A pregnant woman is the only link between the environment and the unborn child. All mother’s feelings are rather subjective and often colored by emotions. There are very few opportunities to assess the condition of the fetus in the womb:
Ultrasound allows you to visually assess the structure of the body and organs, the size of the child, and determine the expected weight. And thanks to this data, you can find out the condition of the fetus;
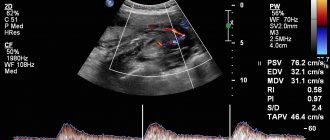
Dopplerography is a method for assessing fetal blood flow;
CTG is a method based on recording the fetal heartbeat curve and its evaluation.
Principles of CTG recording:
* The fetal heartbeat cannot be recorded for every woman and not at any time;
*Registration is made for a period of at least 30 weeks. In all other cases, it will not be possible to decipher the recording, since the heartbeat cannot be analyzed at an earlier time;
* A CTG recording can be prescribed before 30 weeks if the obstetrician-gynecologist cannot find the point at which the baby’s heart is heard. The device may be more sensitive than the doctor's ear. And the second option, the recording is made for the purpose of recording the heartbeat on paper, so that it can be attached to the pregnancy history;
*Recording is done for 10 minutes or longer. In a short period of time, it is quite difficult to assess the entire picture of the heart’s work;
* It is important to choose the right time to record. A woman should rest after traveling to the consultation. Before recording, eat, but not heavily;
* The child should not sleep during the diagnosis. A baby, like an adult, has a daily routine. Every mother knows when her baby moves the most and when he sleeps. Decoding the data directly depends on how active the fetus is;
*Recording must be done in a position comfortable for the woman;
* A special gel must be applied to the sensor, which improves the conductivity of impulses;
* The recording is more informative if fetal movements during pregnancy are recorded along with it. During childbirth, uterine contractions and the heartbeat response to them are recorded;
* Decoding must be done exclusively by a doctor. There are a lot of options for normality and pathology and they do not obey only one system. In order to say about normality or pathology, you need to evaluate the whole picture. There are CTG options that, according to ordinary decoding methods, fit the normal variant, but are exceptions and represent signs of severe conditions during pregnancy.
Every expectant mother needs to know what CTG is during pregnancy, but a specialist should decipher and evaluate the data obtained.
Preparation for the procedure
The study does not require special preparation. However, it is worth considering the duration of the procedure. It will be important for mom to relax and be calm. On the eve of the procedure, the pregnant woman is recommended to get a good night's sleep and rest. On the day of the study, you should take care of a light meal 1-2 hours before. And immediately before the procedure, go to the toilet. During CTG, the expectant mother should not be distracted or disturbed by anything. You can take a book or magazine with you, but electronic devices, including your phone, will have to be turned off, as the equipment creates interference with the recording.
In what cases is it done?
This method is used for early diagnosis of pathological conditions of the fetus. Starting from 28-30 weeks of pregnancy, the doctor at the antenatal clinic may prescribe you to monitor the fetal heartbeat using CTG.
1. CTG is recorded once, if nothing worries you and the doctor does not consider it necessary to record it.
2. With a pathological version of the recording. If the heartbeat is recorded with signs of pathology, the study will most likely have to be repeated.
3. In case of unfavorable course of previous pregnancies. If a woman’s obstetric history has dismal outcomes, then during the current pregnancy, even if it proceeds without any peculiarities, it will be necessary to record CTG more than once. For example: if a child died in the womb in the past, anomalies in the development of internal organs, genetic and chromosomal diseases.
4. In case of disturbances in the behavior of the unborn child. Every expectant mother feels and knows how her child behaves in the womb. Some children are very active and have very short periods of sleep. It happens that the child sleeps most of the day and is active at night. Changes in rhythms may be a sign that the fetus is experiencing discomfort.
5. When the mother herself is ill. For example, with influenza or ARVI, with acute conditions that lead to a deterioration in general well-being.
6. After the unborn child’s conditions have been suffered and treated. A CTG should be recorded for several weeks after inpatient or outpatient treatment.
7. When a woman has gestosis during pregnancy. This disease entails disturbances in the blood supply to the fetus, which can lead to delayed development of the unborn baby.
8. If a woman has a chronic infection.
9. Women who continue to smoke and drink alcohol during pregnancy. This group can also include women with drug addiction, including those in remission.
10. Women with chronic diseases of internal organs. For example, diabetes mellitus, arterial hypertension, heart defects, obesity, liver and kidney diseases.
11. Childbirth is most often carried out under heartbeat monitoring.
12. In case of post-term pregnancy.
Indications for the study
The purpose of cardiotocography is timely diagnosis and detection of fetal disorders. Based on data from a number of functional diagnostic studies, such as ultrasound, CTG, Doppler measurements, anamnesis, the obstetrician-gynecologist chooses pregnancy management tactics, treatment, the optimal date and method of delivery.
