Author: Strokina O.A., therapist, functional diagnostics doctor. April, 2021.
A patent foramen ovale is a minor anomaly of cardiac development. It is a hole in the central part of the interatrial septum. Normally, the window functions in the fetus. By the time the baby is one year old, it usually closes, but sometimes it remains for a longer period and even for life. You can suspect it at an early age in the clinic: blue discoloration of the nasolabial triangle with strong crying of the child, murmurs when listening to the heart. Diagnosed using echocardiography (ultrasound of the heart). Treatment does not require in the absence of pronounced clinical symptoms. If overload of the right side of the heart is detected, surgical treatment may be required.
Photo: mechanism of action of a patent oval window, author: Cleveland Clinic.
A patent foramen ovale is a normal communication between the atria of an unborn baby. It ensures his blood circulation. Thanks to this hole, placental blood, rich in oxygen, passes from the right atrium to the left and then through the ventricle goes to all organs and tissues. In most newborns it closes spontaneously. But according to some data, it remains in about 20% of adults.
A patent foramen ovale is not a heart defect, but a minor anomaly of its development (structural anomaly). Patients often confuse it with an atrial septal defect, which is precisely classified as a defect.
Many people also confuse a patent foramen ovale with a patent ductus arteriosus. These are 2 different pathologies. Patent ductus arteriosus is a congenital heart defect.
In ordinary life, a functioning open oval window is not dangerous. It can have unpleasant consequences, for example, in people who engage in strength activities: athletes in Greco-Roman wrestling, weightlifting, divers, loaders. With such loads, the pressure in the right chambers increases and blood is discharged from right to left, which leads to a sharp weakening of the body. When diving, this small anomaly can lead to death due to air embolism (with a sharp rise from the depths, air microbubbles in the blood combine into larger ones and through the oval window can enter the artery of the brain, heart and clog them).
Prevalence
A patent oval window is considered normal for up to 1 year. By this time, in children it closes. Further, we can consider the anomaly as a pathology. Less often, closure occurs by 3-5 years. The oval window can close at any age, but more often it occurs at the specified interval.
Among adults, a patent foramen ovale is relatively common. According to the largest study, based on autopsies of 90,000 people after death, a patent oval window occurs in 15-35% of people. Such data are quite consistent with the frequency of detection of anomalies during life using echocardiography: 15-25%.
What is this defect and what is its physiology?
An open foramen ovale in the heart of a newborn is a normal variant. What is it for? Blood circulation in the fetus starts at the beginning of the second trimester of pregnancy. Like an adult, a baby’s heart has four chambers:
- In the third week of intrauterine development, there is already a wall separating the atria - the primary interatrial septum (PAS) with a wide opening.
- In the fifth week of pregnancy, it overgrows, but a new one appears - a secondary one (opposite which an oval window is formed in the child’s heart), and another wall is formed to the right of the primordial septum.
- By the end of the seventh week, the primary MPP turns into a valve covering the oval window.
The fetus does not breathe, and its “point of gas exchange” is the placenta, therefore, the body does not need a pulmonary circulation. Instead it has:
- ductus arteriosus - a vessel connecting the aorta to the pulmonary artery;
- Foramen ovale is the opening between the ventricles.
The unborn baby receives oxygenated blood from the mother's placenta, from where it flows through the two umbilical arteries into the inferior vena cava. Venous blood from the baby’s internal organs also enters there. This mixed blood (arterial for the mother and venous for the fetus) flows into the right half of the heart.
The window between the atria is necessary for maximum blood flow into the left chambers of the heart, and then into the aorta. The remaining blood in the right atrium is sufficient to oxygenate the lung tissue.
How the pulmonary circulation turns on
With the first cry, when the mother's oxygenated arterial blood stops flowing, the newborn's carbon dioxide concentration increases. Vascular receptors “signal” about hypoxemia to the respiratory center of the brain. From there, the impulse goes to the skeletal muscles of the ribs, under the influence of which it expands. The pressure inside the chest cavity decreases, and a stream of air rushes into the lungs, thereby straightening them.
At the moment of the first breath:
- The pressure inside the left atrium increases significantly.
- The valve is pressed against the oval window.
- The communication between the atria is blocked.
- The flows of arterial (from the lungs) and venous (from the internal organs) blood no longer intersect.
