning of the heart occur for several reasons related to sports activities. This:
- Frequent stress on the body due to training and preparation for serious competitions. Usually people, wanting to win, do not spare themselves and their bodies by exercising too much time. If we take into account not very good nutrition and lack of sleep and rest, then everything goes to the point that sooner or later the heart will begin to “protest” against this way of life. To prevent this, you should not torture yourself before the competition, exhausting yourself with back-breaking exercises without proper rest. Still, health is more important and should always come first. The healthiest and most resilient win, so it makes sense to take care of yourself before a serious event.
- Intense sports activities in physically unprepared people. If the body has not previously received such loads, then immediately excessive training can seriously damage the heart, since it will not cope with such rapid changes. The same applies when a person changes his sport and immediately begins to actively train in something in which he is still weak. To prevent overload on the heart, any vigorous activity should be started gradually, increasing the intensity.
- A combination of intense sports with strenuous work or other intellectual activities. A direct blow to the physical and mental areas of the human body can lead to malfunctions and even an emotional breakdown. The same applies to playing sports immediately after an infectious disease, such as tonsillitis, flu, etc.
Symptoms
You need to know the signs of myocardial dystrophy so that you can promptly seek medical help and begin treatment as soon as possible. The symptoms of the disease are:
- Shortness of breath and fatigue. This can manifest itself during severe stress that a person received constantly. The strange “behavior” of the body should alert you. You should never continue training if your heart is not behaving as usual. Shortness of breath can be bothersome even when walking or climbing stairs.
- Rapid or strong heartbeat. If earlier sports training did not cause any inconvenience, now the heart will actively react to any, even the smallest load. Strong muscle contraction is evidence of improper functioning of the organ.
- Dizziness, nausea and vomiting. All symptoms are similar to those of poisoning, even if the patient eats exclusively healthy food. These signs may indicate that the heart is not functioning properly.
- Muscle pain and weakness, which manifests itself constantly, even without much stress on the body.
- Loss of consciousness.
- Acute pain in the heart. It may indicate that myocardial dystrophy has acquired complications and leads to a heart attack. In this case, the pressure can drop sharply, and the person begins to suffocate from lack of oxygen. Sometimes you can observe a strong cardiac cough and wheezing in the chest area.
If such symptoms occur, the person should immediately stop any exercise and maintain maximum rest to allow the heart to recover. If pain occurs, it is important to immediately consult a doctor or call an ambulance, as this is an extremely serious situation. For several weeks you need to limit yourself to any sport and not participate in any competitions. The doctor can determine whether it is acceptable for the patient to start playing his favorite sport.
DIAGNOSIS AND TREATMENT of myocarditis
Myocarditis is a clinical syndrome characterized by many possible causes and manifestations. It is believed that viral infection is the most common cause of myocarditis, but similar changes can be caused by other infectious and non-infectious factors, the impact of which leads to inflammatory infiltration between cardiomyocytes.
Not only the causative factors of this pathological condition, but also its manifestations are very diverse. The diagnosis is clear in the presence of clear and characteristic signs of acute cardiac dysfunction that has arisen in connection with a viral disease, but with an erased clinical picture, diagnosing myocarditis is a very difficult task.
Definition. Myocarditis is a pathological condition in which an active inflammatory process occurs in the myocardium with necrosis and degenerative changes in cardiomyocytes; the pathomorphological picture differs from the changes observed during infarction. Cell death and fibrosis are observed. Inflammatory infiltration can be represented by any type of immune cells, and the histological nature of the inflammatory reaction often indicates the etiological factor.
Morbidity. It is difficult to give exact figures regarding myocarditis, since this pathological condition is very heterogeneous: in some cases it occurs hidden and therefore does not come to the attention of doctors; its chronic form can lead to dilated cardiomyopathy with manifestation many years after the onset of the disease.
Myocarditis is found in 1-4% of routine autopsies. In Europe and North America, viral infections are considered the most common cause of myocarditis. Cardiac pathology, according to some estimates, develops in 5% of all cases of viral diseases; however, clinically significant cardiac damage, according to large studies, is observed in 0.5-5.0% of cases.
The incidence is influenced by extreme factors, including age, as well as pregnancy and time of year. The incidence of myocarditis is high in infants, with a second peak in adolescence.
Etiology. The inflammatory response in the myocardium can arise from a number of different influences that damage cardiomyocytes (see table). Viral infections are considered the most common cause of myocarditis.
The mechanisms of damage to cardiomyocytes during viral infections are being actively studied: it is currently believed that viruses change the antigens expressed by cardiomyocytes, therefore, in addition to the direct replication of the pathogen, these cells are damaged by a constantly ongoing cellular immune reaction.
If this is so, then the immune response in a given patient determines the clinical manifestations of the infection.