Indications for additional cardiotocography may include:
- Rhesus conflict
- Preeclampsia in the second half of pregnancy
- Maternal diseases
- Post-term pregnancy
- History of premature birth
- Fetal growth restriction
- Pregnancy pathologies and fetal development abnormalities identified by ultrasound
- Oligohydramnios or polyhydramnios
- Multiple pregnancy
- Complicated obstetric and gynecological history (previous abortions, miscarriages, premature births)
- Changes in the nature of fetal movements (complaints about a decrease or increase in the number of fetal movements per day)
What pathology can be diagnosed using CTG?
What exactly can be said from the data obtained? A final diagnosis cannot be made based solely on this method. Because any pathology and pathological rhythm can be a temporary response of the fetus’s body to an external stimulus or an administered drug, or even the mother’s mood. Therefore, remember, based only on CTG, it will be wrong to make a diagnosis. This method is simple and allows you to quickly and inexpensively suspect any condition in the unborn baby.
The following pathologies can be suspected using cardiotocography:
*Twisting or pressing the umbilical cord. These conditions can lead to disruptions in the supply of oxygen from the mother's body. At first, the fetus can compensate for the lack of nutrients, but if blood flow in the umbilical cord is not restored, this can lead to a serious condition;
* Rhythm disturbances in a child. Irrhythmic heartbeat can occur in the presence of cardiac developmental anomalies, even minor ones, such as accessory chords;
* With fetal hypoxia. The fetus may compensate for a long time and not show a lack of nutrients and there will be slight signs of deviation on CTG;
* During childbirth, this method allows you to quickly assess the condition of the fetus and all the changes that occur;
* For maternal diseases that may affect the condition of the fetus. In such cases, registration is made every day if the woman is in the hospital.
After the recording has been made and the doctor has suspected abnormalities in the CTG during pregnancy, if possible, the woman should undergo an ultrasound and Doppler ultrasound. In some cases, it is possible to carry out treatment and record a CTG again.
If the diagnosis is confirmed by ultrasound, then treatment is performed. CTG is recorded every day, and if necessary, 2 times a day.
Can there be errors when determining accelerations?
Of course yes! The indicators of the CTG curve are considered taking into account data from the anamnesis, clinical picture and other studies. A change in the functional activity of the fetal heart muscle is a response of the autonomic system, which only indirectly reflects the processes occurring in the body of a developing baby.
If, with insufficient oxygen supply, the fetal tissues have managed to adapt to this condition, hypoxia will not affect the study graph in any way. That is why practicing specialists consider CTG, although a very important technique for diagnosing pathologies of fetal development, but only an additional one. Its indicators reflect only part of the “mother-placenta-fetus” system and the results of cardiotocography alone do not make a diagnosis.
Is this method harmful to the fetus?
There are no studies that would prove that CTG is harmful to the fetus.
Some women note that when recording CTG, the child becomes restless or, on the contrary, “calms down.” Most likely, this is due to a new sound that the child hears or to a sensor, which is often fixed quite firmly on the stomach. All this causes discomfort in the child and can lead to unusual behavior.
When can a pathological variant appear in a healthy fetus?
1. During physiological pregnancy, a variant of pathology may appear.
2. If a woman has eaten too much before recording;
3. If the recording is made while the child is sleeping;
4. If the mother is obese. It is difficult to listen to the fetal heartbeat through the large subcutaneous fat;
5. The recording will not work if the child moves violently;
6. If there is no gel on the sensor or a poor fit, it will be difficult to hear the heartbeat;
7. During multiple pregnancy, it is difficult to record the heartbeat of all fetuses.
In these cases, the recording can be made again after some time.
Types of devices
All CTG devices (fetal monitors, cardiotocographs) can be divided into two large groups.
The first type includes devices that record only the heartbeat on tape and do not decipher its result. In this case, the resulting tape is analyzed by a doctor. The analysis depends on what period of pregnancy it was recorded. Decoding during childbirth is different from deciphering during pregnancy. During pregnancy, as a rule, the Fisher assessment is performed.
The second group of CTG devices records and deciphers this curve. But in order to understand the answer, you need to be well versed in all indicators.
How to decipher the resulting curve or data?
In order to decipher CTG, it is necessary to analyze the main parameters. Every pregnant woman saw a recording of the fetal heartbeat. This curve resembles an uneven fence, and looks different every time.