Two circles of blood circulation begin to function. Subsequently, the septum secundum is fused to the wall of the heart. In most people, a fossa ovale forms at the site of the oval window.
Eustachian valve
The Eustachian valve (valvula venae cavae inferioris) is located at the level of the anterior arch of the inferior vena cava and, usually after the neonatal period, does not exceed one centimeter in length or is completely rudimentary. The valve is a fold of the endocardium with an average width of 1 cm. In the embryo, the valve directs a stream of blood from the vein to the foramen ovale. After birth, in the absence of communication between the atria, this valve function loses its significance. According to sectional data, the Eustachian valve is found in 86% of children.
In population studies using echocardiography, an unusually long Eustachian valve (more than 1 cm) is detected in 0.20% of the population and is considered a stigma (Fig. 161). According to our data, this small anomaly predisposes to supraventricular arrhythmias, probably reflexively due to irritation of the pacemaker formations of the atrium.
Fig. 161
Enlarged Eustachian valve of the inferior vena cava.
EchoCG criteria.
Two-dimensional echocardiography:
Visualization of a valve-like structure in the right atrium at the junction of the inferior vena cava.
Why doesn't the hole close?
If the closure of the interatrial communication is formed during the period of intrauterine development, such babies are born with serious dysfunctions of the cardiac and respiratory systems or die even before birth. In fact, an open foramen ovale in a child’s heart is an adaptive mechanism, and not a congenital anomaly.
In 50% of people, the valve fuses with the heart wall by the end of the twelfth month of life. If they do not heal before the age of two, cardiologists classify the condition as minor anomalies of the heart (MACD).
Distinctive features of MARS:
- there is no significant hemodynamic disturbance;
- symptoms are practically absent, and if present, they are not characterized by specificity.
25–30% of the adult population lives with an open foramen ovale. For some, the valve dimensions are insufficient to completely close the hole. The primary MPP may overlap the communication, but not fuse with the interatrial wall. If the pressure in the right side of the heart increases, the valve will open and some of the venous blood will flow through the ventricle into the aorta.
Experts believe that the main cause of MARS is genetic predisposition. The presence of connective tissue dysplasia in the mother significantly increases the likelihood of their occurrence. Risk factors for having a baby with a patent foramen ovale:
- smoking of the expectant mother;
- use of certain medications by a pregnant woman;
- adverse environmental influences.
Pediatricians note that in premature infants, an open foramen ovale is observed much more often than in babies born after the 36th week of gestation. In adults, the valve covering the opening between the atria may open:
- after excessive physical exertion, for example in athletes;
- if there is a history of decompression sickness;
- in people with thrombophlebitis after episodes of pulmonary embolism.
Sometimes the defect between the atria is combined with other, more serious heart anomalies.
Additional trabeculae in the left ventricular cavity
Can be single or multiple. Additional trabeculae are identified in 16% of autopsies.
EchoCG criteria
Two-dimensional echocardiography
- An echo-dense linear formation, detected in two sectional planes and having no connection with the valve apparatus.
- Using two perpendiculars in the long axis projection, drawn at the level of the papillary muscles and the free edges of the mitral valve, the cavity of the left ventricle is conventionally divided into three sections. The classification of trabeculae is based on the criterion of attachment of their ends to the walls of the left ventricle. If the attachment points are located in one section, then the trabecula is transverse, if in adjacent sections, then diagonal, and when the trabecula passes from the apical to the basal section, it is longitudinal.
Transverse localization of trabeculae of the left ventricle is interpreted as the most arrhythmogenic, since it can be an additional path of impulse conduction, and therefore can provoke premature ventricular excitation syndrome in the form of two variants: WPW syndrome and shortened PQ interval syndrome. Diagonal or longitudinal arrangement does not lead to disruption of the functional characteristics of the left ventricle, but is often accompanied by a systolic heart murmur, simulating a congenital heart defect.
Child's symptoms and behavior
In most cases, an unclosed foramen ovale in a child’s heart is not characterized by clinical manifestations. Parents may not even be aware of the existing feature. Further, in adolescence, the following are noted:
- decreased tolerance to physical activity;
- tendency to faint;
- breathing disorders.