Coxsackie viruses A and B, enteroviruses and influenza viruses are the most common etiological factors of myocarditis. Approximately 25-40% of patients infected with HIV (human immunodeficiency virus) show signs of cardiac dysfunction, which manifests itself clinically in 10% of cases.
Recently, there has been increasing recognition of the fact that cardiac pathology can also develop as a long-term complication of radiation therapy, with damage to the myocardium, valves or arteries - sometimes many years after irradiation. More advanced radiation therapy techniques are designed to protect against such complications.
Pathomorphology. Direct exposure to ionizing radiation, exposure to a toxin (such as in diphtheria), or an autoimmune reaction (such as in Mycoplasma pneumoniae infection) can damage cardiomyocytes and cause heart failure and arrhythmias, with the clinical picture depending on the extent of the damage.
Inflammation gives the myocardium a pale tint with rare small hemorrhages. Microscopy reveals a disturbance in the structure of muscle fibers due to interstitial edema and isolated foci of necrosis. The inflammatory infiltrate is usually represented by lymphocytes.
Depending on the etiological factor, more specific histological features may be found, such as non-caseating granuloma in sarcoidosis (see Fig. 1). Subsequently, complete resolution of the process often occurs without residual fibrosis, but in some cases focal healing with interstitial fibrosis is observed.
| Figure 1. Myocardial biopsy specimen for sarcoidosis (hematoxylin and eosin staining): inflammatory lymphocytic infiltration and non-caseating granuloma are visible |
Clinical signs. Clinical manifestations are very diverse and depend on the degree of cardiac dysfunction and the nature of the etiological factor.
Viral myocarditis may be preceded by a prodromal phase with flu-like symptoms, fever, muscle and joint pain, and rash. The time between the appearance of these signs and the onset of symptoms of cardiac pathology can range from several weeks to several years. Coxsackievirus appears to be the most cardiotoxic, especially in children.
Myocardial damage first manifests itself in the form of fatigue, shortness of breath, chest pain and palpitations, sometimes in the form of fainting. These symptoms are explained by insufficiency of systole and damage to the conduction system.
Chest pain may be associated with body position and movement, suggesting the possibility of pericarditis. In severe cases, acute left or right ventricular failure and cardiogenic shock occur. Sudden death may occur due to abnormal heart rhythms.
Physical examination reveals signs of heart failure: tachycardia (in classic cases, it is more pronounced than could be explained by fever), gallop rhythm, and in more severe cases, pulmonary edema or peripheral edema. The heart size is usually normal, and a murmur of mitral regurgitation may be heard. Sometimes atrial fibrillation develops. In some cases, a pericardial friction rub may be heard.
Diagnostics. There are no specific clinical signs on the basis of which this diagnosis could be made. The combination of an acute infectious disease and symptoms of myocardial pathology gives reason to suspect myocarditis.
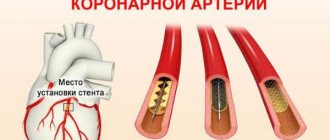
Myocardial pathology can be judged on the basis of ECG data (see Fig. 2), chest x-ray, echocardiography and determination of the level of cardiac enzymes. Pathological signs on the ECG are often observed in the form of nonspecific changes in the ST segment and T wave.
An X-ray of the chest organs reveals signs of pulmonary edema, and the heart may be enlarged. Echocardiography often reveals left ventricular dysfunction, and this change may be regional rather than diffuse. Nonspecific indicators of inflammation: leukocytosis, erythrocyte sedimentation rate, and C-reactive protein also help make the diagnosis.
The presence of an acute viral infection is confirmed by analyzing swabs from the throat, stool, and also on the basis of serological tests (which can reveal a fourfold increase in antibody titer). Sometimes it is possible to isolate the pathogen from fluid taken from the pericardial cavity.
Among the more complex research methods, gallium-67 scanning can be noted, which can detect an active inflammatory process.
Some tertiary centers advocate myocardial biopsy.
Treatment of myocarditis is carried out with the aim of:
- maintaining the pumping function of the heart and reducing the risk of progression of heart failure,
- fight against arrhythmia,
- identifying and eliminating sources of toxicity.
Ideally, all patients with suspected myocardial damage should be admitted to hospital and monitored to see how effective the treatment is.
General supportive measures include bed rest and restriction of physical activity. Animal experiments have clearly shown that exercise during acute myocarditis is harmful; During the recovery period, patients should be advised to limit sports activities. This is important given that many patients suffering from this disease are young.
In the acute phase of myocarditis, the condition of patients must be carefully monitored. For congestive heart failure, conventional treatment with diuretics and angiotensin-converting enzyme inhibitors is effective, as well as anticoagulant therapy when there are signs of peripheral or pulmonary embolism, severe ventricular failure, or atrial fibrillation.