Decoding can be done using different methods, but more often during pregnancy the Fischer method is used:
Basal rhythm. This is the average fetal heart rate. Normal frequency is 119-159 beats per minute. Both a decrease and a rapid heartbeat are a sign that the fetus is experiencing hypoxia.
Amplitude or variability. These are fluctuations in heart rate. The baby’s heart contractions should not be monotonous, and on the CTG monitor you can see that the numbers change every second. Normally, vibrations should be 5-25 beats. A lower amplitude may indicate the child is sleeping or a pathological condition. A large difference between vibrations indicates a pathological condition of the fetus.
Frequency of changes. This parameter is easy to determine; you need to count the number of cloves in 1 minute. Normally there are 6-10 teeth.
Accelerations. This is an increase in the fetal heart rate that lasts from 0.5 to 1 minute. Typically, such increases in the basal rate are associated with fetal movement in the womb or uterine contractions. Acceleration is a normal reaction of the body, similar to the reaction of an adult to physical activity. Normally, there should be at least 2 such accelerations in 10 minutes.
Decelerations. This is a decrease in the fetal heartbeat, which, like acceleration, lasts 30-60 seconds. Decreases are a pathological response to fetal movements and contractions of the uterine muscle. And it may indicate an entanglement of the umbilical cord or other pathology. Normally there should be no reductions.
The doctor assigns a score from 0 to 2 to each sign. If there is a reading within the normal range, it is assigned 2 points, if higher or lower, then 1 point. In case of a critical decrease or increase, 0 points are given. The points are added up and deciphered as follows:
8-10 points is normal fetal condition. Everything is fine;
7-5 points indicates oxygen starvation. In this case, treatment is necessary, which will be aimed at improving uteroplacental blood flow. If possible, confirm the diagnosis using ultrasound;
A score of 4 or less indicates an acute condition; urgent confirmation of the diagnosis by ultrasound is necessary. Further actions are decided through a consultation.
If the device itself issues a response, the following response will be printed at the end of the recording:
Movements per hour - normally there should be 10 movements per day, but the device perceives all motor impulses, and there are a lot of them in one movement.
Signal loss – if signal loss is very frequent, then this will be one of the reasons for a long recording.
Basal rate (bpm) - the basal rate should be 120-160 beats per minute.
Abbreviations - will be shown if a sensor is attached that records contractions.
Accelerations >10 beats/min 15 sec-8 >15 beats/min 15 sec – the number of heart rate increases will be written here, normally more than 2
Low episodes (min) are decelerations. Normally, there should be no decelerations.
Variability – should be from 5 to 22 beats per minute.
Dawes/Redman criteria met to min. - This column will indicate how long the analysis lasted and at what point all the criteria for a normal heartbeat were met. The device records no more than 60 minutes; if the criteria are not met, this column will say that the criteria were not met by 60 minutes.
The result is not valid during childbirth, not a diagnosis - depending on the settings, the device will give a transcript during childbirth or during pregnancy
ULT-Zh 1cm/min. – this is the recording speed, which is adjusted by the doctor.
Pathological rhythms
There are a lot of pathological rhythms, but I would like to dwell on the two most common.
Monotonous rhythm - Observed if the fetus is sleeping or if there is a pathology in the supply of oxygen to the child. Let's imagine that an adult gets sick - most often a defensive reaction occurs, and most of the time he sleeps. Likewise, the fetus in the womb is in a sleepy state, and the heart beats monotonously.
Sinus rhythm is a record of slowdowns and accelerations. This picture can be seen if the fetus is constantly actively moving. If the fetus behaves calmly, and the recording looks like a sinusoid, this indicates a serious condition of the fetus.
You should not decipher CTG yourself. This should be done by a doctor, because only an obstetrician-gynecologist knows all the details and can make a correct diagnosis.
Fetal reactivity index and non-stress test
The first indicator reflects the state of the fetal nervous system in response to external influences. Such stressful situations primarily affect the state of the cardiovascular system. Points are used for calculation, where:
- 0 – complete absence of response to external stimulus.
- 1 – pronounced decrease in reactivity.
- 2 – noticeable decrease in reactivity.
- 3 – moderately expressed response to external influence.
- 4 – initial degree of pathological reactivity.
- 5 – adequate response to external influences.
Applying a warm or cold object to the pregnant woman's abdomen is used to assess fetal reactivity
A non-stress test is carried out to assess the state of the baby’s cardiovascular system during his voluntary movements. Normally, such a test should be negative, which implies the presence of 2 or 3 increases in heart rate by 15 beats, lasting no more than 20 seconds.
Despite the large number of indicators, cardiotocography is only an additional diagnostic method. For a comprehensive assessment of the condition of the mother and fetus, other instrumental examinations, laboratory test data and consultation with an experienced specialist are necessary.