Your doctor may suspect a patent foramen ovale in your baby if:
- pale skin;
- murmur on auscultation of the heart;
- periodically occurring cyanosis (cyanosis) of the nasolabial triangle in a child during outdoor games, screaming, coughing;
- if respiratory diseases “pursue” you much more often than other children;
- when your son or daughter is behind in growth compared to their peers;
- if the child complains of fatigue, dizziness, headaches, shortness of breath during exercise.
The discovery of varicose veins and thrombophlebitis in people under 30 years of age may also lead the doctor to think about a possible unclosed foramen ovale. A young child is not always able to accurately describe his condition, and a teenager, trying to appear older and more independent, sometimes tends to hide painful symptoms. Try not to delay visiting your doctor if there are even minor changes in your health.
Symptoms in children
- This can be manifested by frequent diseases of the lungs and bronchi.
- During periods of stress (crying, coughing, physical activity, attacks of bronchial asthma), the area of the nasolabial triangle becomes cyanotic and the lips turn blue.
- The child is somewhat behind in physical development and growth. Physical exercise causes fatigue and shortness of breath inadequate to the load.
- Spontaneous, unexplained fainting appears. This is especially true for young people with diseases of the veins of the lower extremities.
Diagnosis criteria
The International Classification of Diseases, 10th revision, recommends that atrial septal defect and patent foramen ovale be coded in a card using one code - Q 21.1. But in practice, doctors separate these two conditions (table below).
| Differences | Atrial septal defect | Patent foramen ovale |
| By pathogenesis | The hole may be caused by a violation of the formation of both primary and secondary septa | Rupture or insufficient size of the oval window valve |
| By localization | Can be located in any area | At the bottom of the fossa ovale, on the inside of the right atrium |
| According to anatomical features | Defect in the form of a hole | Has a valve structure |
| For hemodynamic disorders | Blood can flow from one atrium to another in both directions | Blood is shunted more often from right to left |
Ultrasound data
Cardiologists call echocardiography the “gold standard” for determining congenital heart anomalies. An ultrasound doctor judges the presence of an open foramen ovale using the following criteria:
- two-dimensional echocardiography: interruption of the signal from the septum at the location of the fossa ovale, gradual wedge-shaped thinning towards the edges of the defect, absence of volume overload of the right half of the heart, paradoxical movements of the barrier between the atria;
- Doppler echocardiography: turbulent blood flows at the location of the oval window, blood flow indicators in the right ventricle and pulmonary artery are normal.
Transesophageal echocardiographic examination is considered the most informative. But this type of diagnosis is only possible for adults or adolescents.
Mitral valve prolapse
Among ultrasound methods for diagnosing primary mitral valve prolapse, preference is given to two-dimensional echocardiography, since one-dimensional echocardiography results in a large number of false-positive and false-negative results. With two-dimensional echocardiography, it is necessary to measure the area of the atrioventricular valve and the circumference of the atrioventricular ring, which are significantly larger in children with mitral valve prolapse than in healthy ones. Sometimes it is possible to identify a violation of the architectonics of the valves, elongation, atypical attachment and incorrect distribution of the chords. The end-diastolic diameter of the left ventricle in children with primary mitral valve prolapse is reduced: in one third it corresponds to the 5th and in half to the 25th percentile. The combination of a reduced left ventricular cavity with an increase in the area of the mitral valve contributes to the occurrence of valvular-ventricular disproportion, which is one of the pathogenetic aspects of leaflet prolapse.
Additional examination methods
To determine patient management tactics, it is important to know how a hole in the interatrial septum affects heart function. Doctors do electrocardiography at rest and after exercise. This will help eliminate arrhythmia and conduction disturbances.
For adults, x-rays of the chest cavity are recommended, which will make it possible to judge the degree of hypertrophy of the right atrium and reveal congestion in the lungs.
Children with minor anomalies of heart development need consultation with a pulmonologist and immunologist. The presence of chronic foci of infections can aggravate the child’s condition, so you need to go to the otolaryngologist’s office or visit a dentist.
Functionally narrow aorta
EchoCG criteria:
- Aortic diameter value corresponding to the 3rd to 10th percentile of the normal population distribution.
- No significant pressure gradient between the aorta and left ventricle.