In some cases, a clinical picture of cardiogenic shock and low ventricular output is observed, and adequate intensive care is necessary.
Arrhythmia may occur, requiring specific therapy. Occasionally, there is a need for temporary or permanent implantation of artificial pacemakers. It is generally accepted that the risk of sudden cardiac death is increased following myocarditis, especially in younger patients.
Specific therapy directed at the causative factor is limited. Since in most cases myocarditis develops against the background of viral infections and is based on immunological reactions, some studies have examined the role of antiviral and immunosuppressive therapy. Many of these studies were poorly controlled and their results were inconclusive. Currently, there are no clear data on the basis of which immunomodulatory therapy can be recommended.
It is best not to prescribe non-steroidal anti-inflammatory drugs, as some animal studies have shown that their use increases heart damage.
Most patients recover completely without evidence of residual cardiac dysfunction. Echocardiography allows accurate and noninvasive assessment of cardiac function, and, at least until cardiac function returns to normal, all patients should receive angiotensin-converting enzyme inhibitors.
With residual myocardial dysfunction, continuous treatment and specialist supervision is required, since in a small percentage of cases the disease recurs. Often the causative factor cannot be identified, but when it is known, it must be adequately addressed.
Rajesh K. Kharbanda , Fellow, British Heart Research Foundation Howerd Swanton , MD, Fellow, Middlesex Hospital
Treatment and prevention
If myocardial dystrophy has developed due to an untreated infection, then you need to make every effort to get rid of all foci of side diseases.
The underlying problem needs to be treated, and then the heart will get relief. If the disease is mild, you can be treated at home, only by seeing a cardiologist on time, who will adjust the therapy and give useful advice regarding lifestyle. The selection of medications, various procedures and measures will depend on the cause of myocardial dystrophy. If the root cause of the disease is serious overstrain of the body, muscle overload, then a competent doctor will prohibit any activities for a while to allow the heart to recover. And then he will adjust his training regimen to prevent a relapse. If dystrophy has arisen due to constant stress, emotional instability, the doctor will prescribe something soothing and offer to get rid of problematic situations as much as possible: change jobs, move to another place, stop communicating with negative people, watch depressing news, etc.
In any case, you need to spare your body, ensure good rest, which will bring joy and positive emotions. Surround yourself with friendly people and go for walks as often as possible, since you shouldn’t completely give up physical activity. If anemia occurs, you should start feeding your body the necessary vitamins that contain iron. For endocrine disorders, it is suggested to use hormones to restore the correct balance of all elements. Treatment of myocardial dystrophy will be individual in each case, so you should not start independent therapy without knowing the true cause of the disease. All treatment methods must be agreed upon with a doctor, who will first send you for examination in order to draw the right conclusions regarding the patient’s health.
It is much easier to prevent a disease than to treat it later. It is worth using all preventive methods that will protect the heart from disease. To do this, you need to train moderately and avoid even the slightest overload on the body. There must be proper nutrition, which will nourish the cells with the necessary substances, and the blood vessels will be in good shape.
How to treat left ventricular hypertrophy of the heart
As for treatment, therapy is carried out with the prescription of beta blockers in combination with verapamil. This treatment method allows you to reduce the symptoms caused by cardiovascular pathology. As the main adjunct to therapy, diet must be followed. It is also necessary to give up habits that harm the body. Experts do not rule out that surgical intervention will be required to remove the area of muscle that has undergone hypertrophy.
Permissible physical activity for myocardial dystrophy
Myocardial dystrophy requires partial rest so as not to overload the heart muscle.
After all, this can lead to serious complications and even death. But no one says that you need to give up sports completely. To treat the heart muscle, special physical therapy is provided, which allows you to develop the organ and thereby quickly treat it from the disease. At the same time, the “dosage” of such physical education should be prescribed on a strictly individual basis, since what is suitable for one person can be dangerous or even fatal for another. They use gymnastic exercises that exclude strength exercises, so as not to strain the heart. In addition to gymnastics, it is recommended to walk every day and gradually increase the walking time. The duration of gymnastics should not be more than half an hour, since patients need rest. The exercises used are those aimed at intense movements of the limbs. Breathing exercises are required to develop and train the diaphragm. All exercises must be done so that the load on parts of the body is distributed evenly.
In addition to therapeutic exercises, you can go on walking excursions, play volleyball, but no more than half an hour. Bathing and swimming will also be useful, but in moderate doses. In winter it is permissible to skate and ski. With myocardial dystrophy, it is advisable to spend the day actively, alternating physical activity with rest. One-time intense workouts that put the heart at risk by forcing it to work at full capacity should be avoided. Moderate body training will be beneficial if the disease has not taken an acute form, which requires only rest with limited movement.