When studying the diameter of the aorta in children from 3 to 15 years old in the population, we found a wide range of variations in this size. In this segment of ontogenetic development, the lumen of the aorta increases 1.5-2 times. A comparison of echometric indicators of the aortic root in 1800 children aged 3-15 years revealed a relationship between aortic diameter and anthropometric indicators. Correlation analysis made it possible to detect a relationship between diameter and child height (r=0.872 for boys, r=0.634 for girls) and, to a lesser extent, with body weight (r=0.574 for boys, r=0.532 for girls) and body surface area. The aortic diameter value corresponding to the 3rd - 10th percentile was found in 5.6% of children; no dependence on the age of the children was identified. This fact excludes the influence of physiological periods of intensive growth in ontogenesis on the representation of this trait in the population under study. Our data allows us to conclude that a narrow aorta is a genetically determined or congenital minor anomaly of the heart. None of the children showed clinical and/or hemodynamic signs of stenosis. According to Doppler examination of blood flow in the ascending aorta, there was no diagnostically significant increase in the pressure gradient, which averaged 1.3+0.07 m/sec. Children with a functionally narrow aorta have a characteristic functional-structural organization of intracardiac hemodynamics, so in 91.2% of boys and 95.4% of girls, borderline values of the diameter of the right ventricle were identified, corresponding to the 90th - 97th percentile. Left ventricular end-diastolic diameter tended to increase (90-97 percentile) in children under 7 years of age, while in older children it corresponded to the 25 percentile. On the contrary, the transverse diameter of the left atrium in children under 7 years of age usually corresponded to the 25-75 percentile; at older ages it increased and, in most cases, exceeded the 75 percentile.
In most cases, in children with a functionally narrow aorta, an increase in the muscle mass of the left ventricle was detected, as evidenced by the values of the diastolic thickness of the posterior wall of the left ventricle and the interventricular septum, corresponding to the 90-97 percentile. Thickening of the interventricular septum was observed in 35.1% of boys and 34.1% of girls, and thickening of the posterior wall of the left ventricle in 80.7% of boys and 88.6% of girls. A combination of a functionally narrow aorta with other cardiac anomalies—mitral valve dysfunction (25.7%), mitral valve prolapse (8.9%), and additional trabeculae in the left ventricular cavity (10.8%)—was noted.
Children with borderline low values of aortic diameter are predisposed to the occurrence of supraventricular and ventricular arrhythmias, as well as insufficient performance and exercise tolerance.
Possible complications
Most parents and pediatricians rightly believe that the presence of an open oval window does not threaten the child’s health. This opinion is supported by the statement of a popular pediatrician, Evgeniy Olegovich Komarovsky: this condition is not a malformation of the heart. Indeed, with a small hole, a person can play sports, work and study, and young men are even subject to conscription for military service.
But under certain conditions, a patent foramen ovale can cause the following unfavorable conditions in adults:
- Paradoxical venous embolism is the entry of a microthromb, a bubble of fat or air from the venous system into the left atrium, and then its penetration into the systemic circulation. This condition can provoke a transient ischemic attack or stroke.
- Migraine with a patent foramen ovale often occurs with an aura. It usually occurs in older women when blood is shunted from right to left.
- Platypnea-orthodeoxia is a syndrome characterized by shortness of breath that occurs when standing and subsides when lying down. It is usually observed when a patent foramen ovale is combined with deformation of the IV.
- Obstructive sleep apnea syndrome.
Some people with a patent foramen ovale develop transient global amnesia after a migraine or ischemic attack - a syndrome of memory impairment and inability to perceive new information.
Idiopathic dilatation of the pulmonary artery
It is characterized by an expansion of the trunk in the absence of heart disease and pulmonary pathology. Dilatation of the pulmonary artery trunk occurs against the background of hereditarily determined connective tissue pathology, which is confirmed by the simultaneous detection of other markers of connective tissue dysplasia of the heart and the frequent detection of dilation in hereditarily determined syndromes, for example, Marfan syndrome. Auscultation can detect a systolic murmur of moderate intensity at the base of the heart, which decreases with an upright position. With idiopathic dilatation of the pulmonary artery, dynamic observation and examination is necessary.
Treatment
Holes with a diameter of 4 - 5 mm have a high chance of closing on their own. Approaches to the treatment of an open foramen ovale are individual and depend not only on the size of the defect, but also on the presence of increased pressure in the pulmonary trunk, the degree of myocardial hyperplasia, and the risk of complications.
For children with no clinical manifestations and stable defect sizes, drug therapy is not indicated.
If your child is diagnosed with a patent foramen ovale, he or she needs periodic examinations by a cardiologist.
What can happen to the oval window during life:
- closure;
- maintaining constant dimensions;
- expansion of the defect as they grow older.
Some parents give their children vitamin complexes and dietary supplements and resort to herbal treatment, but the effectiveness of such therapy has not been proven.
Indications for surgical correction of communication between the atria:
- signs of overload of the right atrium and ventricle;
- the occurrence of heart failure;
- presence of complications.
Transcatheter closure of the hole in the interatrial septum is performed. An occluder is passed to the human heart through large vessels using a catheter (see photo below), which plays the role of a patch. The manipulation is performed under X-ray and ultrasound control.
For preventive purposes, the operation is not indicated even for people of certain professions, although the available data from the medical literature confirm that performing transcatheter occlusion can help prevent decompression sickness in divers.
It is worth mentioning the possible adverse consequences of the intervention:
- embolization with occluder;
- infectious complications;
- erosion of the aorta or pericardium;
- atrial fibrillation;
- occluder thrombosis;
- the emergence of a new MPP defect.
Late complications of the transcatheter procedure include the occurrence of a residual shunt (residual discharge of blood into the left atrium) and the formation of a blood clot on the occluder. You should carefully discuss with your doctor all the pros and cons of surgical correction of the defect. Closing the oval window significantly improved the condition of patients with migraine, platypnea-orthodeoxia syndrome, and helped prevent recurrent ischemic strokes in adults. At the same time, pediatric cardiologists do not recommend surgical elimination of the IV defect in infants, considering the optimal age for radical correction to be from 2 to 5 years.
Subvalvular apparatus of atrioventricular valves
The significance of these microanomalies is not fully understood. Typically, these abnormalities in childhood do not cause valvular regurgitation and/or obstruction of blood flow and are manifested only by a functional systolic murmur, sometimes simulating congenital heart disease. Whether microabnormalities of the chordae and papillary muscles predispose to the onset of valve insufficiency in adulthood is not fully understood. These anomalies are likely to predispose to rheumatic and infective endocarditis, as well as mitral valve prolapse in children and, as a consequence, atrioventricular valve insufficiency in adults. The subvalvular apparatus of the left atrioventricular valve has a wide variety of structure (Fig. 158).
Fig. 158
Anomaly in the structure of the papillary muscles: one papillary muscle located in the apical region, the obturator function of the valve is not impaired.
Most often in childhood, impaired distribution of the chords to the anterior or posterior leaflet of the mitral valve occurs.
Disturbed distribution of chords to the anterior (posterior) leaflet of the mitral valve
EchoCG criteria
One-dimensional echocardiography:
- Increased diastolic excursion of the anterior mitral leaflet.
- Additional echoes from tendon formations in the left ventricular outflow tract during systole.
Two-dimensional echocardiography
- On an echocardiogram, tendon echoes from the anterior (posterior) leaflet are predominantly oriented in the center or at the base.
- There are no manifestations of mitral regurgitation (dilatation of the left atrium and ventricle).
Doppler EchoCG
There is no significant pressure gradient between the left atrium and the left ventricle, as well as the left ventricle and the aorta.
Patent foramen ovale in an adult
There is a high likelihood of ischemic stroke in young women with a patent foramen ovale who suffer from migraines.
In adults, after examination and ultrasound, cardiologists note the following risk factors for complications:
- dimensions of the oval window – more than 4 mm;
- tension of the interatrial septum during the Valsava maneuver;
- shunting even a small amount of blood to the left;
Sometimes doctors prescribe anticoagulants and antiplatelet agents to prevent the development of stroke and other thromboembolic complications.
Causes and risk factors
The main cause of patent oval window is a genetic factor. Most often, the anomaly occurs in people with a predisposition to connective tissue dysplasia, which is inherited. Therefore, in addition to the oval window, people often experience mitral valve prolapse.
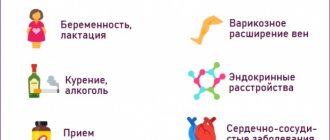
There are other reasons and risk factors for the development of an open oval window:
- taking non-steroidal anti-inflammatory drugs (diclofenac, ibuprofen, nimesulide, etc.) during pregnancy, especially in late gestation (pregnancy);
- alcohol and nicotine consumption during pregnancy;
- premature birth.